Respiratory condition
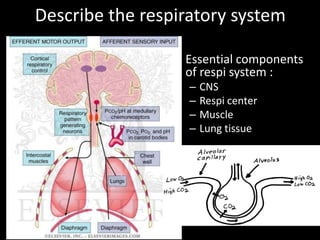
- 1. Describe the respiratory system • Essential components of respi system : – CNS – Respi center – Muscle – Lung tissue
- 2. Depict signs of respiratory distress in a real patient
- 3. Respiratory distress • It is an abnormal physiologic condition identified by increased work of breathing. • The child in respiratory distress is effectively compensating to preserve adequate gas exchange.
- 5. Signs of Respiratory distress • Tachypnea • Tachycardia • Retractions (supraclavicular, suprasternal, intercostal or subcostal) • Use of accessory neck muscles • Nasal flaring and grunting • Pallor or cyanosis • Altered mental status (restlessness, irritability, confusion, anxiety, inability to recognize parents)
- 6. Positioning • With an upper airway obstruction, the patient characteristically assumes sniffing position (jaw thrust forward) and may drool due to inability to swallow secretions. • A patient in severe respiratory distress may position himself in the tripod position (seated and leaning forward on outstretched arms), sitting upright and leaning forward to maximize use of accessory muscles.
- 7. Respiratory rate • Abnormal respiratory rate is common finding in respiratory distress. • Although normal respiratory rate varies with age, a rate greater than 60 breaths per minute is abnormal in any child. • A slow respiratory rate might arise concerns as it may signifies respiratory fatigue and imminent respiratory arrest in an exhausted child.
- 8. Retractions • Subcostal, intercostal and suprasternal retractions are manifestations of increased work of breathing as well as use of accessory muscles of respiration. • Paradoxic breathing (abdomen retracts upon inspiration and expands upon expiration) may be noted.
- 9. Nasal flaring and grunting • Flaring of the nostrils with inspiration is also a sign of respiratory distress. • Grunting is a sound made by forceful expiration against a partially closed glottis. • Head bobbing may be seen in infants.
- 10. Lung Sounds and Auscultation • Decreased breath sounds and diminished air entry in the setting of increased respiratory effort suggest worsening respiratory disease.
- 11. Heart Rate • Tachycardia is a common finding in children in respiratory distress and is not necessarily indicative of cardiovascular instability. • Bradycardia, for instance, is indicative of severe hypoxemia and acidosis which require critical interventions. • Bradycardia in a child with history of respiratory distress signifies imminent cardiopulmonary arrest.
- 12. Altered level of consciousness • Some children might present with effortless tachypnea resulting from an increased respiratory drive caused by metabolic acidosis or central nervous system disease. • Therefore, mental status is evaluated as a gauge of systemic oxygenation and critical management must be done if the patient appears lethargic or agitated.
- 13. Normal Respiratory Rate • Infant = 30 – 40 /min • Toddler = 24 – 40 /min • School age = 18 – 30 /min • Adolescent = 12 – 16 / min
- 14. Define respiratory failure • Respiratory failure is a syndrome of inadequate gas exchange due to dysfunction of one or more essential components of the respiratory system: • Type I : Hypoxaemic respiratory failure. PaO2 < 60 mm Hg with a normal or low PaCO2. This is caused by ventilation- perfusion mismatch with either/both: – Under-ventilated alveoli (eg pulmonary oedema, pneumonia or acute asthma). – Venous blood bypasses ventilated alveoli (eg right to left cardiac shunts). • Type II : Hypercapnic respiratory failure. PaCO2 > 50 mm Hg and indicates inadequate alveolar ventilation. Any ventilation-perfusion mismatch will affect PaO2 and therefore hypoxaemia is also common.
- 15. • Common causes of type • Common causes of type I respiratory failure II respiratory failure – COPD. – Drug – Pneumonia. overdose, poisoning. – Pulmonary oedema. – Myasthenia gravis. – Pulmonary fibrosis. – Polyneuropathy. – Asthma. – Poliomyelitis. – Pneumothorax. – Muscle disorders. – Pulmonary embolism. – Head injuries and neck – Pulmonary hypertension. injuries. – Cyanotic congenital heart – Hypothyroidism. disease. – Bronchiectasis. – Acute respiratory distress syndrome.
- 16. Ix : • Arterial blood gas analysis: confirmation of the diagnosis. • CXR: often identifies the cause of respiratory failure. • FBC: anaemia can contribute to tissue hypoxia; polycythaemia may indicate chronic hypoxaemic respiratory failure. • Renal function tests and LFTs: may provide clues to the aetiology or identify complications associated with respiratory failure. Abnormalities in electrolytes such as potassium, magnesium, and phosphate may aggravate respiratory failure and other organ dysfunction. • Serum creatine kinase and troponin I: to help exclude recent myocardial infarction. Elevated creatine kinase may also indicate myositis. • TFTs (hypothyroidism may cause chronic hypercapnic respiratory failure). • Spirometry: useful in the evaluation of chronic respiratory failure. • Echocardiography: if a cardiac cause of acute respiratory failure is suspected. • Pulmonary function tests are useful in the evaluation of chronic respiratory failure. • ECG: to evaluate a cardiovascular cause; it may also detect dysrhythmias resulting from severe hypoxaemia or acidosis.
- 17. Management • A patient with acute respiratory failure generally needs prompt hospital admission in an intensive care unit. • Many patients with chronic respiratory failure can be treated at home, depending on the severity of respiratory failure, underlying cause, comorbidities and social circumstances. • Immediate resuscitation may be required. • Appropriate management of the underlying cause.
- 18. Describe obstructive and restrictive respiratory conditions
- 19. Obstructive disorders • These are respiratory disease which make it more difficult to get air out of the lungs. • This group of disorders is characterized by obstruction of normal airflow due to airway narrowing and includes: Asthma, COPD, bronchiectasis, cystic fibrosis and tumors. • Mechanisms causing airway narrowing differ and may include obstruction by a mucus plug, airway compression and smooth muscle constriction.
- 20. Obstructive disorders • In general, obstructive disorders lead to hyperinflation of the lungs as air is trapped behind closed airways. • Residual volume is increased as in the ratio of RV: TLC. Functional residual capacity also increased. • In patients with severe obstruction, air trapping is so extensive that vital capacity is decreased.
- 21. • In addition, dynamic compression of the airway prolongs the FEV1, as well as the forced expiratory flow rate measured over the middle half of expiration (FEF 25-75%) • Both FEV1 and FVC are reduced, but the reduction in FEV1 is greater (airway narrowing reduces the speed of forced expiration such that FEV1 is reduced to an abnormally low fraction of FVC, perhaps to 40% or lower). • Result: low FEV1 / FVC.
- 22. Obstructive disorders • Extrathoracic- stridor • Intrathoracic- wheezing, best heard during expiration • Long deep breaths • Hyperinflated and tympanitic to percussion
- 23. Bronchoconstriction causes obstructive airway problems
- 26. Restrictive disorders • These are respiratory disease which makes it more difficult to get air into the lungs. • They “restrict” inspiration. • Examples include: Fibrosis, sarcoidosis, silicosis, asbestosis, muscular diseases and chest wall deformities.
- 27. Restrictive disorders • In fibrosis or alveolar wall thickening, the increased connective tissue reduces lung compliance, making it difficult to expand the lung during inspiration. • In condition such as alveolar edema, respiratory distress syndrome, or infiltrative interstitial lung diseases, the lungs are stiff decreasing its compliance. • Extrapulmonary factors that can contribute to decrease vital capacity include limited thoracic expansion (Pleural fibrosis, Kyphoscoliosis) and nerve or muscular dysfunction.
- 28. • As a result, all lung volumes are reduced. In particular, there can be marked decreases in total lung capacity and functional vital capacity. • FEV1 and FVC are reduced proportionately but the normal ratio is preserve. • The patient might demonstrate rapid shallow breathing. He/she might also shows grunting. • Percussion of the respiratory system demonstrate dull/ hyper-resonance?
- 32. Differentiate clinical presentation of obstructive airway Upper airways obstruction Lower airways obstruction Stridor Wheezing • harsh sound •Continuous expiratory sound •Produced near larynx by the vibration of •Due to turbulence airflow upper airway structures •Musical •Inspiratory ( expiratory – less common) •Partial obstruction produces wheezing •hoarseness – effect vocal chord sound at later phase of expiration •Supraglottic etiology – moves with child’s •Harsh, monophonic and low pitch (usually head from large, central airways) •Decreases while sleep – inspiration at lower • high pitched and musical (from small and rate during sleeping peripheral airways) Suprasternal retraction Rhonchi •Pressure gradient between trachea and •Secretion in intrathoracic airways, resulting atmosphere in irregular sound Rales or crackles •Sound characterized by of crumpling celophane due to fluid or secretion in small airways
- 33. Describe conditions presented with wheezing in children and infants • Acute wheezing : – Infection – Foreign body aspiration (FBA) • Chronic/ recurrent wheezing – Anomalies of the tracheobronchial tree (ie Congenital tracheomalacia and bronchomalacia) – Cardiovascular disease (pulmonary artery dilation and/or left atrial enlargement, including large left to right shunts, can compress large airways and cause wheezing) – Mediastinal masses (ie tumors, cyst, LN enlargement)
- 34. Upper respiratory tract conditions - to be presented in tabulated manner • common cold • acute pharyngitis • acute otitis media • acute sinusitis
- 35. common cold acute pharyngitis acute otitis media acute sinusitis Fever Inflamed pharynx and fever, Cough Nasal discharge soft palate irritability, Nasal symptoms Loss of appetite Enlarged and tender headache, Fever Difficulty sleeping. LN apathy, Headache anorexia, Facial pain and vomiting, swelling diarrhea Sore throat Rhinovirus, Adenovirus RSV, rhinovirus, Rhinovirus, coronavirus, RSV Enterovirus Pneumococcus, adenovirus, influenza, Rhinovirus H. influenzae or parainfluenza Gp A β-hemolytic strepto Treat fever and pain Paracetamol Paracetamol Nebulized anti- with paracetamol or Penicillin (bact only) Ibuprofen microbials ibuprofen
- 36. Pnuemococal Staphylococcus Mycoplasma Viral pneumonia pneumonia pneumonia pneumonia S. Pneumoniae Staphylococcus Mycoplasma Influenza virus aureus pnuemoniae Parainfluenza virus Community acquires Presentation Presentation Presentation •Skin infection •Fever •Fever •Soft tissue •Malaise •Chills infection – •Headche •Non productive pyomyositis, septic •Persistent slowly cough bursitis worsening dry •Rhinitis •Toxic shock cough •Myalgias syndrome •Chills •Headache •Endocarditis •Sore throat •fatigue •Osteromyelitis •Pluertictic chest •Pneumonia pain •Food poisoning •UTI Tx Tx Antibiotics amantindine, Antibiotics Antimicrobial Macrolides, rimantidine, therapy doxycyline acylovir
- 37. Pertussis – whooping cough Etiology Caused by Bordetella pertussis Infect among human through respiratory droplets (coughing) Clinical presentation Infants beyond neonatal period through school age Catarrhal stage – injection, increased nasal secretion and low grade fever 1-2 weeks Paroxysmal stage – coughing (expiration) to dislodge plugs of necrotic bronchial epithelial tissues and thick mucus. Lasted 2-4 weeks Followed by forceful inhalation against narrowed glottis – whoop characteristic Convalescent stage – symptom gradually resolve 1-2 weeks, coughing less severe, whooping cough dissapear. CNS damage due to hypoxia, bacterial pnuemonia, Adult – starts with broncholitis illness. Tx Erythromycin – early coarse, eradicates nasopharyngeal carriage within 3-4days, ameliorate the effects of infection, ineffective at paroxysmal stage, , ass with pyloric stenosis if given to neonates <4 weeks old Azithromycin & clarithromycin – shorter duration, ass with gastrointestinal adverse effects Pertussis-specific immunoglobin – effectivelt reduced symptoms at paroxysmal stage TMP-SMZ (trimethoprim/sulfamethozxazole)
- 38. Pulmonary tuberculosis Etiology Caused by Mycobacterium tuberculosis Spread via respiratory droplets – become respiratory nuclei, <10um can reach alveoli Clincal manifestation •Asymptomatic in older and infants patient •+ve tuberculin skin test •Minimal abnormalities on CXR infiltration with hilar lymphadenopathy (Ghon complex) •Malaise, low grade fever, erythema nodosum, lympahadenopathy symptoms. Investigation Tuberculin skin test (TST) •T-cell-mediated hypersensitivity, 2-6 weeks Mantoux test •Intradermal injection of 5TU on volar surface of forearm, screen high-risk population and for diagnosis in all ill patients or contacts. •False –ve at early phase of illness or immunosuppression Culture Tissue, sputum, fluid Treatment Antibiotics – RIPES, 9-months of isoniazid&rifampin 98% case cured Prevention - BCG
- 39. • Acute viral bronchiolitis • transient infant wheeze • chronic lung diseases of prematurity • bronchiectasis.
- 40. Acute viral bronchiolitis • lower respiratory tract infection (LRTI) that primarily affects the small airways (bronchioles) – RSV is the most common cause, followed by rhinovirus – Less common causes include parainfluenza virus, human metapneumovirus, influenza virus, adenovirus, coronavirus,
- 41. • S/s : fever (usually ≤38.3ºC), cough, mild respiratory distress, preceded by a one- to three- day history of upper respiratory tract symptoms, such as nasal congestion and/or discharge. • PE : – tachypnea – intercostal and subcostal retractions, often with expiratory wheezing. – The chest may appear hyperexpanded with increased anteroposterior (AP) diameter and may be hyperresonant to percussion. – Findings on auscultation include any combination of expiratory wheeze, prolonged expiratory phase, and both coarse and fine crackles. • Ix : Mild hypoxemia (oxygen saturation <95 percent) commonly is detected by pulse oximetry, even without clinical signs of desaturation
- 42. • Mx : – SEVERITY ASSESSMENT — Severe bronchiolitis is indicated by persistently increased respiratory effort (tachypnea; nasal flaring; intercostal, subcostal, or suprasternal retractions; accessory muscle use; grunting), hypoxemia, apnea, or acute respiratory failure – In healthy infants and young children, bronchiolitis usually is a self-limited disease. – Maintain oxygenation and hydration. – Bronchodilator therapy may be beneficial in a subset of patients
- 43. Transient infant wheeze • The successful transition from fetal to neonatal life at delivery requires a series of rapid physiologic changes of the cardiorespiratory system. These changes result in redirection of gas exchange from the placenta to the lung and comprise: – Replacement of alveolar fluid with air – Onset of regular breathing – Increase in pulmonary blood flow as a result of increased systemic vascular resistance and decreased pulmonary vascular resistance (PVR)
- 44. • difficulty may be a consequence of : – impaired lung function due to fluid retention, – airway obstruction associated with congenital anomalies, – persistent pulmonary hypertension, – apnea associated with lack of respiratory effort.
- 45. Respiratory distress syndrome • Respiratory distress (ie, tachypnea and labored breathing) and cyanosis occur at or soon after birth. • Typical signs include – grunting (which prevents end-expiratory alveolar collapse), – nasal flaring (which reduces nasal resistance and reflects increased use of accessory muscles of respiration), – and intercostal and subcostal retractions (due to decreased lung compliance and the highly compliant chest wall). • Surfactant deficient • inability to clear lung fluid from air spaces
- 46. Bronchiectasis • Abnormal dilation and distortion of the bronchial tree, resulting in chronic obstructive lung disease. • End result of a variety of pathophysiologic processes that render the bronchial walls weakened, easily collapsible, chronically inflamed, and plugged with mucus secretions. • Associated findings include atelectasis, emphysema, fibrosis, and hypertrophy of the bronchial vasculature.
- 47. • S/s : productive cough, purulent sputum, fever, pleuritic chest pain, and dyspnea • PE : – Crackles (inspiratory popping sounds) and rhonchi (coarse expiratory breath sounds), – Wheezing (less common) – Clubbing of the nailbed – Chest wall deformity, which can be seen in obstructive lung diseases (eg, cystic fibrosis)
- 48. • Ix : – CXR - linear atelectasis and dilated and thickened airways, HRCT – sweat chloride or DNA testing – blood count with differential, immunoglobulins, and IgG subclasses • Mx : aimed at treating the underlying cause, improving mucocilliary clearance, treating and preventing infection, and controlling inflammation – Antibiotic therapy – Chest physiotherapy – Mucolytic agents and airway hydration – Bronchodilators – Anti-inflammatory drugs – Immunization
- 49. Laryngotracheobronchitis (Croup) • It is a viral infection of the middle respiratory tract occurs from 6 months to 6 years of age with peak incidence in the 2nd year of life. • There is mucosal inflammation and increased secretions affecting the airway, but it is the edema of the subglottic area that is potentially dangerous as it may result in critical narrowing of the trachea.
- 50. Laryngotracheobronchitis (Croup) • A small decrease in diameter secondary to mucosal edema and inflammation exponentially increases airway resistance and significantly increases work of breathing. • During inspiration, walls of the subglottic space are drawn together, aggravating the obstruction and producing stridor characteristic of croup.
- 51. Laryngotracheobronchitis (Croup) • Symptoms are Low grade fever, cough and coryza for 12-72 hours followed by Stridor that may occur when excited, at rest or both (Harsh, high-pitched respiratory sound produced by turbulent airflow; usually inspiratory, but may be biphasic and is a sign of upper airway obstruction) hoarse voice, brassy or “barking” cough Respiratory distress of varying degree • Onset of symptoms is usually over several days and often start and worse at night. • Symptomatic reinfection is common but usually mild.
- 52. Laryngotracheobronchitis (Croup) • Parainfluenza viruses (type 1,2,3) are the commonest cause but other viruses such as human metapneumovirus, RSV and influenza virus type A and B, adenovirus, enterovirus, measles, mumps and rhinoviruses can produce similar clinical picture. • Chest X-ray reveals a characteristic narrowing of the subglottic region known as the “steeple sign”.
- 54. Assessment of severity • a
- 55. Laryngotracheobronchitis (Croup) • When the upper airway obstruction is mild, the stridor and chest recession disappear when the child is at rest. • The child can usually be managed at home and need to be closely monitored for signs of increasing severity. • Most cases of croup are mild and resolve within 1 to 2 days.
- 56. Laryngotracheobronchitis (Croup) • Indication for hospital admission Moderate and severe viral croup Poor oral intake Family lives a long distance from hospital, lacks reliable transport Toxic looking Age less than 6 months Unreliable caregivers at home
- 58. Management of Croup • Oxygen therapy indication include severe viral croup and percutaneous SaO2 <93%. • Steroids are helpful in moderate to severe cases. • Antibiotics may be indicated if the child fails to improve or if purulent secretions are present where coverage should be directed towards Staphylococcus and H.influenzae.
- 59. Acute epiglottitis (Supraglottitis) • It is less common than croup, typically presents with a greater degree of airway compromise. • H.influenzae type B is the major etiologic organism. • The incidence of epiglottitis has decreased with the administration of H. influenzae vaccine. • It is most common in children aged 1-6 years but affect all age groups.
- 60. Clinical manifestations of Acute epiglottitis • Patients typically present with acute onset (over several hours) of High fever in an ill, toxic-looking child An intensely painful throat preventing child from speaking or swallowing with saliva drools down the chin Marked dysphagia Soft inspiratory stridor and rapidly increasing respiratory difficulty over hours Patients are often encountered leaning forward in a “tripod” position (Immobile, upright with an open mouth) • Unlike croup, cough is frequently absent.
- 61. Acute epiglottitis (Supraglottitis) • Attempts to lie the child down or examine the throat with a spatula or perform a lateral neck X-ray must not be undertaken as this may precipitate total obstruction and death. • Instrumentation of the throat with tongue depressors is not advisable as this can precipitate a fatal laryngospasm.
- 62. Acute epiglottitis (Supraglottitis) • If the diagnosis of epiglottitis is suspected, urgent hospital admission and treatment are required. • The child should be intubated under controlled conditions with a general anesthetic. • Rarely, this is impossible and urgent tracheostomy is life- saving. • Only after securing the airway, blood is taken for culture and broad-spectrum IV antibiotics such as cefuroxime directed against H.influenzae and gram-positive organisms started. • Tracheal tube can usually be removed after 24 hours and antibiotics given for 2-3 days. • Prophylaxis with rifampicin is offered to close household contacts.
- 63. Clinical features of croup and epiglottitis Croup Epiglottitis Onset Over days Over hours Preceding coryza Yes No Cough Severe, barking Absent or slight Able to drink Yes No Drooling saliva No Yes Appearance Unwell Toxic, very ill Fever <38.5 Celsius >38.5 Celsius Stridor Harsh, rasping Soft, whispering Voice, cry Hoarse Muffled, reluctant to speak
- 64. Laryngomalacia • It is the most common congenital anomaly of the larynx, accounting for up to 60% of all anomalies. • Inspiratory stridor is the hallmark of the condition. • Symptoms are typically aggravated when the child is supine or crying. • Examination reveals partial collapse of a flaccid supraglottic airway with inspiration. • The condition is generally benign and self-limited, as most cases resolve by 18 months of age. • Severe cases may require surgical intervention if the distress prevents adequate feeding.
- 68. Congenital subglottic stenosis Etiology •Can be iatrogenic •Intubation and mechanical ventilation – residual damage to the larynx •Down’s syndrome infants more susceptible due to smaller larynx Clinical manifestation •Subglottic obstruction produces stridor and frequently biphasic (expiration and inspiration) •Worsen with respiratory effort •Viral infection exacerbate subglottic stenosis Diagnostic studies •Requires endoscopic evaluation Treatment •Tracheostomy and reconstructive surgery may be necessary •Some improve with age as larynx grow and require no intervention
- 69. Retropharyngeal abscess & Peritonsilar abcess Retropharyngeal abscess Comparison Peritonsilar abscess <6 years Age >10 years Posterior pharynx Location Oropharynx S. aureus, anaerobes Etiology Group A streptococci, anaerobes Insidious to sudden Prodrome onset Biphasic with sudden worsening None Stridor No Yes Retraction No Muffled Voice “Hot potato” muffled Arching of neck or normal Position and appearance Normal Drooling Swallowing (dysphagia) Drooling, trismus No Barking cough None Severe Toxicity Dyspnea >101 F Fever >101 F Thickened retropharyngeal space X Ray None needed Leukocytosis with left shift WBC count Leukocytosis with left shift Antibiotics, surgical drain - abscess Therapy Antibiotics, aspiration None Prevention Treat Group A streptococci early
- 70. Diphtheria Etiology Caused by bacteria Corynebacterium diphtheriae spread through respiratory droplets from infected person or carrier Infects nose, throat causes gray to black, thick fiber like covering airway Infects skin - Skin lesions Produces toxins – spread via bloodstream to other organs Signs and symptom Mild fever, sore throat, chills – few days after infection Breathing problems, croup-like (barking cough), drooling, hoarseness Nasal discharge, fatigue Dysphagia, paralysis, heart failure – serious Tx Antitoxin IV/IM Antibiotics – penicillin and erythromycin Diphtheria vaccine – lasted for 10 years (if in contact with infected person)
- 71. Chronic lung disease of prematurity • Infants who still have an oxygen requirement at a post-menstrual age of 36 weeks are described as having bronchopulmonary dysplasia (BPD) or chronic lung disease. • Criteria for diagnosis are oxygen requirement beyond 36 weeks post conceptional age or beyond 28 days of life.
- 72. Pathophysiology of BPD • The lung damage (alveolar cells, interstitium and blood vessels) comes from pressure and volume trauma from artificial ventilation, oxygen toxicity and infection. • Oxygen concentration greater than 40% are toxic to the neonatal lung. • Oxygen-mediated lung injury results from the generation of superoxides, hydrogen peroxide and oxygen free radicals which disrupt membrane lipids.
- 73. Pathophysiology of BPD • Assisted ventilation with high peak pressures produces barotrauma, compounding the damaging effects of highly inspired oxygen levels. • Inflammatory mediators are released and causing increase permeability of blood vessels leading to leakage of water and protein. • In later stages, there is fibrosis and cellular hyperplasia. • Severe lung damage can leads to respiratory failure.
- 75. Risk factors of BPD • In most patients, BPD develops after ventilation for RDS that may have been complicated by PDA (Patent ductus arteriosus) or pulmonary interstitial emphysema. • Inflammation from prolonged assisted ventilation and repeated systemic and pulmonary infections may play a major role. • Failure of RDS to improve after 2 weeks, the need for prolonged mechanical ventilation and oxygen therapy required at 36 weeks’ postconceptional age are characteristics of patients with RDS in whom BPD develops.
- 76. Risk factors of BPD • BPD also may develop in infants weighing less than 1000g who require mechanical ventilation for poor respiratory drive in the absence of RDS. • 50% of infants of 24 to 26 weeks’ gestational age require oxygen at 36 weeks’ corrected age.
- 77. Chest X-Ray of BPD • The chest X-ray characteristically shows widespread areas of opacification, sometimes with cystic changes accompanied by areas of over-distention and atelectasis, giving the lung a sponge like appearance. • Histopathology of BPD reveals interstitial edema, atelectasis, mucosal metaplasia, interstitial fibrosis, necrotizing obliterative bronchiolitis and overdistended alveoli.
- 80. Clinical manifestations of BPD • The clinical manifestations of BPD are oxygen dependence, hypercapnia, compensatory metabolic alkalosis, pulmonary hypertension, poor growth and development of right-sided heart failure. • Increased airway resistance with reactive airway bronchoconstriction also is noted and is treated with bronchodilating agents. • Severe chest retractions produce negative interstitial pressure that draws fluid into the interstitial space. • Together with cor pulmonale, these chest retractions cause fluid retention, necessitating fluid restriction and the administration of diuretics.
- 81. Management of BPD • Some infants need prolonged artificial ventilation, but most are weaned onto continuous positive airways pressure (CPAP) followed by additional ambient oxygen, sometimes over several months. • To reduce risk of subglottic stenosis, a tracheotomy may be indicated. • To reduce oxygen toxicity and barotrauma, ventilator settings are reduced to maintain blood gases with slightly lower PaO2 (50mmHg) and higher PaCO2 (50 to 75 mmHg) levels than for infants during the acute phase of RDS.
- 82. Management of BPD • Dexamethasone therapy may reduce inflammation, improve pulmonary function and enhance weaning of patients from assisted ventilation. • However, corticosteroid therapy may increase risk of abnormal neuro-development including cerebral palsy, thus limits use to those at highest risk and only short courses are given.
- 83. Management of BPD • Some babies go home while still receiving additional oxygen. • A few infants with severe disease may die of intercurrent infection or pulmonary hypertension. • Some survivors of BPD have hyperinflation, reactive airways and developmental delay. • Subsequent pertussis and RSV (Respiratory syncytial virus) infection may cause respiratory failure necessitating intensive care and thus prophylaxis against RSV should be given.
- 84. Inhaled foreign body Epidemiology •Common, 4 y/o •Main right bronchus (direct continous with trachea •May migrate on larynx (coughing) causes occlusing of airway Clinical manifestation •Cough, localized wheezing, unilateral absence of breath sounds, stridor, blood sputum (rare) •fever, cough, sputum production, or chest pain – need medical attention •Persistence wheezing unresponsive to bronchodilator therapy, persistent atelectasis, recurrent or persistence pneumonia, persistent cough without other explanation – suspect foreign body inhalation. •Lodge in esophagus and compress trachea – produce respiratory symptoms Diagnostic studies •Radiographic studies – presence of radiopaque object or eveidence of air trapping Prevention •Education to parent and caregiver •Small toys should kept away
- 85. Pneumothorax • defined as a collection of air that is located within the thoracic cage between the visceral and parietal pleura – Primary : no underlying lung disease – Secondary : complication of underlying lung disease (ie asthma, cystic fibrosis, necrotizing pneumonia, and interstitial lung disease)
- 86. • S/s : dyspnea and pleuritic chest pain that is described as sharp or stabbing. The pain typically is diffuse on the affected side with radiation to the ipsilateral shoulder. A dry or non-productive cough • PE : – deviation of the trachea towards the contralateral side – diminished breath sounds – hyperresonant percussion – decreased vocal fremitus on the affected side. – Other signs : tachypnea, increased work of breathing, and cyanosis.
- 87. • Ix : ABG, CXR • Mx : depends on the size of the pneumothorax, the extent of respiratory distress, and the presence or absence of underlying lung disease. The goals of treatment are to remove air from the pleural space and to prevent recurrence. – Supplemental oxygen – Needle aspiration – Thoracostomy tube
- 88. Empyema • Early in the course of parapneumonic effusion, the pleura becomes inflamed; leakage of proteins, fluid, and leukocytes. At the time of formation, the pleural effusion is usually sterile with a low leukocyte count. With time, bacteria invade the fluid, resulting in empyema, which is defined as the presence of grossly purulent fluid in the pleural cavity. • S/s : persistent fever, cough, malaise, decreased appetite, chest pain, and dyspnea • PE : tachypneic, but breaths may be shallow to minimize pain, mediastinal shift and tension hydrothorax, Hypoalbuminemia
- 89. • Ix : Pulse oximetry , Blood and sputum culture, CXR • Management: – Main goals : sterilization of the pleural cavity, resolution of pleural fluid, and reexpansion of the lung – Antibiotics – Thoracocentesis – Chest tubes – Surgical (for symptoms for more than one week only)
- 90. Pneumatocele • A pneumatocele is a cavity in the lung parenchyma filled with air (cyst) that may result from pulmonary trauma during mechanical ventilation • Ddx : Lung ca, TB • Mx : palliative care
- 91. Lung abscess • Result from lung tissue necrosis from an infection (ie pneumonia) • Conditions contributing to lung abscess – Aspiration of oropharyngeal or gastric secretion – Septic emboli – Vasculitis: Wegener's granulomatosis – Necrotizing tumors:
- 92. Congenital diaphragmatic hernia Congenital lobar emphysema (congenital lobar over distention) Etiology Over inflation of one lobe during neonatal Improper joining of structure during fetal dev. period – left upper lobe (often) Stomach, small intestine, spleen appear in chest cavity, Lung tissue not completely develop Left side – common Increase risk with +ve family hx Symptom •Produces respiratory distress because Breathing difficulty after born due to surrounding lung tissue has compressed ineffective movement of diaphragm and •Mediastinal shift crowding of lung tissue, which causes collapse Cyanosis, tachypnea, tachycardia Irregular chest movement Absence of breath sound on both side Bowel sound heard in the chest Palpation – abd feels less full Xray – abd organs in chest cavity Surgery - place abd organs back n repair Lobectomy – if RDS is severe and progressive diapgrmatic opening Breathing support until recvers from surgery
- 93. H type- tracheoesophageal fistula -
- 94. • S/s : if the defect is large, with coughing and choking associated with feeding. • Diagnosis — attempt to pass a catheter into the stomach. This finding can be confirmed with an anterior-posterior chest radiograph that demonstrates the catheter curled in the upper esophageal pouch • Mx : surgical ligation of the fistula. – if the distance between esophageal segments is large, staged procedures are performed that include elongation of the esophagus.
- 96. Gastroesophageal reflux (GER) It is defined as the effortless retrograde movement of gastric contents into the esophagus. In infancy, GER is not always an abnormality. Distinction between physiologic GER and pathologic GER in infancy and childhood is determined by presence of reflux-related complications.
- 97. Physiologic GER Physiologic GER (Spitting up) is normal in infants younger than 8 to 12 months of age. Nearly half of all infants are reported to spit up at 2 months of age. It is caused by inappropriate relaxation of the lower esophageal sphincter as result of functional immaturity. Infants who regurgitate stomach contents meet the criteria for physiologic GER, as long as they maintain adequate nutrition and have no signs of respiratory complications or esophagitis.
- 98. Clinical manifestations Presence of GER is easy to observe in an infant who spits up. In older children, the refluxate is usually kept down by reswallowing, but GER may be suspected by associated symptoms, such as: • Heartburn • Cough • Dysphagia • Wheezing • Aspiration pneumonia • Hoarse voice • Failure to thrive • Recurrent otitis media/ Sinusitis
- 99. Clinical manifestations GER can have both esophageal and extraesophageal manifestations. The esophageal manifestations are those caused directly by contact between refluxed gastric juice and the esophageal mucosa. The extra-esophageal manifestations are caused by contact between refluxed gastric juice and extraesophageal organs or by reflexes triggered by acid in the esophagus that affects other organs.
- 100. Extraesophageal complications Cardiac: Atypical chest pain, ischemia Vocal cords: Laryngitis, granuloma, polyps, ulcers, neoplasm Respiratory: asthma, recurrent bronchitis, aspiration or chronic interstitial pneumonia, sleep apnea, chronic or recurrent cough Pharyngeal: pharyngitis, hoarseness Oral: Erosions, burning mouth syndrome Other: sudden infant death syndrome, otitis media
- 101. Investigations 1. Barium upper gastrointestinal series 2. 24-hour esophageal pH probe monitoring 3. Esophageal impedance monitoring 4. Endoscopy
- 102. Relation to respiratory symptoms GER has been associated with significant respiratory symptoms in infants and children. The infant’s proximal airway and esophagus are lined with receptors that are activated by water, acid or distention. Activation of these receptors can increase airway resistance, leading to development of reactive airway disease.
- 103. Relation to respiratory symptoms One postulated mechanism for gastroesophageal reflux- mediated airway disease involves micro-aspiration of gastric contents that leads to inflammation and bronchospasm. However, experimental evidence also supports the involvement of esophageal acid-induced reflex bronchospasm in the absence of frank aspiration. Therapy using histamine 2 blockers or proton pump inhibitors has been shown to benefits patients with steroid-dependent asthma, nocturnal cough and reflux symptoms.
- 104. Asthma and GER In 1892, Sir William Osler first postulated a relationship between asthma and gastroesophageal reflux, manifested by a bi-directional cause-and-effect presentation. Prevalence of GER is more common in asthmatics compared to control populations ranging from 47 to 75%. Severe studies suggest that severe nocturnal asthma is more likely to be associated with GER than daytime asthma.
- 106. Asthma and GER Not all asthmatics with GER will have esophageal symptoms. The mechanism of esophageal acid induced bronchoconstriction includes a vagally mediated esophageal bronchial reflex, airway hyper responsiveness and microaspiration.
- 109. Asthma and GER It has been suggested that a vagally mediated reflex exists whereby acid reflux into the lower esophagus initiates bronchoconstriction via a shared autonomic innervation between esophagus and bronchi based on their common embryonic origin. Support is based on this two lines of evidence: • Acid infusion of the esophagus in asthmatic children results in increased airway resistance, which can be reversed with antacids. • Infusion of antacids into the distal esophagus of asthmatic children during sleep induces bronchoconstriction, suggesting presence of a protective mechanism.
- 110. Asthma and GER Esophageal acidification has also been associated with heightened non-specific hyperresponsivity of the airways to bronchoconstrictors contributed by increased vagal tone, “priming” the airways to other triggers.
- 111. Asthma and GER Asthmatics have significant decreased lower esophageal sphincter pressures, greater esophageal acid exposure times, more frequent episodes of GER and longer esophageal acid clearance times. There may be increase in transient lower esophageal sphincter (LES) relaxations, LES hypotonia and esophageal due to autonomic dysfunction in asthmatics patient. Furthermore, LES pressure augmented by diaphragm normally prevents GER but it can be prevented by hyperinflation and hiatal hernia. LES pressure can also be overcome by increased negative intrathoracic pressures (bronchospasm, cough, upper airway resistance syndrome and obstructive apnea).
- 112. Asthma and GER Anti-reflux therapy results in improvement in asthma in approximately 70% of patients. Acid-suppression medication such as histamine 2 receptor antagonists (ranitidine) or proton pump inhibitors (omeprazole) are helpful in reducing volume of gastric contents. (Therapeutic trial)
- 115. Chronic cough and GER GER can potentially stimulate sensory limb of cough reflex in multiple ways. It can irritate upper respiratory tract without aspiration (such as larynx) and the lower respiratory tract by either macro-microaspiration. It can also cause cough by stimulating an esophagus bronchial cough reflex whereby refluxate into distal esophagus alone is a sufficient stimulus.
- 116. Chronic cough and GER GER related cough occurs predominantly during the day and in the upright position whereby some patients may have nocturnal symptoms. Cough may be the sole manifestation of GER and is often long standing. Diagnosis can be made with certainty only when cough are resolved with specific anti-reflux therapy.
- 117. Senario 3 Samy, a 2 days old premature infant who was born at 30 weeks gestational age was noted to be cyanosed by a nurse. There was absence of chest movement. What is Samy’s clinical condition? Respiratory distress syndrome (RDS) What is your immediate action? surfactant replacement therapy IV glucocorticoid administration What is the mechanism of his respiratory failure? Immature lung lack surfactant atelectasis
- 118. Senario 5 Aminah a 2 year old toddler has been having mild cough and rhinorrhea for the past 2 days. It was associated with low grade fever. Suddenly her mother noticed that she breath noisily with fast breathing. What is Aminah’s clinical condition? Common cold What are the relevant physical finding that you would like to look for? Signs of respiratory distress Outline the principle management. Symptomatic therapy
