Bone destruction Periodontics *(ViRa)*
- 1. .
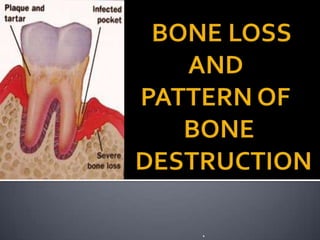
- 4. The bone that forms and supports the tooth is called ALVEOLAR PROCESS Destruction of the bone is responsible for tooth loss. As the tooth is shed this bone resorbs
- 5. Facial and lingual compact bone Socket wall consist of dense lamellated bone and bundle bone Interdental septum consist of cancellous bone.
- 6. Average distance of alveolar bone and Cemento-enamel junction: Young Adult: 0.75mm - 1.49mm Old age: 1.08mm – 2.81mm Mesiodistal angulation of crest of interdental septum usually parallels a line drawn between Cementoenamel junction of approximating teeth.
- 11. Centers of Ossification Centers of Ossification
- 14. The height and density of alveolar bone is normally maintained by an equilibrium, regulated by loacal and systemic factors between bone resorption and bone formation When this resorption exceeds formation both bone height and density are reduced. In periodontal disease, even the bone morphology is altered.
- 16. BONE DESTRUCTION PATTERN Horizonal bone loss Bone deformities Vertical or angular defect Osseous craters Bulbous bone contour Reversed architecture Ledges Furcation involvement FACTORS CAUSING DESTRUCTION OF BONE Extension of gingival inflammation Trauma from occlusion Systemic disorders FACTORS DETERMINIG BONE MORPHOLOGY Normal variation in alveolar bone Exostoses Trauma from occlusion Buttressing bone formation Food impaction Aggressive periodontitis
- 17. The most common pathway The inflammatory invasion of bone surface and the initial bone loss marks the transition from gingivitis to periodontitis. This transition is associated with changes in composition of bactrerial host and resistance og host. In advances stages of disease, the number of motile organism and spirochete increases, whereas the coccoid rods and straight rods decreases. The lesion presents with most pathogenic bacteria, inflammatory cell infiltrate, lesion becoming more destructive with conversion of T- lymphocyte to B-lymphocytic lesion.
- 18. 1. Interproximally from gingiva into bone 2. From bone into periodontal ligament 3. From gingiva into periodontal ligament
- 19. 1. Facially and lingually from gingiva along the outer periosteum. 2. From periosteum into bone 3. From gingiva into periodontal ligament
- 20. Gingival inflammation Marrow spaces Replaced by leucocytes and fluid exudates, new blood vessels and proliferating fibroblasts Increase in osteoclasts and mononuclear cells Thinning of bone trabeculae and enlargement of marrow spaces Destruction of bone and reduction of bone height Replacement of fatty bone marrow with fibrous type
- 21. Area of inflammation extends from gingiva into suprabony area. Extension of inflammation occurs along blood vessels and between collagen bundles. Inflammation extending from pocket area between collagen fibres, which are partially destroyed. Extension of inflammation into centre of interdental septum. Inflammation from gingiva penetrates transseptal fibres and enters the bone around blood vessels in the centre of septum. Cortical layer at the top of septum are destroyed and inflammation penetrates into bone marrow. Re-formation of trans-septal fibres. Recreated transseptal fibres above the bone margin, partially infiltrated by inflammatory process. Extension of inflammation to crestal bone surface.
- 22. 1.5 to 2.5mm within which a bacterial plaque can induce loss of bone. For interproximal angular defect space have to be greater than 2.5 mm because in narrow spaces bone is entirely destroyed leading to horizontal bone defects. Large defects exceeding 2.5mm can be seen in localised juvenile periodontitis and Pappilon-lefevre syndrome
- 23. in individual with no oral hygiene facial surface: 0.2mm a year proximal surface: 0.3 mm a year Bone loss may vary depending on the type of disease present. Rapid progression 8% Loss of attachment of 0.1 to 1.0mm Moderate progression 81% Loss of attachment of 0.05mm to 0.5mm Minimal or no progression 11% 0.05mm to 0.09mm yearly
- 24. Occurs in episodic, intermittent manner with period of inactivity or quiescence. Results in loss of collagen and alveolar bone resulting in deepening of periodontal pocket. The reason for onset, not elucidated. Some theories have been put forward
- 25. subgingival ulceration and an acute inflammatory reaction, resulting in rapid loss of alveolar bone. this coincides with the conversion of a predominantly Tlymphocyte lesion to one with a predominantly Blymphocyte–plasma cell infiltrate. Microbiologically they are associated with an increase of the loose, unattached, motile, gram-negative, anaerobic pocket flora, while periods of remission coincide with the formation of a dense, unattached, nonmotile, gram-positive flora with a tendency to mineralize. the onset of periods of destruction coincide with tissue invasion by one or several bacterial species and is followed by an advanced local host defense that controls the attack.
- 26. (a) bacterial (b) host mediated. Bacterial plaque products induce the differentiation of bone progenitor cells into osteoclasts and stimulate gingival cells to release mediators that have the same effect. Plaque products and inflammatory mediators can also act directly on osteoblasts or their progenitors, inhibiting their action and reducing their numbers. In addition, in rapidly progressing diseases such as aggressive periodontitis, bacterial microcolonies or single bacterial cells have been found between collagen fibers and over the bone surface, suggesting a direct effect. Several host factors released by inflammatory cells are capable of inducing bone resorption in vitro and play a role in periodontal disease. These include host-produced prostaglandins and their precursors, interleukin-1α (IL-1α) and IL-β, and tumor necrosis factor alpha (TNF-α). When injected intradermally, prostaglandin E2 (PGE2) induces the vascular changes seen in inflammation; when injected over a bone surface, PGE2 induces bone resorption in the absence of inflammatory cells and with few multinucleated osteoclasts. In addition, nonsteroidal antiinflammatory drugs (NSAIDs), such as flurbiprofen and ibuprofen, inhibit PGE2 production, slowing bone loss in naturally occurring periodontal disease in beagle dogs and humans. This effect occurs without changes in gingival inflammation and rebounds 6 months after cessation of drug administration.
- 29. Normal variation in alveolar bone: The anatomic feautres that affect bone destructive pattern in periodontal disease includes: The thickness,width and crestal angulation of interdental septa The thickness of facial and lingual alveolar plates Presence of fenestrations and dehiscences The alignment of teeth Root and root trunk anatomy Root position within the alveolar process Proximity with another tooth surface
- 30. Exostoses are outgrowths of bone Of varied size and shape. Palatal exostoses have been found in 40% of human skulls. They can occur as small nodules, large nodules, sharp ridges, spike-like projections, or any combination of these. Exostoses have been described in rare cases «is developing after the placement of free gingival grafts
- 31. Trauma from occlusion may be a factor in determining the dimension and shape of bone deformities. It may cause a thickening ol the cervical margin of alveolar bone or a change in the morphology of the bone on which inflammatory changes will later be superimposed
- 32. Bone formation sometimes occurs in an attempt to buttress bony trabeculae weakened by resorption. When it occurs within the jaw, it is termed central buttressing bone formation. When it occurs on the external surface, it is referred to as peripheral buttressing bone formation. The latter may cause bulging of the bone contour, termed lipping, which sometimes accompanies the production of osseous craters and angular detects
- 33. Interdental bone defects often occur where proximal contact is abnormal or absent. Pressure and irritation from food impaction contribute to the inverted hone architecture. In some instances the poor proximal relationship may be the result of a shift in tooth position because of extensive bone destruction preceding food impaction
- 34. Horizontal bone loss Vertical or angular defect Osseous defects Osseous craters Bulbous bony contours Reversed architecture Ledges Furcation involvement
- 35. The most common pattern Bone is reduced in height Bone margins remain perpendicular to tooth surface Interdental septa, facial and lingual cortical plates are affected.
- 37. Occur in adults Have been reports in skulls with primary dentition.. Presence is suggested on radiographs Careful probing and surgical exposure of areas is required.
- 38. Occur in oblique direction Leaves a hollowed out trough in the bone alongside root Base of defect is apical to the surrounding bone. Angular defect and intrabony periodontal pocket Classified on basis of number of walls: one wall defect two walled defect three walled defect combined osseous defect
- 39. Three bony walls Combined osseous defect Two wall defect One wall defect
- 41. Concavities in the crest of alveolar bone Confined to facial and lingual walls Resons for high frequency interdental craters: interdentally area collects plaque and is difficult to clean. The normal flat or even concave faciolingual shape of interdental septum in lower molars favours plaque formation. Vascular patterns from gingiva to crest-pathway for inflammation.
- 42. Bony enlargements caused by exostoses, adaptation to function or buttressing bone formation. Maxilla> Mandible
- 43. Defects produced by loss of interdental bone Includes facial plates and lingual plates without concomitant loss of radicular bone. Maxilla more common
- 44. These are plateau like bone margins caused by resorption of thickened bony plates.
- 45. It refers to the involvement of bifurcations and trifurcations of multirooted teeth by periodontal disease. Most common in mandibular molars. Least common in maxillary premolar. Furcation anatomy: area of root separation Surface coronal to root separation Root furcation
- 46. GRADEI : Also called as early lesion. Suprabony pocket involving soft tissue Radiographic changes not usually found as bone loss is minimal, but increase in probing depth GRADEII: Bone destroyed in one or more surfaces of furcation Part of PDL, alveolar bone remains intact, allows partial penetration of bone. Radiograph may or may not show presence
- 47. GRADEIII : Interradicular bone completely missing. Facial and lingual or both orifices of furation canot be seen clinically because of soft tissue coverage. Bone loss crater like or angular. Radiograph at proper angulation shows furcation. GRADE I V: Clinically visible if gingival reseccion is present. Radiograph reveals easy furcation involvement
- 48. DEGREE I: Horizontal bone loss less than 3mm DEGREE II: Horizontal bone loss more than 3mm DEGREE III: through and through horizontal lesion Vertical bone loss is measured in mm from the roof of the furcation Subclass A: Vertical destruction to one-third of total radicular height (1-3mm) Subclass B: Vertical destruction reaching two-third of inter-radicular height (4-6mm) Subclass C: Inter-radicular osseous destruction into or beyond apical third (>7mmm)
- 50. Mandibular Molars Buccal Furcation Place the probe between the two buccal roots from the buccal aspect Mandibular Molars Lingual Furcation Place the probe between the two lingual roots from the lingual aspect
- 51. Should include both periapical and bitewing Location of the interdental bone and bone level within the root complex should be examined
- 53. THANK YOU..
