Imaging cartilage and subchondral bones
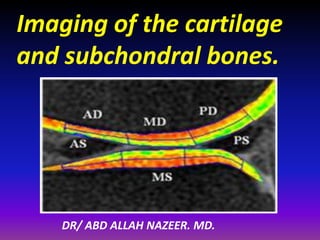
- 1. Imaging of the cartilage and subchondral bones. DR/ ABD ALLAH NAZEER. MD.
- 3. Articular cartilage. Definition: The cartilage covering the articular surfaces of the bones forming a synovial joint. Also called arthrodial cartilage, diarthrodial cartilage, investing cartilage. Articular cartilage. A type of hyaline connective tissue that covers the articulating surfaces of bones within synovial joints. Cartilage. A specialized, fibrous connective tissue present in adults, and forming most of the temporary skeleton in the embryo, providing a model in which most of the bones develop, and constituting an important part of the organism's growth mechanism; the three most important types are hyaline cartilage, elastic cartilage, and fibrocartilage. Also, a general term for a mass of such tissue in a particular site in the body.
- 4. CARTILAGE: • CHONDROCYTES: (1‐2%) • EXTRACELLULAR MATRIX: • Solid. Proteoglycans (15%). Collagens‐Type II (15‐20%). • Fluid. Water (70‐80%). Proteoglycan: • draws water & maintains osmotic pressure • counteracts swelling pressures • provides force in tension & shear • resists compression
- 7. Imaging modalities of articular cartilage disease. Radiography have been the traditional imaging modality used to evaluate patients with acute cartilage injury. However radiograph can only assess joint space loss(Indirect imaging of cartilage) and osteophytic formation and are insensitive for early cartilage degeneration. Ultrasound. Arthrography and CT arthrography. For this reason MRI is has become the imaging modality of choice for evaluating articular cartilage, especially T2 mapping. Because of its high resolution, multiplaner capabilities and excellent tissue contrast, MRI can detect and characterize morphologic changes associated with cartilage degeneration and acute cartilage injury. Lack of exposure to ionizing radiation is an additional attractive feature of MR imaging particularly in young patients. Detecting biochemical or functional changes in cartilage is desirable.
- 9. Ultrasound. Visualization in multiple planes. Real time, dynamic assessment. No radiation and in expensive. But, no visualization of deep articular cartilage. Low contrast between cartilage and fluid. Low negative predictive value.
- 10. OA of the knee. Coronal ultrasound scans through the distal femur of a normal knee (A) and an osteoarthritic knee (B) demonstrate the intracondylar notch. The red arrows indicate the cortical surface of the femur, and the yellow arrows indicate the superficial surface of the cartilage. Note that compared with the normal knee, the cartilage in the osteoarthritic knee is more echoic, there is loss of definition of the margins, and it appears thinner laterally.
- 11. CT-Arthrography. Tomographic technique : High spatial resolution. Multiplaner capability. Acute traumatic injury. More available than MRI. Excellent to depict superficial cartilage damage. (probably superior to MRI). But: Invasive. Very poor assessment for other articular structures. No well validated for early intra-substance changes.
- 12. Correlation of CT arthrography and MR imaging. (A) Sagittal reformatted CT arthrography of the medial knee compartment shows posterior horn meniscal tear (arrow). Note superficial cartilage thinning at the femoral condyle adjacent to the meniscus. (B) Sagittal proton density-weighted MR image of the same knee demonstrates the posterior horn meniscal tear (arrow). (C) Coronal reformatted CT arthrography of the medial compartment shows focal cartilage defect in the central femoral condyle (arrow). (D) Coronal fat- suppressed T2-weighted MR image shows the same defect (arrow).
- 13. Focal cartilage defect at CT arthrography and MRI Fat sat images.
- 22. The International Cartilage Repair Society has set up an arthroscopic grading system by which cartilage defects can be ranked: grade 0: (normal) healthy cartilage grade 1: the cartilage has a soft spot or blisters grade 2: minor tears visible in the cartilage grade 3: lesions have deep crevices (more than 50% of cartilage layer) grade 4: the cartilage tear exposes the underlying (subchondral) bone.
- 23. Chondromalacia can be divided into 4 grades by MRI, typically using fat saturated proton density sequences. This grading system is the modified outer bridge grading system, which was devised for arthroscopy initially for assessment of chondromalacia patella, but then modified and extended for all chondral surfaces. grade I. Focal areas of hyperintensity with normal contour arthroscopically : softening or swelling of cartilage. grade II. Blister-like swelling/ fraying of articular cartilage extending to surface arthroscopically : fragmentation and fissuring within soft areas of articular cartilage. grade III. Partial thickness cartilage loss with focal ulceration arthroscopically : partial thickness cartilage loss with fibrillation (crab- meat appearance). grade IV. Full thickness cartilage loss with underlying bone reactive changes arthroscopically : cartilage destruction with exposed subchondral bone.
- 29. dGEMRIC • Assesses early cartilage damage as GAG loss prior to development of macroscopic cartilage Defects. • Negatively charged MRI contrast (Gadolinium; Gd), (IV or intra‐articular) is repelled by negatively charged GAG. Less GAG in cartilage less negative charge relative to normal cartilage. The more the negatively charged contrast will penetrate GAG deplete cartilage. • Gd penetrates normal cartilage, high [GAG], in a reciprocal manner.
- 30. ↑ Gd ↓ T1 value (MRI property of Gd) • Double negative: ↓*GAG+ = ↑Gd = ↓ T1 ↑*GAG+ = ↓Gd = ↑T1 • *GAG+ is directly proportional to T1 value • T1 value = T1 relaxation =me = dGEMRIC index.
- 31. TECHNIQUE: • IV Gd – double dose. • Exercise. • Wait 30‐90min for penetration. • IA be over than IV. • T1 maps of cartilage. generated/manually plotted. • No difference between 1.5T & 3T (5).
- 32. VALIDATION. • Reproducible. • Excellent in vitro Correlation. • Higher dGEMRIC index (less Gd , higher [GAG]) = higher resistance to mechanical compression.
- 33. INTERPRETATION. MARATHON BEFORE 1 DAY 1 WEEK
- 34. Color-coded T1ρ map overlays on SPGR images in the posterior femoral cartilage. (a) a healthy volunteer, male, 30; (b) a patient with early OA, female, 27. The T1ρ values were 40.05±11.43 ms in the volunteer and 50.56±19.26 ms in the patient, respectively.
- 36. Case study of dGEMRIC as a function of time before and after PCL injury. A decline in the dGEMRIC Index is apparent at one month, with a further decrease at three months and recovery at six months. These data illustrate the potential for biochemical monitoring of cartilage to demonstrate degeneration and recovery of the tissue from a traumatic injury. Similar studies might be used to monitor cartilage status improvement with other mechanical, surgical, or pharmaceutical interventions. (From Young AA, Stanwell P, Williams A, et al. Glycosaminoglycan content of knee cartilage following posterior cruciate ligament rupture demonstrated by delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC).
- 49. Mild diffuse increased intra-substance signal within morphologically normal cartilage.
- 50. Transverse T2 weighted MR of patella. Blister is seen at surface of cartilage (arrow) suggestive of grade 2 chondropathy. Transverse T2 weighted MR of patella. Crabmeat appearance is apparent (arrow) compatible with grade 2 chondropathy.
- 51. Thinning, fissuring or fibrillation involving depth < 50% over small area.
- 53. Transverse T2 weighted MR of patella. Focal ulceration is seen (arrow) Grade 3 chondropathy.
- 54. Transverse (T2 fat sat) weighted MR of patella. Focal ulceration is seen (arrow) Grade 3 chondropathy.
- 55. Thinning, fissuring or fibrillation involving depth > 50% over large area.
- 56. Transverse CT arthrographic image. several patellar fissures are seen extending to subchondral bone, compatible with grade 4 chondropathy. Transverse proton density weighted MR with FS of patella. Fissures are seen (thin arrows) extending to subchondral bone compatible with grade 4 chondropathy. Patchy subchondral edema is also evident (bold white arrow).
- 57. Full thickness chondral lesion , exposed subchondral bone.
- 62. Subchondral bone. Various changes may be seen in the subchondral bone, and are often associated with cartilage changes. Subchondral bony changes can be described in more detail by grading MR changes according to signal intensity or by assessment from a morphological pattern. MR signal intensities usually are compatible either with edematous changes or with sclerotic changes. A small sclerotic focus of subchondral thickening of the Cortex or a subchondral semilunar area is commonly seen in degenerative disease. A cortical impaction, bowing fracture or a subchondral branching fracture line can be seen in trauma and may be accompanied by bone marrow edema. Geodes or cysts may be seen in degenerative disease . Bone marrow edema is non-specific and can be seen in degenerative disease or traumatic injury . Osteophytes are a clear indication of degenerative disease.
- 64. Patterns of subchondral changes 1. Focally thickened cortical line (arrow). 2. Focal semilunar subchondral change (arrow). 3. Focal impaction (arrow). 4. “Bowing” fracture (arrow). 5. Cyst (arrow). 6. Edema (arrow). 7. Diffuse linear branching changes (arrow). 8. Osteophyte (arrow).
- 65. Sagittal STIR weighted MR. Subchondral patchy high signal intensity consistent with edema (arrow) following ankle trauma.
- 66. T1 weighted MR (A) and STIR weighted MR (B) in tibial plateau specimen. Thinning of cartilage is seen in A (white bold arrows) associated with subchondral semilunar-shaped very low signal intensity (black arrows), and larger area of mildly lowered signal intensity. In B larger area revels diffuse patchy high signal intensity compatible with “edema”(arrow) surrounding the semilunar area.
- 67. Coronal T1 weighted MR in knee trauma. Focal thickening of cortical line (black arrow) and larger area of patchy subchondral changes (white arrows). Note that this appearance could also be seen in avascular necrosis.
- 68. Sagittal T2 weighted MR obtained following meniscectomy. In A (initially) meniscal remnant is apparent (arrowhead),as well as diffuse patchy subchondral changes (arrows).In (follow-up) B cortical impaction is seen (curved arrow) and semilunar subchondral change (arrow).
- 69. Sagittal T2 weighted MR image. Note linear band of subchondral edema (long arrow) and deeper foci of branching subchondral changes (short arrows).
- 70. Sagittal proton density weighted MR. Abnormal concavity of lateral tibial plateau is seen (arrows) compatible with “bowing” fracture.
- 71. Transverse T2 weighted MR with FS. Marginal (bold arrows) and central osteophytes (long thin arrow) are evident.
- 72. Coronally reconstructed CT image of ankle. Subchondral cysts (arrows) and cartilage defect (arrowhead) are seen after ankle trauma.
- 73. Sagittal fat saturated T2. Degenerative disease with severe cartilage thinning is apparent (arrows). Note subchondral edema (short arrow).
- 75. Osteochondroma: Most common benign skeletal tumor 20-50% of all benign bone tumors. Most frequent in 1 1st and 2nd decade of life Male : female = 1.5 : 1. Most often in juxta -epiphyseal / metaphaseal. area of long bones (distal femur, proximal tibia) 40% around the knee (also shoulder, hip).
- 76. Ostechondroma: Bony exostosis with cartilage cap. Typically grow away from physis. Growth ceases after maturity. Growth after maturity indicates malignant transformation. < 1% risk of malignant transformation for solitary lesions. Clinical Presentation. Painless bony mass. Can be painful if mechanical irritation (nerves, vessels, muscles, tendons, bones). Fracture. Bursa formation.
- 77. Radiographic Appearance: Diagnostic Sessile or stalk -like (exostosis). Metaphyseal bone may be expanded and remodeled. Cartilage cap may be calcified. Base of lesion contiguous with cortex of bone.
- 78. Exostosis.
- 80. Enchondroma. Solitary, benign, intramedullary cartilage forming tumor Peak incidence in 3 3rd rd decade Male : female = 1 : 1 Common in short tubular bones of hands and feet Most common primary tumor in the hand, usually in the diaphysis.
- 81. Clinical Presentation. Hand > Foot lesions more commonly active. Cortical bone erosion resulting in pain, bony mass, or pathologic fracture. Expansile lesions may cause palpable bony mass Found incidentally in long bone . < 1% risk of malignant transformation< transformation. Radiographic Appearance. Long bones. Metadiaphysis. Most common in femur and humerus. Tubular bone Diaphysis Matrix – “popcorn ” “comma shaped ” “stippled” calcification.
- 82. Enchondroma.
- 83. Chondroblastoma. Rare, benign tumor derived from chondroblasts (5% of benign bone tumors) Epiphysis of long bones (also apophyseal Most common sites Femur, humerus, tibia apophyseal) . Male : female = 3 : 2 Mean age: skeletally immature May have behavior not normally associated with benign tumors (pulmonary metastases, local bone / soft tissue invasion).
- 84. Clinical Presentation. Pain near a joint without history of trauma Tumor can induce a secondary synovitis Patient may have a joint effusion Pathological fracture rare. Radiographic Appearance: Lytic well-defined margins Scalloping or erosion of cortical bone may be present Fine calcifications (punctate , rings).
- 85. Chondroblastoma.
- 86. Chondrosarcoma: Malignant tumor that produces cartilage matrix Primary chondrosarcoma Very uncommon, arises centrally in bone, found in children found children Secondary chondrosarcoma Secondary Arises from benign cartilage defects (osteochondroma – surface , enchondroma - Intra-medullary). Clinical Presentation. Pain. Enlarging mass.
- 87. Chondrosarcoma. Occurs in 5th or 6th decade of life. Male : female = 1.5 : 1 Location: femur, humerus, ribs, pelvis Higher risk to occur in patients with Ollier disease and Maffucci Syndrome (3rd rd or 4th decade of life).
- 88. Chondrosarcoma.
