4.n periodontal aspects
- 1. 1 1 Periodontal AspePeriodontal Aspectscts ofof Fixed ProsthodonticsFixed Prosthodontics
- 2. 2 2 Patients seeking prosthodontic treatment may possess HealthyHealthy periodontal statusperiodontal status PeriodontallyPeriodontally comprised statuscomprised status
- 3. 3
- 4. 4
- 5. 5 5 Patient may possess:Patient may possess: A.A. HHealthy periodontal statusealthy periodontal status in which case our goal would be to:in which case our goal would be to: maintain and preservemaintain and preserve by inserting restorations which would not provoke or insult theby inserting restorations which would not provoke or insult the attachment apparatus but maintain its well being.attachment apparatus but maintain its well being. B.B. Periodontally comprised statusPeriodontally comprised status in which case our goal would bein which case our goal would be 1.1. to diagnose and treat the condition,to diagnose and treat the condition, 2.2. arrest its progressarrest its progress 3.3. establish a regimen of strict oral hygieneestablish a regimen of strict oral hygiene followed byfollowed by 4.4. inserting restorationsinserting restorations which would help promote and preserve the attachmentwhich would help promote and preserve the attachment apparatus of the abutments in a state of health.apparatus of the abutments in a state of health.
- 6. 6
- 7. 7 7 MG→ Marginl Gingiva AG→Attached Gingiva AM→Alveolar Mucosa 1. Free marginal gingiva: Covering the neck of the tooth and extending to the epithelial attachment. 2. Interdental papillae: Triangular gingival projection, filling the area between the adjacent teeth apical to the contact point. 3. Attached gingiva: Extends from the epithelial attachment to the junction between the gingiva and the alveolar mucosa i.e. from the muco-gingival junction till it meets the alveolar mucosa.
- 8. 8 8 Periodontal ligament:Periodontal ligament: Is composed of collagen fibres embedded in alveolar bone and cementum.Is composed of collagen fibres embedded in alveolar bone and cementum. It supports the tooth and anchors it to the jaw.It supports the tooth and anchors it to the jaw. A healthy periodontal ligament in functional occlusion is 0.25 mm wide.A healthy periodontal ligament in functional occlusion is 0.25 mm wide. It is widest at the margin and apex and narrower in the middle.It is widest at the margin and apex and narrower in the middle. Fibres of the periodontal ligament: 1.Alveolar crest 4. Horizontal 2.Oblique 5. Interradicular 3.Transeptal 6. Apical
- 9. 9 9 Functions of the periodontal ligament:Functions of the periodontal ligament: 1.Supportive function:1.Supportive function: Periodontal ligament not onlyPeriodontal ligament not only connects the tooth to the alveolar boneconnects the tooth to the alveolar bone but alsobut also supports the tooth in its socket.supports the tooth in its socket. 22. Formative function:. Formative function: The ligament is aThe ligament is a reservoir for cellsreservoir for cells which are mesenchymal cells and can differentiate into :which are mesenchymal cells and can differentiate into : bone forming cells (osteoblast),bone forming cells (osteoblast), cementum forming cells (cementoblast)cementum forming cells (cementoblast) ligament forming cells (fibroblast).ligament forming cells (fibroblast). 3.Sensory function:3.Sensory function: Contain mechanoreceptors that are stimulated to reduce forces. The mechanoreceptorsContain mechanoreceptors that are stimulated to reduce forces. The mechanoreceptors in the periodontal ligament monitor changes in pressure within the ligament.in the periodontal ligament monitor changes in pressure within the ligament. As forces increase, greater numbers of mechanoreceptors are stimulated.As forces increase, greater numbers of mechanoreceptors are stimulated. These results in increasing numbers of impulses passing via the sensory nerves, in turnThese results in increasing numbers of impulses passing via the sensory nerves, in turn results in inhibitory impulses that reduce or stop masticatory forces.results in inhibitory impulses that reduce or stop masticatory forces.
- 10. 10 10 4.Socket absorbing function:4.Socket absorbing function: Periodontal ligament absorbs loads imposed on the tooth thusPeriodontal ligament absorbs loads imposed on the tooth thus protecting the tooth especially at the apex.protecting the tooth especially at the apex. Axial forcesAxial forces are absorbed most readily. On loading the wavy principleare absorbed most readily. On loading the wavy principle fibers assume their full length and the tooth is depressed in the socket.fibers assume their full length and the tooth is depressed in the socket. The fibers of the periodontal ligament withstand forces in the long axisThe fibers of the periodontal ligament withstand forces in the long axis of the tooth.of the tooth. Lateral and rotational forcesLateral and rotational forces are less absorbed. Onare less absorbed. On tensiontension side fibersside fibers are extended and on theare extended and on the pressurepressure side fibers are compressed. Furtherside fibers are compressed. Further compression results in bone resorption.compression results in bone resorption. Horizontal (lateral) forcesHorizontal (lateral) forces are produced in balancing side interferencesare produced in balancing side interferences and are destructive to the periodontium. They initiate bone resorption inand are destructive to the periodontium. They initiate bone resorption in areas of pressure and bone formation in areas of tension.areas of pressure and bone formation in areas of tension. Pressure compressed Tension extended
- 11. 11 11 One of the primary goals of the restorative dentist should be to accomplish the required procedureOne of the primary goals of the restorative dentist should be to accomplish the required procedure with a minimal degree of tissue damage to the gingival tissue.with a minimal degree of tissue damage to the gingival tissue.
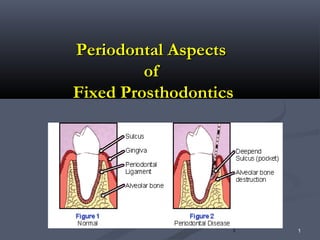
- 12. 12 12 TheThe periodontiumperiodontium is composed of the whole attachment unit::is composed of the whole attachment unit:: Gingiva – periodontal ligament – cementum and alveolar bone.Gingiva – periodontal ligament – cementum and alveolar bone. The gingival crevice:The gingival crevice: Normal depthNormal depth 1-2 mm ~ 1.8 mm1-2 mm ~ 1.8 mm Epithelial attachmentEpithelial attachment 1 mm1 mm Connective tissue attachmentConnective tissue attachment 1 mm1 mm Alveolar crest is located 2 mm apical to the base of the sulcus.Alveolar crest is located 2 mm apical to the base of the sulcus. A-B Gingival Crevice, B-C Junctional epithelium, C-D Connective tissue attachment, B-D Biologic Width
- 13. 13 13 Biologic width:Biologic width: It is composed of junctional (sulcular) epithelium which lines the lateral wall of theIt is composed of junctional (sulcular) epithelium which lines the lateral wall of the gingival crevice and connective tissue attachment.gingival crevice and connective tissue attachment. Periodontal pocket:Periodontal pocket: It is the apical migration of the epithelial attachment with the loss of connective tissueIt is the apical migration of the epithelial attachment with the loss of connective tissue and eventually a lveolar bone loss.and eventually a lveolar bone loss. Gingivitis:Gingivitis: If bleeding occurs while probing the gingiva with a blunt probe this is an indication ofIf bleeding occurs while probing the gingiva with a blunt probe this is an indication of ulceration of the sulcular epithelium.ulceration of the sulcular epithelium. Gingivitis is caused byGingivitis is caused by local irritation from plaque, bacteria, calculus and foodlocal irritation from plaque, bacteria, calculus and food impaction.impaction. Periodontitis:Periodontitis: It is a direct extension of neglected gingivitis, involving the deeperIt is a direct extension of neglected gingivitis, involving the deeper tissues of the periodontium. It is characterized by:tissues of the periodontium. It is characterized by: 1.1. pocket formation andpocket formation and 2.2. alveolar bone loss.alveolar bone loss.
- 14. 14 14 Factors in Fixed Restorations which affect periodontal health:Factors in Fixed Restorations which affect periodontal health: 1.Crown margins:1.Crown margins: ExtensionExtension (location/position) length.(location/position) length. Nature & shape, (sharp/dull/round/blunt/polished.)Nature & shape, (sharp/dull/round/blunt/polished.) Restoration material.Restoration material. Shape ,thickness & adaptation of margins:Shape ,thickness & adaptation of margins: 2.Axial crown contour:2.Axial crown contour: Proximal contact.Proximal contact. .. EmbrasureEmbrasure Facial & lingual contour.Facial & lingual contour. Emergence profile.Emergence profile. 3.Occlusal Forces & anatomy.3.Occlusal Forces & anatomy. Occlusal table dimension. Force magnitude, duration, frequency.Occlusal table dimension. Force magnitude, duration, frequency. 4. Pontic design & material.4. Pontic design & material. 5. Bridge Design5. Bridge Design
- 15. 15 15 1.1. Crown marginsCrown margins:: A. Extension of margin:A. Extension of margin: a. Supragingivala. Supragingival: (above the gingival crest): (above the gingival crest) It is the optimum position of the finish line for the health of the gingiva.It is the optimum position of the finish line for the health of the gingiva. It provides proper vision and accessibility during preparation, impression and evaluation.It provides proper vision and accessibility during preparation, impression and evaluation. It is easier to prepare, no soft tissue trauma occurs and is easily cleaned patient. In case of gingival recession,It is easier to prepare, no soft tissue trauma occurs and is easily cleaned patient. In case of gingival recession, preparations should end at the cementoenamel junction.preparations should end at the cementoenamel junction. b. Subgingivalb. Subgingival:: This location was considered self cleansing in the past but recently this was proven wrong and a major cause ofThis location was considered self cleansing in the past but recently this was proven wrong and a major cause of gingival recession.gingival recession. However, some conditions necessitate this position such as:However, some conditions necessitate this position such as: 1.1. Caries.Caries. 2.2. Root sensitivityRoot sensitivity 3.3. Erosion.Erosion. 4.4. Esthetics.Esthetics. 5.5. Insufficient retention caused by short OGInsufficient retention caused by short OG 6.6. Cervical location of proximal contactCervical location of proximal contact However, care must be taken to position the marginHowever, care must be taken to position the margin midway in the sulcus between the gingival crest and the depth of the sulcus.midway in the sulcus between the gingival crest and the depth of the sulcus. Iatrogenic tearing of the epithelial attachment results in its apical migration and pocket formation.Iatrogenic tearing of the epithelial attachment results in its apical migration and pocket formation. C. At the crest:C. At the crest: Finish lines should never be located at that position as margins are always rough due to microirregularitiesFinish lines should never be located at that position as margins are always rough due to microirregularities inviting food debris and plaque accumulation thus causing continuous irritation,decay or periodontalinviting food debris and plaque accumulation thus causing continuous irritation,decay or periodontal involvement.involvement.
- 16. 16 16 b.b. Nature and shape of the margin:Nature and shape of the margin: Margins should beMargins should be smooth, blunt, round and polishedsmooth, blunt, round and polished. Rough,. Rough, sharp, porous margins harbor bacteria and plaque causing irritationsharp, porous margins harbor bacteria and plaque causing irritation leading to gingivitis.leading to gingivitis. Fingertip examination of all restoration margins should be doneFingertip examination of all restoration margins should be done before insertion to ensure smooth, rounded polished extensionsbefore insertion to ensure smooth, rounded polished extensions for better gingival tissue tolerance.for better gingival tissue tolerance. C.C. Restoration material:Restoration material: Acrylic temporary crownsAcrylic temporary crowns:: Should be blunted and polished to a smooth finish with a lathe andShould be blunted and polished to a smooth finish with a lathe and wheel followed by fine pumice.wheel followed by fine pumice. Porcelain:Porcelain: Glazing provides the smoothest surface. After minor intraoralGlazing provides the smoothest surface. After minor intraoral adjustments of glazed porcelain it may be polished using coarse (greenadjustments of glazed porcelain it may be polished using coarse (green silicon carbide) to fine white rubber stones containing fine grainedsilicon carbide) to fine white rubber stones containing fine grained aluminum oxide followed by a fine- particle diamond paste applied onaluminum oxide followed by a fine- particle diamond paste applied on a felt wheel or diamond impregnated wheels and points.a felt wheel or diamond impregnated wheels and points.
- 17. 17 Gold alloys:Gold alloys: Are finished using coarse, medium and fine abrasives followed by rubberAre finished using coarse, medium and fine abrasives followed by rubber wheels impregnated with fine abrasives (white). Final polishing is donewheels impregnated with fine abrasives (white). Final polishing is done with Tripoli and rouge (iron-oxide) on rag wheels or a soft-bristle brush.with Tripoli and rouge (iron-oxide) on rag wheels or a soft-bristle brush. Subgingival margins may be burnished on the die with a fine stone.Subgingival margins may be burnished on the die with a fine stone. No intra-oral finishing is done to avoid injury of the gingiva.No intra-oral finishing is done to avoid injury of the gingiva. Base metals:Base metals: Any rough areas or margins are smoothened with blue rubber wheelsAny rough areas or margins are smoothened with blue rubber wheels followed by white rubber wheels.followed by white rubber wheels. Glazed porcelain followed by polished gold margins are better tolerated .Glazed porcelain followed by polished gold margins are better tolerated . The least tolerated are acrylic margins.The least tolerated are acrylic margins.
- 18. 18 18 d. Fit and adaptation of margins:d. Fit and adaptation of margins: Successful margins should possess good marginalSuccessful margins should possess good marginal adaptation with a gap of 50-120 µm.adaptation with a gap of 50-120 µm. Types of defective margins:Types of defective margins: a. Overextended b. Underextended c. Thicka. Overextended b. Underextended c. Thick d. Opend. Open
- 19. 19 19 22) Axial crown contour:) Axial crown contour: Improper crown contours impair gingival health.Improper crown contours impair gingival health. Proximal contactProximal contact:: Must be more than a point OG but should notMust be more than a point OG but should not extend too much cervically in order not to encroach on the gingivalextend too much cervically in order not to encroach on the gingival embrasure.embrasure. Occluso-gingival locationOccluso-gingival location:: AnteriorAnterior Incisal third.Incisal third. PosteriorPosterior mostly occlusal third towards the buccal except betweenmostly occlusal third towards the buccal except between 6 & 7 where it is in middle third6 & 7 where it is in middle third Bucco-lingual location:Bucco-lingual location: Facial to the middle third except for 6 & 7, where it is centered.Facial to the middle third except for 6 & 7, where it is centered. Buccolingual positionBuccolingual position OcclusogingivalOcclusogingival positionposition
- 20. 20 20 Errors in contact:Errors in contact: Broad proximal contactBroad proximal contact (wide BL) crowds the facial &(wide BL) crowds the facial & lingual papilla trapping food debris leading to gingivallingual papilla trapping food debris leading to gingival inflammation, and pressure on interdental papilla.inflammation, and pressure on interdental papilla. Narrow contact pointNarrow contact point Allows wedging of fibrous foodAllows wedging of fibrous food Deficient contactDeficient contact causes proximal caries and foodcauses proximal caries and food wedging.wedging. Tight contactTight contact causes lateral forces & torque oncauses lateral forces & torque on the tooth.the tooth. Contact is checked by comparing resistance of unrestoredContact is checked by comparing resistance of unrestored intact teeth to the introduction of dental floss.intact teeth to the introduction of dental floss.
- 21. 21 21 b.b. Gingival embrasureGingival embrasure:: Spaces that widen from the proximalSpaces that widen from the proximal contact filled with gingival tissue.contact filled with gingival tissue. Proximal surfaces gingival to the contact area should be flatProximal surfaces gingival to the contact area should be flat or concave.or concave. Function:Function: 1.1. Protect the gingiva from food impaction.Protect the gingiva from food impaction. 2.2. Deflect the food to massage the gingiva.Deflect the food to massage the gingiva. 3.3. Provide spillways for food during mastication.Provide spillways for food during mastication. 4.4. Allow proper oral hygiene.Allow proper oral hygiene. Proximal surfaces gingival to the contact area should be flat or concave.
- 22. 22 22 Occlusal embrasure:Occlusal embrasure: Occlusal to contact.Occlusal to contact. Gingival embrasure :Gingival embrasure : Gingival to contact pointGingival to contact point Lingual embrasure:Lingual embrasure: is wider than the buccal embrasure.is wider than the buccal embrasure. Inter-proximal space:Inter-proximal space: Anterior:Anterior: Should be just large enough for floss toShould be just large enough for floss to pass with resistance without compromisingpass with resistance without compromising esthetics.esthetics. Posterior:Posterior: May be wider to promote easy access toMay be wider to promote easy access to hygiene.hygiene.
- 23. 23 Facial and lingual contour: Should be in harmony with the adjacent teeth. Position: Buccally- Height of contour Its position is located at the cervical third in case of premolars & molars both maxillary & mandibular. Lingual mandibular posterior Middle 1/3 A. in harmony with adjacent teeth B. not in harmony Extension: It extends horizontally 0.5 mm beyond outline of the root at the CEJ in maxillary teeth, while it extends 0.75 and 1 mm on mandibular premolars and molars respectively. Bulge (extensive convexity): Over-contoured restorations with large convexities encourage accumulation of food debris and plaque retention leading to gingivitis while under-contouring is reported to be harmless.
- 24. 24 d)Emergence profile: It is the area below the height of contour and contact area. It is the part of the tooth extending from the base of the gingival sulcus to the height of contour. A straight profile should be reproduced to allow access for oral hygiene, it is easier to floss. Straight or concave profiles are allowed, never convex. Furcation Involvement: In case of teeth with gingival recession and furcation involvement: the surfaces directly occlusal to furcations are usually concave and the concavity should extend occlusally on the axial surface of the restoration to improve access for a toothbrush.
- 25. 25 3. Occlusal Forces & anatomy. During function (mastication and swallowing) functional forces act for fractions of a second and their direction is mainly vertical. The attachment apparatus is well adapted to resist axial forces i.e. forces directed within the periphery of the root. While lateral or horizontal forces are accommodated by, bone resorption in areas of pressure and bone formation in areas of tension. Rotational forces (torque) are the most harmful The periodontal tissues resist forces through: Collagen fibres which transmit occlusal forces as tension to the alveolar bone. Compressive forces are also resisted. Proprioceptive mechanism Reflex activity. It is a feed back mechanism which protects the periodontium, e.g. in case of the presence of a hard object in the food bolus. Proprioceptors in the periodontal ligament cause the jaws to open by reflex activity, thus controlling any stresses.
- 26. 26 4.Pontic design & Material: The pontic is that part of the bridge, which acts as the substitute for the lost tooth and is suspended between the retainers .It replaces the lost natural tooth both functionally and esthetically. In evaluating the relation of the pontic design with the health of gingival tissue, each surface of the pontic will be discussed separately. a) Gingival surface: To prevent ulceration and inflammation of the soft tissues, pressure- free contact area between the pontic and the underlying tissues is indicated. The area of contact touching the ridge should be as convex as possible. The gingival surface should meet gingival tissue with a smooth rounded contour. In the anterior, premolar and maxillary molar (esthetic demand zone) tissue contact of the pontic is recommended facially. Accordingly, the modified ridge lap area (concave buccally and convex lingually) is accepted.
- 27. 27 In the mandibular posterior area (for hygienic demands)tissue clearance is recommended. Therefore, sanitary pontic is used. (convex buccolingually) . Note:Anterior pontics are influenced by Esthetic demands while in Posterior areas Hygienic demands predominate
- 28. 28 B)Occlusal surface: The concept in designing the occlusal surface of the pontic should be to minimize the forces exerted on it. Reducing the buccolingual width of the pontic by as much as 30% was suggested as a means of decreasing occlusal forces on the abutment teeth. Actually narrowing the occlusal table may affect harmonious and stable occlusal relationships, consequently pontics with normal occlusal width (at least on the occlusal third) are generally recommended. Proprioceptive mechanism controls occlusal forces; reduction of the occlusal table does not diminish the effects on the abutment teeth. However, reduction of the pontic width is desirable only if the residual alveolar ridge has collapsed buccolingually to facilitate plaque control measures.
- 29. 29 C) Proximal surfaces: Vertical clearance must be sufficient to permit physiologic contour of the pontic and to allow space for the interproximal tissues. Interproximal embrasures should be open to permit access for cleaning. The maxillary anterior proximal embrasures are minimal for esthetics but should allow sufficient space to prevent papillary impingement. Moving posteriorly, the size of the embrasures gradually increases. In the mandibular posterior area, wider embrasures are created to facilitate hygiene since esthetics is not of prime concern.
- 30. 30 D) Buccal and lingual surfaces: The contours of the buccal and the lingual surfaces of the pontic are determined by esthetics, function and hygienic requirements. In the maxillary and mandibular anterior region, esthetics demands maintaining normal facial contour (convex inciso-gingivally and mesio- distally) axial alignement and length. Posteriorly, the lingual contour should harmonize, with adjacent teeth from the cusp tip to the height of contour, and then sharply recede convexly to the facial tissue contact area. Embrasures on the lingual are wider than on the buccal. In the mandibular posterior region, the buccal and the lingual surfaces follow normal tooth form from the cusp tip to the height of contour. The sanitary design results from tapering the buccal and the lingual surfaces from the height of contour toward the gingival contact. While the modified ridge lap adapts to the facial portion of the ridge only (concave).
- 31. 31 Pontic material: The requirements for any material to be used as a pontic is that it should provide good esthetics. biocompatibility, rigidity and strength to withstand occlusal forces. Longevity. The biocompatibility of the materials used to fabricate pontics is based on two factors: the effect of the materials and the effects of its surface adherence Glazed porcelain is considered to be the most biocompatible of the available pontic materials and the most resistant to the accumulation of plaque. Well-polished gold is smoother, possesses high corrosion resistance and is less retentive of plaque than unpolished or porous casting. Highly polished gold is also more resistant to initial plaque accumulation than rougher surfaces. For ease of plaque removal, it is recommended that the tissue surface of the pontic be made in glazed porcelain. If gold is placed in the tissue contact it should be highly polished. Acrylic pontics are the worst due to their plaque retention and imbibition potential. Surface finish is the most significant factor in pontic material.
- 32. 32 5.) Bridge Design: Different Fixed Partial Denture Designs produce different magnitude of tipping force: A)Fixed Fixed Bridge: The degree of bending or deflection is controlled by the position of the bridge,as well as the span dimension and pontic design and material. Ex extra hard alloys should be used in long spans to minimize bending. B)Fixed Supported Bridge: Occlusal forces will be distributed as follows; 11/16 on the abutment towards the soldered joint and 5/16 on the rest seat. C)Fixed Free (Cantilever Bridge): The balance between the tipping force and the periodontium varies according to the length of the pontic (Tipping or lever arm) and the number of abutments which denotes the surface area of periodontium (Resistance arm)
- 33. 33 Note: Short span & ↑ abutments→increase in surface area of resisting abutments → thickened lamina dura increasing bone resistance to the forces.Formation of new bone due to mild force applied to abutments and accommodation. ↑ surface area of periodontium→ ↑ mild effect ↑ tipping arm→ ↑serious effect on the periodontium Long edentulous span & ↓abutments → looseness & failure of bridge and abutments Bridge Design: Different Fixed Partial Denture Designs produce different magnitude of tipping force:
- 34. 34
- 35. 35
- 36. 36
- 37. 37
- 38. 38
- 39. 39 39 Treatment plan for periodontally comprised dentitions:Treatment plan for periodontally comprised dentitions: B.B. Periodontally comprised statusPeriodontally comprised status in which case our goal would bein which case our goal would be 1.1. to diagnose and treat the condition,to diagnose and treat the condition, 2.2. arrest its progressarrest its progress 3.3. establish a regimen of strict oral hygiene followed byestablish a regimen of strict oral hygiene followed by 4.4. inserting restorationsinserting restorations which would help promote and preserve the attachmentwhich would help promote and preserve the attachment apparatus of the abutments in a state of health.apparatus of the abutments in a state of health.
- 40. 40
- 41. 41 Causes and Etiology of Periodontal Disease:Causes and Etiology of Periodontal Disease: Most gingival and periodontal disease result fromMost gingival and periodontal disease result from microbialmicrobial plaqueplaque which causes inflammation. Other factors whichwhich causes inflammation. Other factors which contribute to inflammation are calculus, pathogens and foodcontribute to inflammation are calculus, pathogens and food debris.debris. Teeth withstand forces along their long axis because of theTeeth withstand forces along their long axis because of the arrangement of their fibers.arrangement of their fibers. In case of increasing function on the periodontium, theseIn case of increasing function on the periodontium, these forces maybe accommodated by the adaptive capacity of theforces maybe accommodated by the adaptive capacity of the periodontium. This adaptation varies between patients.periodontium. This adaptation varies between patients.
- 42. 42 42
- 43. 43 43 Stages of periodontal disease:Stages of periodontal disease: Marginal lesion.Marginal lesion. Early clinical signs. Ex redness, swelling, tenderness,Early clinical signs. Ex redness, swelling, tenderness, bleeding. Local irritants inducing gingivitis and pocket formation affectbleeding. Local irritants inducing gingivitis and pocket formation affect the marginal gingiva only. (Inflammation without trauma)the marginal gingiva only. (Inflammation without trauma) Advanced lesionAdvanced lesion.. Deeper layers are involved along with osteolyticDeeper layers are involved along with osteolytic activity and alveolar bone resorption.activity and alveolar bone resorption. If this is associated with traumatic occlusion then loss of bone isIf this is associated with traumatic occlusion then loss of bone is enhanced causing mobility.enhanced causing mobility.
- 44. 44 44
- 45. 45 Occlusal Trauma Occlusal traumatization is defined as forces originating by movement of maxillary and mandibular teeth in a way that creates a pathologic lesion. The primary occlusal trauma is a pathologic lesion that has been created by a force strong enough to disturb a normal intact periodontium . While, the secondary occlusal trauma is a lesion created by a normal function on a weakened periodontium because of periodontal disease.
- 46. 46 46 Traumatic occlusion:Traumatic occlusion: Local irritants inducing gingivitis and pocket formationLocal irritants inducing gingivitis and pocket formation affect the marginal gingiva only. (Inflammation withoutaffect the marginal gingiva only. (Inflammation without trauma)trauma) In the absence of inflammation and local irritants, occlusalIn the absence of inflammation and local irritants, occlusal trauma causes:trauma causes: 1.1. No gingivitis or periodontal pocket.No gingivitis or periodontal pocket. 2.2. Teeth mobilityTeeth mobility. Widening of periodontal ligament. Widening of periodontal ligament (thickening of lamina dura).(thickening of lamina dura). 3.3. Vertical bone defectsVertical bone defects without pockets.without pockets. However, if inflammation reaches the supporting tissues, itHowever, if inflammation reaches the supporting tissues, it is influenced by occlusion to change the environmentis influenced by occlusion to change the environment aggravating periodontal damage and bone resorption.aggravating periodontal damage and bone resorption.
- 47. 47 47 PrimaryPrimary OOcclusalcclusal TTrauma:rauma: Injury resulting fromInjury resulting from excessive occlusal forcesexcessive occlusal forces applied to aapplied to a tooth withtooth with normal periodontalnormal periodontal support.support. Response to traumatic occlusionResponse to traumatic occlusion occurs in 3 stages:occurs in 3 stages: Trauma → repair → change in morphology.Trauma → repair → change in morphology. In an effort to withstand these increased forcesIn an effort to withstand these increased forces,, adaptationadaptation occurs in the form ofoccurs in the form of bone resorptionbone resorption along the periodontal ligament leading toalong the periodontal ligament leading to increased mobility in aincreased mobility in a healthy toothhealthy tooth.. Once the periodontal ligament widens to the point ofOnce the periodontal ligament widens to the point of neutralising the forces, mobility and resorption are arrestedneutralising the forces, mobility and resorption are arrested i.e. increased but not increasing i.e. once the trauma isi.e. increased but not increasing i.e. once the trauma is removed mobility is arrested.removed mobility is arrested.
- 48. 48 Effects of traumatic occlusion:Effects of traumatic occlusion: 1.1. Alteration in occlusal forces.Alteration in occlusal forces. 2.2. Reduced capacity of periodontium to withstand occlusalReduced capacity of periodontium to withstand occlusal forces.forces. Causes of 1ry occlusal trauma:Causes of 1ry occlusal trauma: 1.1. Parafunctional habits s. a. clenching, grinding, tongueParafunctional habits s. a. clenching, grinding, tongue thrusting.thrusting. 2.2. Premature contacts caused by high restorations.Premature contacts caused by high restorations. 3.3. Orthodontic movements into unaccepted functionalOrthodontic movements into unaccepted functional position.position. 4.4. Teeth drifting due to unreplaced lost teeth.Teeth drifting due to unreplaced lost teeth. 5.5. Removable partial dentures that cause increased stress onRemovable partial dentures that cause increased stress on abutments.abutments.
- 49. 49 49 Treatment:Treatment: Removal of the cause of occlusal trauma to induce repair and promoteRemoval of the cause of occlusal trauma to induce repair and promote healing.healing. Alveolar bone loss, widening of periodontal membrane space andAlveolar bone loss, widening of periodontal membrane space and tooth mobility are reversible in non-plaque induced lesions.tooth mobility are reversible in non-plaque induced lesions. Methods of occlusal adjustment:Methods of occlusal adjustment: 1.1. The aim is to reduce forces and redirect them to the long axis.The aim is to reduce forces and redirect them to the long axis. 2.2. Controlling parafunctional habits.Controlling parafunctional habits. 3.3. Selective grinding (subtraction)Selective grinding (subtraction) 4.4. Occlusal cast restorations (addition)Occlusal cast restorations (addition) 5.5. Orthodontic treatment.Orthodontic treatment. SecondarySecondary OOcclusalcclusal TTrauma:rauma: A lesion created by normal function on a weakened periodontium dueA lesion created by normal function on a weakened periodontium due to periodontal disease.to periodontal disease.
- 50. 50 50 II.II. Mobility:Mobility: Normal teeth have a certain degree of mobility. SingleNormal teeth have a certain degree of mobility. Single rooted teeth are more mobile than multirooted teeth.rooted teeth are more mobile than multirooted teeth. Mobility is an indication of the loss of tooth attachment.Mobility is an indication of the loss of tooth attachment. Diagnosis of mobilityDiagnosis of mobility:: X-ray appears as widened periodontal ligament space.X-ray appears as widened periodontal ligament space. Clinically detected by pressing the tooth between a hardClinically detected by pressing the tooth between a hard object (e.g. mirror handle) and a finger.object (e.g. mirror handle) and a finger. Grades of mobilityGrades of mobility:: Grade 1……..Grade 1…….. Early, normal physiologic.Early, normal physiologic. Grade 2……..Grade 2…….. Abutment may need splinting and rigidAbutment may need splinting and rigid connectionconnection Grade 3…….Grade 3……. Mobile in all directions and depressible inMobile in all directions and depressible in its socket.its socket. ..
- 51. 51 Causes of mobility:Causes of mobility: 1.1. Occlusal traumaOcclusal trauma 2.2. Trauma due to accident.Trauma due to accident. 3.3. Periodontal involvement: increased bonePeriodontal involvement: increased bone resorption leading to mobility.resorption leading to mobility. 4.4. Parafunctional habits ex. continuous forcesParafunctional habits ex. continuous forces with no time for repairwith no time for repair
- 52. 52 52 III.III. Parafunctional habits:Parafunctional habits: Clenching, bruxism, nail biting, tongue thrusting induce excessiveClenching, bruxism, nail biting, tongue thrusting induce excessive lateral and horizontal forces which are destructive to thelateral and horizontal forces which are destructive to the periodontium and promote mobility.periodontium and promote mobility. Mesiodistal component of mobility is easier to reduce thanMesiodistal component of mobility is easier to reduce than buccolingual due to neighboring teeth which aid in anchorage.buccolingual due to neighboring teeth which aid in anchorage. Reduction of buccolingual mobility depends on the presence of firmReduction of buccolingual mobility depends on the presence of firm stable teeth in the splint.stable teeth in the splint.
- 53. 53 53 Sequence of Treatment of periodontally compromised patients:Sequence of Treatment of periodontally compromised patients: 1.1. Control of dental plaque by establishing adequate oral hygiene measuresControl of dental plaque by establishing adequate oral hygiene measures through tooth brushing, flossing and mouthwashes. (mechanical &through tooth brushing, flossing and mouthwashes. (mechanical & chemical )chemical ) 2.2. Scaling and Polishing.Scaling and Polishing. 3.3. Correction of any defective or overhanging restorations.Correction of any defective or overhanging restorations. 4.4. Root planningRoot planning 5.5. Removal of compromised teeth.Removal of compromised teeth. 6.6. Occlusal adjustment.Occlusal adjustment. 7.7. Stabilization of mobile teeth through splinting.Stabilization of mobile teeth through splinting. 8.8. Surgical therapy to promote bone induction if needed.Surgical therapy to promote bone induction if needed. 9.9. Treatment of furcation involvement including odontoplasty andTreatment of furcation involvement including odontoplasty and osteoplasty.osteoplasty. 10.10. Temporary restorations till the active phase of the therapy is concluded.Temporary restorations till the active phase of the therapy is concluded. 11.11. Final restorations.Final restorations.
- 54. 54
- 55. 55 55 3. Correction of any defective3. Correction of any defective or overhanging restorations.or overhanging restorations.
- 56. 56 56 7. Splinting:7. Splinting: 1.1. Occlusal adjustment.Occlusal adjustment. 2.2. Stabilization of mobile teeth through splinting.Stabilization of mobile teeth through splinting. It is the process of joining two or more teeth together for the purpose ofIt is the process of joining two or more teeth together for the purpose of stabilization.stabilization. 1.1. Occlusal adjustment.Occlusal adjustment. 2.2. Stabilization of mobile teeth through splinting.Stabilization of mobile teeth through splinting. Factors affecting the number of teeth required to stabilize a looseFactors affecting the number of teeth required to stabilize a loose tooth:tooth: 1.1. Depends on the grade and direction of mobility, the more theDepends on the grade and direction of mobility, the more the mobility, the greater the number of stable teeth needed.mobility, the greater the number of stable teeth needed. 2.2. Amount of remaining bone.Amount of remaining bone. 3.3. Position of the tooth in the arch. Ex Posterior mobile abutmentsPosition of the tooth in the arch. Ex Posterior mobile abutments require additional abutments in the design.require additional abutments in the design. 4.4. Whether it is used as an abutment.Whether it is used as an abutment.
- 57. 57 57 Functions of splinting:Functions of splinting: 1.1. The purpose of splinting is toThe purpose of splinting is to stop mobility or arreststop mobility or arrest its increaseits increase.. 2.2. ToTo protect loose teeth from injury duringprotect loose teeth from injury during stabilization in a favorablestabilization in a favorable occlusal relationship and promote an environment for bone healing.occlusal relationship and promote an environment for bone healing. 3.3. ToTo redistribute occlusal forces over large no of teethredistribute occlusal forces over large no of teeth weakened byweakened by loss of periodontal support. Thus a single rooted teeth function as multi-loss of periodontal support. Thus a single rooted teeth function as multi- rooted teeth.rooted teeth. 1.1. ToTo preventprevent natural teeth fromnatural teeth from migrating and super-eruptingmigrating and super-erupting.. 2.2. It is common use in conjunction with implants.It is common use in conjunction with implants. 3.3. Stabilization of teeth during and after trauma.Stabilization of teeth during and after trauma. 4.4. ToTo prevent lateral forcesprevent lateral forces which are destructive to the periodontium.which are destructive to the periodontium. 5.5. Centre of rotationCentre of rotation is transferred to the middle third.is transferred to the middle third.
- 58. 58 58 Methods of splintingMethods of splinting:: Splinting maybe temporary or permanent.Splinting maybe temporary or permanent. 1. Temporary, reversible and provisional splint.1. Temporary, reversible and provisional splint. Temporary splinting may or may not be followed withTemporary splinting may or may not be followed with permanent splinting. It provides a better chance topermanent splinting. It provides a better chance to periodontal tissues and alveolar bone to mature afterperiodontal tissues and alveolar bone to mature after periodontal therapy or orthodontic treatment. If after 6-8periodontal therapy or orthodontic treatment. If after 6-8 weeks the teeth stabilize, no further splinting is required.weeks the teeth stabilize, no further splinting is required. Types:Types: Ligature wireLigature wire,, A-splint or circumferential wiresA-splint or circumferential wires.. Rarely used and involve wrapping wire around the teeth, tying it andRarely used and involve wrapping wire around the teeth, tying it and covering it with acrylic.covering it with acrylic.
- 59. 59 59 2. Bonding ;2. Bonding ; Composite resin has greater strength, and the light cured bonding allowsComposite resin has greater strength, and the light cured bonding allows better control of the contours.better control of the contours. Temporary splinting is accomplished with the composite material aloneTemporary splinting is accomplished with the composite material alone or in combination with extra and intra coronal wires or screen meshes.or in combination with extra and intra coronal wires or screen meshes. 3. Removable appliances.3. Removable appliances. Continuous clasp partial denture.Continuous clasp partial denture. A swing lock RPD. is rare because it can be damaging.A swing lock RPD. is rare because it can be damaging. Orthodontic retainer.Orthodontic retainer.
- 60. 60 60 3. Provisional splinting with full-coverage acrylics Commonly used with periodontally compromised patients. Before periodontal treatment, the teeth are prepared and heat processed acrylic treatment restorations are constructed and cemented with sedative cement. These splints are then removed, periodontal therapy performed, and the splints replaced and left for 6-8 weeks. When tissue has healed after surgery, cast splints are inserted.
- 61. 61 61 bb. Permanent splint. Permanent splint:: Permanent splint can be performed usingPermanent splint can be performed using Fixed partial denture with rigid connectorsFixed partial denture with rigid connectors Resin bonded retainersResin bonded retainers Pinledge retainersPinledge retainers
- 62. 62 62 Occlusal morphology of the splints: should modify the occlusal table to establish occlusal adjustment by reducing cuspal inclines, reshaping cusps to eliminate lateral forces by guiding forces to fall within the peripheral contours of the root retained in alveolar bone thus influencing the direction of the transmitted forces upon the periodontium.
- 63. 63 63 Parafunctional habits and splinting:Parafunctional habits and splinting: Single or multiple mobile teeth with enough bone support in a patientSingle or multiple mobile teeth with enough bone support in a patient with parafunctional habits should not be splinted together.with parafunctional habits should not be splinted together. Occlusal correction should be done and an appliance such as a nightOcclusal correction should be done and an appliance such as a night guard should be done.guard should be done. If the forces are corrected, mobility should be reversed.If the forces are corrected, mobility should be reversed. However, if these teeth are splinted to stable teeth without correction ofHowever, if these teeth are splinted to stable teeth without correction of the cause of occlusal trauma the entire arch may become mobile.the cause of occlusal trauma the entire arch may become mobile. Prognosis:Prognosis: More root length has better prognosis. C: Root ratioMore root length has better prognosis. C: Root ratio Decreased cuspal inclines to decrease occlusal forces.Decreased cuspal inclines to decrease occlusal forces. Cusp position and restoration contour to reduce lateral forces outsideCusp position and restoration contour to reduce lateral forces outside root surface. ( 0.5 – 0.75 mm)root surface. ( 0.5 – 0.75 mm) Multirooted teeth have better prognosis than single rooted teeth.Multirooted teeth have better prognosis than single rooted teeth. Disadvantages of splinting:Disadvantages of splinting: We use additional number of abutments to replace missing teeth, thusWe use additional number of abutments to replace missing teeth, thus restorations face more complications such as deflection, path ofrestorations face more complications such as deflection, path of insertion, caries, removal if needed….insertion, caries, removal if needed….
- 64. 64 64 Preparation modification for periodontally involved teeth:Preparation modification for periodontally involved teeth: Location of F.L. in exposed roots:Location of F.L. in exposed roots: Often after surgical periodontal treatment part of the root is exposed.Often after surgical periodontal treatment part of the root is exposed. Some authors advocateSome authors advocate ending the preparation at the C.E. junctionending the preparation at the C.E. junction andand leaving the root uncovered.leaving the root uncovered. Others terminate the preparation on the root especially in case of rootOthers terminate the preparation on the root especially in case of root sensitivity. A chamfer F.L. is placed with a metal gingival collar, assensitivity. A chamfer F.L. is placed with a metal gingival collar, as extension of ceramic veneer on the root requires a shoulder F.L. whichextension of ceramic veneer on the root requires a shoulder F.L. which will endanger the pulp and cause extensive destruction of the tooth.will endanger the pulp and cause extensive destruction of the tooth.
- 65. 65 65 RootRoot RResectionesection: (Radectomy): (Radectomy) It is the removal of a root of a tooth.It is the removal of a root of a tooth. Root amputationRoot amputation:: It is the removal of a root without touching the crown.It is the removal of a root without touching the crown. The term tooth resection denotes the excision and removal of any segment of the tooth or a root with or without its accompanying crown portion. Various resection procedures described are : root amputation, hemisection,radisection and bisection HemisectionHemisection:: A procedure where the tooth is separated through the crown andA procedure where the tooth is separated through the crown and furcation, producing almost two equal teeth.furcation, producing almost two equal teeth.
- 66. 66 The term tooth resection denotes the excision and removal of any segment of the tooth or a root with or without its accompanying crown portion. Various resection procedures described are : root amputation, hemisection, radisection and bisection Root amputation refers to removal of one or more roots of multirooted tooth while other roots are retained. Hemisection denotes removal or separation of root with its accompanying crown portion of mandibular molars. Radisection is a newer terminology for removal of roots of maxillary molars. Bisection / bicuspidization is the separation of mesial and distal roots of mandibular molars along with its crown portion,where both segments are then retained individually2.
- 67. 67 67 IndicationsIndications:: The aim is to improve the prognosis of the involved root beingThe aim is to improve the prognosis of the involved root being resectioned by salvaging the healthy part and thus indirectly improveresectioned by salvaging the healthy part and thus indirectly improve the survival chance of the adjacent and neighbouring teeth.the survival chance of the adjacent and neighbouring teeth. 1.1. Severe vertical bone loss in one root.Severe vertical bone loss in one root. 2.2. Root removal or hemisection may change furcation anatomy to aid inRoot removal or hemisection may change furcation anatomy to aid in cleaning where embrasure space is obliterated.cleaning where embrasure space is obliterated. 3.3. Resection may save teeth where endodontic failure has occurred inResection may save teeth where endodontic failure has occurred in some roots e.g. extensive caries, instrument fracture.some roots e.g. extensive caries, instrument fracture. 4.4. Reduces the risk of lesion extension to the surviving roots.Reduces the risk of lesion extension to the surviving roots. Contraindications:Contraindications: Insufficient remaining bone to support the roots.Insufficient remaining bone to support the roots. No resection on maxillary first premolar.No resection on maxillary first premolar.
- 68. 68 68 Tooth Preparation and Crown Modification in Resected Roots:Tooth Preparation and Crown Modification in Resected Roots: These teeth have fewer loads bearing ability due to diminishedThese teeth have fewer loads bearing ability due to diminished attachment area. However, they may be used asattachment area. However, they may be used as abutments for fixed P.D., splints or vertical stops forabutments for fixed P.D., splints or vertical stops for cantilever F.P.D.cantilever F.P.D. Endodontic treatment usually precedes resectionEndodontic treatment usually precedes resection Preparation:Preparation: Any ridges (lips) found during preparation should be smoothened.Any ridges (lips) found during preparation should be smoothened. The F.L. should extend apically beyond the pulp chamber but notThe F.L. should extend apically beyond the pulp chamber but not necessarily covering other areas exposed by root removal.necessarily covering other areas exposed by root removal. Often, if (crown) is sound but the tooth only periodontally involvedOften, if (crown) is sound but the tooth only periodontally involved the pulp chamber may be filled with amalgam and a post is not needed.the pulp chamber may be filled with amalgam and a post is not needed. In other cases a post & core maybe needed to restore the tooth.In other cases a post & core maybe needed to restore the tooth.
- 69. 69 69 Teeth with Furcation involvementTeeth with Furcation involvement FurcationFurcation:: It is the site where the common root trunk divides into twoIt is the site where the common root trunk divides into two or three roots. In cases where the F.L. approaches theor three roots. In cases where the F.L. approaches the furcation the design of the preparation (and the crown)furcation the design of the preparation (and the crown) must be modified, due to intersection of the F.L with themust be modified, due to intersection of the F.L with the concavity in the root trunk (flute).concavity in the root trunk (flute). This concavity extends from the furcation to the CEJ.This concavity extends from the furcation to the CEJ. ie .Fluting.ie .Fluting. .. A. Max facial furcation B. Mand first molar
- 70. 70 PreparationPreparation:: Axial surface of the preparation occlusal to theAxial surface of the preparation occlusal to the inversion of the finish line must have ainversion of the finish line must have a concavity. Facial and lingual furcations are 3-4concavity. Facial and lingual furcations are 3-4 mm apical to the CEJ on mandibular molars.mm apical to the CEJ on mandibular molars. Flutes on maxillary molars are less seen as theirFlutes on maxillary molars are less seen as their indication is a sign of increased bone lossindication is a sign of increased bone loss
- 71. 71
- 72. 72 72
- 73. 73 73 The artificial crown should recreateThe artificial crown should recreate the contours of thethe contours of the furcation flutefurcation flute and not the original crown contour.and not the original crown contour. The facial surface should possess the concavity above theThe facial surface should possess the concavity above the bifurcation that extends occlusally until it meets the facialbifurcation that extends occlusally until it meets the facial groove in the occlusal third of the facial surface, and blendsgroove in the occlusal third of the facial surface, and blends into the occlusal surface. If the concavity does not extend allinto the occlusal surface. If the concavity does not extend all the way a plaque retaining area will develop.the way a plaque retaining area will develop.
- 74. 74 74 Tooth preparation & Crown Configuration:Tooth preparation & Crown Configuration: 1. Palatal Root Resection:1. Palatal Root Resection: Fig showing Maxillary palatal root resection, reduction & restorationFig showing Maxillary palatal root resection, reduction & restoration
- 75. 75 75 2.2. Distofacial Root Resection:Distofacial Root Resection: Distofacial root resection of a maxillary molar
- 76. 76 76 III. Mesobuccal Root Resection:III. Mesobuccal Root Resection: Sectioning is done at 45Sectioning is done at 4500 to the trunk.to the trunk. Crown preparation and restoration on a maxillary molar with no distofacial root
- 77. 77 77 IV. Mandibular molars:IV. Mandibular molars: a. Mandibular Hemisectiona. Mandibular Hemisection:: One root may be removed while the other is preserved.One root may be removed while the other is preserved. Mesial root resection Root Separation: Maybe accomplished orthodontically. Interradicular shoulders on the crown preparations.
- 78. 78 Hemisection of the distal root Bridge replacing resected distal root
- 79. 79 79
- 80. 80 80
- 81. 81 81 b. Bicuspidisation: The molar may be split and both roots maintained. However, they should be separated from each other to establish normal embrasure space and allow proper access to hygiene measures.
- 82. 82
- 83. 83 83
- 84. 84 84 Prognosis:Prognosis: 55% failure occurs within 5-7 years.55% failure occurs within 5-7 years. Failure is mostly endodontic or restorative in natureFailure is mostly endodontic or restorative in nature rather than periodontic failure, often seen as rootrather than periodontic failure, often seen as root fracture especially infracture especially in mandibular molars.mandibular molars. Maxillary molarsMaxillary molars have better prognosis due to thehave better prognosis due to the presence of at least two roots which provide morepresence of at least two roots which provide more support and stability.support and stability. For better prognosis:For better prognosis: 1.1. Occlusal scheme should be canine protected.Occlusal scheme should be canine protected. 2.2. Flatten posterior cusps.Flatten posterior cusps. 3.3. Restoration is designed to promote periodontal health,Restoration is designed to promote periodontal health, ex wide embrasure space, flat emergence profile.ex wide embrasure space, flat emergence profile.
