1357.full
- 1. Critical Care and Trauma Section Editor: Jukka Takala Continuous Airway Access for the Difficult Extubation: The Efficacy of the Airway Exchange Catheter Thomas C. Mort, MD BACKGROUND: The American Society of Anesthesiologists Task Force on the Man- agement of the Difficult Airway regards the concept of an extubation strategy as a logical extension of the intubation process, although the literature does not provide a sufficient basis for evaluating the merits of an extubation strategy. Use of an airway exchange catheter (AEC) to maintain access to the airway has been reported on only a limited basis. METHODS: I reviewed an observational analysis of a prospectively collected difficult airway quality improvement database for patients who were extubated over an AEC for a known or presumed difficult airway primarily in the intensive care unit. The data were reviewed for time to reintubation, number of attempts to reintubate the trachea, method of securing the airway, incidence of hypoxemia during reintubation, and complications encountered during reestablishment of the airway. RESULTS: Fifty-one patients with an indwelling AEC failed their extubation trial. Forty-seven of 51 AEC patients were successfully reintubated over the AEC (92%), with 41 of 47 on the first attempt (87%). In three of the four AEC reintubation failures, the AEC was inadvertently removed from the glottis during the reintuba- tion process, and one patient had significant laryngeal edema precluding endotra- cheal tube advancement. CONCLUSIONS: Maintaining continuous access to the airway postextubation via an AEC can be an important component of an extubation strategy in selected difficult airway patients. The indwelling AEC appears to increase the first-pass success rate in patients with known or suspected difficult airways and decrease the incidence of complications in patients intolerant of extubation and requiring tracheal reintubation. (Anesth Analg 2007;105:1357–62) “A irway management” comprises care of the pa- tient during tracheal intubation, maintenance of the improve patient safety (2). Therefore, maintaining a conduit within the trachea that affords the ability to endotracheal tube (ETT) in situ, and extubation, with resecure the airway may serve as the central point of a continued control of the airway into the postextuba- preformulated extubation strategy (1). tion period. The American Society of Anesthesiolo- Airway exchange catheters (AEC) have been used gists Task Force on the Management of the Difficult to more safely change ETT as well as to maintain Airway regards the concept of an extubation strategy access to the airway after extubation, thus allowing a as a logical extension of the intubation process. Cur- reversible extubation if needed (3– 6). Successful rein- rent literature does not provide a sufficient basis for tubation of the trachea with an AEC for a difficult evaluating the merits of an extubation strategy (1), and extubation is not a new concept, yet reports of this most efforts have been expended on addressing strat- practice have been limited. Three separate groups egies, safety concerns and techniques for intubating reviewed 278 difficult extubation patients, but only 29 the trachea, with relatively little attention paid to patients required attempted reintubation over the extubation. Further, the Closed Claim Analysis for AEC. Details of the tracheal reintubation were pro- difficult airway management concluded that the de- vided in only 4 of the 29 AEC-assisted reintubation velopment of management strategies covering emer- attempts, and no complications were reported (6). gence and the recovery phase after extubation may Published complications related to the AEC have been From the *Department of Anesthesiology, Simulation Center, Hartford more plentiful than reports touting the AEC’s role in Hospital, Hartford; and †Department of Anesthesiology, University of maintaining access during the clinician’s most difficult Connecticut School of Medicine, Farmington, Connecticut. airway encounters; hence, the literature offers few details Accepted for publication July 17, 2007. regarding its reintubation success on a larger scale There are no conflicts of interest to be disclosed by the author regarding this manuscript. (7–13). Extubation intolerance (failure) is relatively un- Address for correspondence and reprint requests to Thomas C. common in the elective operating room (OR) patient, but Mort, MD, Department of Anesthesiology, 80 Seymour St., Hartford the critically ill intensive care patient suffers extubation Hospital, Hartford, CT 06015. Address e-mail to tmort@harthosp.org. failure regularly (0.4%–25%) (14 –24). Copyright © 2007 International Anesthesia Research Society Patients with a known or suspected difficult airway DOI: 10.1213/01.ane.0000282826.68646.a1 represent a patient cohort who may benefit from an Vol. 105, No. 5, November 2007 1357
- 2. extubation strategy involving reversible extubation complications encountered during reestablishment of (14 –21). This is the first report to provide details, in a the airway. Hypoxemia was defined as a desaturation relatively large cohort of difficult airway patients, on nadir of Spo2 Ͻ90% and severe hypoxemia as Spo2 the reintubation first-pass success rate, reasons for Ͻ70%. Reintubation of the patient’s trachea was indi- reintubation failure, and any complications associated vidualized for each patient and at the discretion of the with reestablishment of the airway after extubation. ICU and anesthesia teams. Typically, shortness of Further, this is the first report describing extensive use breath, tachypnea, worsening oxygen saturations, stri- of both the smaller adult 11F and the medium-sized dor, increased work of breathing, and failure of pul- adult 14F AEC. monary toilet despite therapeutic assistance by the nursing and respiratory therapy staff contributed to the decision for reintubation. METHODS Data were analyzed using SPSS 12 (SPSS Inc., In an observational analysis, a difficult airway Chicago, IL). The contingency 2 test was used for quality improvement database was reviewed for pa- categorical variables in comparing complications be- tients who were extubated over an AEC for a known tween patients with and without the AEC in place yet or presumed difficult airway in the OR, the postanes- requiring reintubation of the trachea. Statistical sig- thesia care unit (PACU), or the intensive care unit nificance was accepted at P Ͻ 0.05. (ICU). Data were collected by the author prospectively and entered into a Microsoft Excel spreadsheet (1998 –2002); then, the database was transferred to and RESULTS maintained in an SPSS statistical package data sheet In the review period, 354 patients with a known or (2002–2006). Patients were cared for directly by the suspected difficult airway, based on previous airway author or by members of the anesthesia airway team. encounters and current physical examination, had If observation of postextubation patients extended access to their trachea maintained by an indwelling beyond regular working hours (evening and night AEC after extubation. Other methods of staged extuba- shifts), the author collected and verified data through tion (transition from ETT to laryngeal mask airway ICU care team interviews and review of the medical [LMA] or bronchoscopic-assisted extubation) were rela- records. The hospital’s IRB waived the need for in- tively few in the ICU setting and were not reviewed. formed consent. After extubation over an AEC, each patient re- Over a 9-yr period, 354 patients were extubated mained in a monitored environment (the ICU setting, with a Cook AEC (3.7 mm E.D.-11F, 4.7 mm-14F or 6.3 the PACU, or transition from the OR to the PACU). mm-19F, Cook Critical Care, Bloomington, IN) left in The AEC remained in place for a mean of 3.9 h (range, the trachea for a potential reversible extubation as part 5 min to 72 h). All patients in the first group who of a staged extubation strategy. The AEC remained in underwent an AEC-assisted reintubation did so the trachea until reintubation was considered unlikely within 24 h after extubation. The second group did not for each individual patient by the ICU and anesthesia have the AEC in position at the time of their reintu- airway team. Reintubation of the trachea was man- bation. The AEC size used for the extubation varied: aged by the anesthesia airway team (an anesthesia 11F (151 patients typically Ͻ5Ј5Љ tall, 46%), 14F (165 attending physician alone or an anesthesia resident patients typically taller than 5Ј5Љ, 50%) and 19F (13 [CA-2, CA-3] directly supervised by the attending patients taller than 5Ј10Љ, 4%). The location of staff) at the patient’s bedside. The anesthesia team the patient at the time of tracheal extubation included members’ experiences with reintubation over an in- the OR (17 postsurgical patients extubated at the dwelling AEC varied, although they routinely per- conclusion of their anesthesia), the PACU (24 postsur- formed tracheal intubation over a bougie airway catheter gical patients extubated after their transfer from the or tracheal tube exchanges over an AEC. OR to the PACU for postanesthesia recovery), and the Patient analysis was performed on the primary ICU (288 patients). Most of the ICU patients (75%) had group, which included patients with an indwelling been intubated for Ͼ48 h, and many were in the AEC, who required reintubation within 24 h and a recovery phase of resolving pneumonias, congestive secondary group of patients who had initially had an heart failure, tracheobronchitis, neuro/mental status indwelling AEC in the postextubation period but who alterations, and other maladies placing them at high then underwent removal of the AEC based on the risk for potential extubation failure. Seventy-two per- presumed tolerance of the extubated state. Patients in cent of the 354 patients had a known difficult airway the secondary group subsequently required reintuba- based on a history of difficult airway management tion within 7 days of tracheal extubation. These two requiring multiple conventional attempts (Ն3) or re- groups were reviewed for the time from extubation to quiring an accessory airway device to secure the reintubation, the number of attempts required to airway in the emergency room, the OR, or a remote reintubate the trachea (with and without the AEC in location intubation during the current hospitalization. place), the incidence of hypoxemia during reintuba- The remaining patients, 28%, had a suspected difficult tion, the method used to resecure the airway, and any airway based on their current physical examination 1358 Extubation of the Difficult Airway ANESTHESIA & ANALGESIA
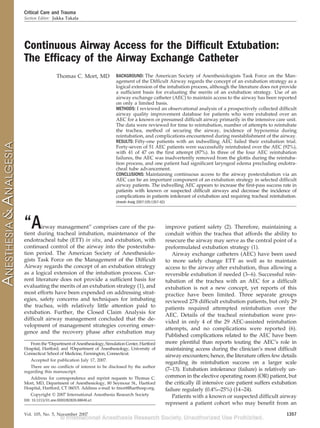
- 3. Table 1. Success Rate of Reintubation with AEC In Situ Table 2. Reintubation Technique in Patients Without an Airway Exchange Catheter (AEC)a (n ϭ 40) Overall success rate 92% (47 of 51 patients) 1st attempt 87% (41 of 47 patients) Direct laryngoscopy alone 3 (3ϩ attempts) 2nd attempt 11% (5 of 47 patients, requiring LMA/Fastrach LMA 20 downsizing of ETT) Flexible fiberoptic bronchoscope 6 3rd attempt 1 case (required downsizing of ETT) Rigid fiberscope (Bullard®, Shikani®) 4 4th attempt 1 case-failed despite progressive Tracheal tube introducer (bougie) 3 downsizing of ETT, Fastrach Surgical airwayb 4 LMA® rescue a Includes failed AEC intubation attempts, AEC migration (36 patients without AEC ϩ 4 failed AEC migration out 6% (3 cases) rescued with flexible AEC cases). of airway fiberscope-1 case, multiple b These four patients had successful ventilation/oxygenation achieved via bag-mask (1 case), attempts-1 case, Fastrach LMA-1 laryngeal mask airway (LMA) (2 cases) and the esophagotracheal Combitube® (1 case) but case could not be intubated via the glottis. AEC ϭ airway exchange catheter; ETT ϭ endotracheal tube; LMA ϭ laryngeal mask airway. by the resident/attending and one handled by the (airway-related swelling; edema or tissue trauma sec- attending physician alone. The relatively low failure ondary to surgery, infection or injury; intravascular rate did not allow statistical analysis to identify any volume resuscitation; systemic response to sepsis; differences between resident and attending staff. drug reaction or patient positioning, e.g., prone). Forty-one percent of the AEC-assisted reintubations Restriction in cervical range of motion or limited in 51 patients occurred within 2 h of the initial access to the airway due to injury, hard cervical collar, extubation, representing an overall rate of 6% (21 of a halovest or bandages/dressings were additional 354 patients). The remaining 30 extubation failures factors suggestive of potential difficult airway man- with an indwelling AEC occurred beyond 2 h postex- agement. Fifty-one patients had an indwelling AEC at tubation, primarily between 2 and 10 h. Once the the time of the reintubation procedure. decision to reintubate the trachea was made, admin- Forty-seven of 51 AEC patients had successful istration of oxygen was provided by bag-mask venti- AEC-assisted reintubation (92%, Table 1), with 41 of 47 lation in the majority of patients (44 of 51) by the on the first attempt and thus an 87% first-pass success anesthesia airway team, with the AEC lateralized to rate. Five patients required two attempts to pass the the corner of the mouth to optimize the mask seal. The ETT via the AEC, and one patient required three remaining seven patients had 3– 6 L of oxygen flow attempts (each with a smaller diameter ETT). Of the provided directly via the AEC, in lieu of bag-mask four AEC failures, three patients had the AEC inad- support. Direct administration of oxygen via the AEC vertently removed during the reintubation process, effectively kept the seven patients’ oxygen saturation and in the fourth patient the ETT could not be passed Ͼ90% in each case, but this method required a brief over the AEC despite progressive ETT downsizing, disconnection of oxygen flow during the initial pass- lubrication, and counterclockwise rotation of the ETT ing of the ETT over the indwelling AEC. High- (marked laryngeal edema noted by fiberoptic bron- pressure jet ventilation via the AEC was not used in choscopy during reintubation). Reintubation of these any of the cases. four patients included the Fastrach LMA™ in two Patient preparation for AEC-assisted reintubation patients, fiberoptic bronchoscopy in one patient, and included no medication or local anesthesia applied conventional laryngoscopy in one patient who re- topically to the upper airway (27%). The remaining quired four attempts. Seven patients suffered hypox- patients received light-to-moderate doses of sedative- emia, with mild desaturation (Spo2 Ͻ90%, n ϭ 3) or hypnotic drugs: midazolam 0.01– 0.02 mg/kg, 1–3 mg severe desaturation (Spo2 Ͻ70%, n ϭ 4), during the total (12% of patients), etomidate: 0.07– 0.17 mg/kg, reintubation process. Three of the 4 patients who 4 –14 mg total (34%), or propofol Ϫ0.4 to 1.4 mg/kg, developed severe hypoxemia were the AEC failures, 30 –130 mg total (27%). Reintubation of the trachea and each experienced bradycardia (Ͻ40 bpm) and was facilitated with laryngoscopy to open the orohy- concomitant hypotension during the reintubation pro- popharynx in three-quarters of the patients. The re- cess. Only two patients who underwent successful maining patients underwent manual jaw thrust/ AEC-assisted reintubation experienced severe reduc- lingual retraction to assist with ETT passage over the tion of the heart rate while resecuring the airway (one AEC. Only two patients received neuromuscular hypoxemia induced). blocking drugs to assist in the intubation procedure All reintubations were performed by an attending over the AEC; in the remaining patients, spontaneous anesthesiologist alone (n ϭ 23) or by an anesthesiology ventilation was maintained. resident under direct supervision of an attending Thirty-six patients (second group) required reintu- anesthesiologist (n ϭ 28). The attending alone and bation after their AEC had been removed. Eighteen of attending/resident groups had similar reintubation these 36 patients (50%) were intolerant of extubation success rates via the indwelling AEC. Three cases of within 120 min, 4 patients between 2 and 4 h, and 14 inadvertent AEC migration out of the trachea during patients succumbed to reintubation beyond 4 h. These the reintubation process occurred: two cases handled patients proved worthy of their designation as “known Vol. 105, No. 5, November 2007 © 2007 International Anesthesia Research Society 1359
- 4. Table 3. Complications of the Reintubation Procedure AEC present AEC absent (n )15 ؍ (n )63 ؍ P First-pass success rate for reintubation 87% 14% (5) Ͻ0.02 Hypoxemia during reintubation (Spo2 Ͻ90%) 8%b (4) 50% (18) Ͻ0.01 Severe hypoxemia during reintubation (Spo2 Ͻ70%) 6%a(3) 19% (7) 0.05 Bradycardia (heart rate Ͻ40) with hypotension 4% (2) 14% (5) Ͻ0.05 Multiple intubation attempts (Ն3) including the 10%b (5) 77% (28) Ͻ0.02 placement of an accessory airway device Esophageal intubation 0 18% (6) Rescue airway device/technique 6%a (3) 90% (32) Ͻ0.01 a Includes the AEC failures due to inability to pass ETT into trachea (1 case) and proximal migration of the AEC out of the trachea (3 cases). AEC ϭ airway exchange catheter; ETT ϭ endotracheal tube. or suspected difficult airway,” since the vast majority the skills and preferences of the practitioner (1). Rein- required multiple attempts to resecure the airway tubation of the trachea in the known or suspected (three or more attempts with laryngoscopy plus the difficult airway patient appears fraught with compli- accessory device/technique, 77%) when compared cations, as illustrated in this study by the group of with only one patient with the indwelling AEC who patients who underwent extubation of their trachea required three attempts. Table 2 illustrates the conven- over an AEC, had it subsequently removed when the tional and accessory airway devices that were re- reintubation risk was presumed to be low, yet later quired to assist the practitioner in resecuring the suffered extubation intolerance and were reintubated. patients’ airways. Postextubation hypoventilation, airway compro- The 14% first-pass reintubation success rate (first mise, ventilation-perfusion inequalities, and obstruc- attempt with direct laryngoscopy or accessory device) tion due to fatigue may afflict the patient in the OR, in in the non-AEC group was dwarfed by the AEC- the PACU, and in particular in the ICU (3,4). Continu- assisted first-pass success rate of 87% (Table 3). Nearly ous access to the airway can be maintained via an AEC all (90%) of the non-AEC group required an accessory with the proximal tip secured to the patient’s clothing airway device or an advanced technique to success- or forehead (waterproof adhesive tape). This is well fully reestablish the airway (Table 3). Of note, after tolerated by most patients (90%) and thus is a valuable failure to intubate the trachea in four patients, despite option, considering a reintubation rate that varies concerted attempts with accessory devices, a surgical from 0.4% to 25% in the various PACU and ICU airway was required. Two of these four patients populations (3–7,14 –21). received bag-mask ventilation during the establish- Currently, there are no evidence-based guidelines ment of the surgical airway, and two patients had regarding the optimal period of time for maintaining concurrent and successful ventilation and oxygen- airway access postextubation via an indwelling AEC. ation via an LMA during placement of the surgical Experts have suggested at least 30 – 60 min or until the airway. likelihood of reintubation is minimized (3,5,6,22–24). Oxygen desaturation in the non-AEC group was Unfortunately, our database suggests that a minimum common during the reintubation process, with the of 30 – 60 min would underestimate the need for a nadir of Ͻ90% Spo2 occurring in 50% of the patients; reversible extubation in a significant number of these 40% of these suffered severe hypoxemia (Spo2 Ͻ70%, high-risk patients. Moreover, the potential for changes Table 3). Esophageal intubation was more common in in the patient’s clinical status makes it difficult to the non-AEC group (18% to 0%), as was hypoxemia- predict when the need for reintubation is minimized. driven bradycardia with profound hemodynamic This may be particularly true in the ICU population, deterioration. Table 3 compares the various complica- who may suffer acute alterations in their cardiopul- tions of the reintubation procedure between those monary, metabolic, or neurological status, or other reintubated with and without an indwelling AEC. critical medical/surgical issues that may influence their tolerance of extubation. DISCUSSION If the intolerance of the extubated state is based In the high-risk extubation patient with known or principally on the presence or potential accumulation suspected airway management difficulties, develop- of periglottic edema, then the patient may benefit from ment of a strategy to maintain access to the airway and extending the duration of the indwelling AEC to to offer the safety of reversibility if the extubated state 60 –120 min. Periglottic edema contributing to airway is not tolerated should be considered (1). This strategy compromise often occurs immediately upon extuba- will depend, in part, on the surgical and medical tion or within 10 – 45 min of extubation, although it conditions of the patient, on the previous airway has been noted that symptomatic laryngeal edema procedures and current airway status, as well as on may develop as late as 8 h postextubation (14,15). 1360 Extubation of the Difficult Airway ANESTHESIA & ANALGESIA
- 5. Extending the duration of continuous airway access means other than the AEC. Immediate access to con- would seem prudent if the patient demonstrates car- ventional and advanced airway rescue devices and the diopulmonary pathology and other systemic illness. presence of competent and experienced airway Difficult airway patients who have failed an extuba- personnel capable of providing advanced airway tion trial are typically handled by determining the management in this difficult airway population are previous extubation time and then extending it by a imperative (25–32). factor of two- to three-fold to provide a reasonable The limitations of this data analysis are that it was cushion for maintaining access in the event of failure. neither a randomized nor a blinded evaluation of If mental or neurological status is compromised, espe- AEC-assisted extubation of the difficult airway pa- cially when coupled with cardiopulmonary limita- tient, nor did it compare one method of maintaining tions, then extending the time to 12–24 h or beyond airway access to another. Removal of the indwelling may provide a valuable safeguard. AEC was based on the clinical determination that the Even if the time devoted to maintenance of airway risk of reintubation was diminished; thus, it was access is extended, patients may still fail their extubation limited by the practitioner’s individual experience and trial well after removal of the AEC. Clearly, guidelines to judgment and the unpredictable nature of the patient’s assist the practitioner in decision-making are needed, clinical status. Some patients may have remained and further study to investigate the optimal duration of instrumented with the AEC longer than needed, the indwelling AEC appears warranted. whereas others may have prematurely lost the benefit Previous investigators who incorporated an airway of continuous airway access. catheter (3.7– 4 mm ED) found it was well tolerated, The optimal duration of continuous access to the affording reasonable comfort and allowing the pa- airway after extubation in this patient population was tients to retain the ability to phonate and generate a not directly tested. Beyond conjecture and the author’s secretion-clearing cough (3,6). The current database, experienced opinion, this data analysis provided non- again, reconfirms that the 11F (3.7 mm ED) is well definitive evidence-based findings to assist the practi- tolerated in over 90% of patients and may serve a key tioner in answering this important question. role in resecuring an airway in the difficult extubation In summary, this practice analysis reconfirms that patient. Moreover, the two larger sized AEC, the 14F the AEC is an efficient method of maintaining con- (4.7 mm ED) and the 19F (6.3 mm ED), which had not tinuous access to the airway after extubation, as it is been previously reported for the difficult extubation well tolerated and potentially offers a clinically valu- patient, were useful for maintaining access to the able conduit for reintubation, as reported by earlier, airway and reintubating the trachea for a reversible more limited reviews (3,4,6). Further, in the taller extubation in this study. In this database, the larger patient, the medium-sized AEC (14F, 4.7 mm ED) may 14F AEC, based on patient interviews postextubation, be a useful alternative to the smaller adult version had a relatively minor rate of patient discomfort (8%), (11F, 3.7 mm ED), as both sizes appear to be well similar to that of the smaller 11F AEC (7%). The largest tolerated by most patients. Complications of resecur- sized AEC (19F), although an excellent conduit for ing the airway in the known or suspected difficult reintubation or exchanging an ETT, had a significantly higher rate of patient discomfort (50%). Its use for airway are relatively common, especially when con- maintaining a reversible extubation has been curtailed tinuous airway access is not preserved. The optimal at the author’s institution due to this higher rate of time for maintaining access to the airway postextuba- discomfort and patient dissatisfaction. Although AEC- tion should be addressed in further studies. assisted reintubation of the trachea is not guaranteed, the 92% success rate of both sizes of AEC is excep- REFERENCES tional and compares favorably with the three previ- 1. American Society of Anesthesiologists Task Force on Manage- ously published studies reporting AEC-assisted ment of the Difficult Airway. Practice guidelines for the man- agement of the difficult airway: an updated report by the reintubation (27 of 29 attempts successful, 93%) (3,4,6). American Society of Anesthesiologists Task Force on Manage- The presence of the AEC to assist in reintubating ment of the Difficult Airway. Anesthesiology 2003;98:1269 –77 the trachea is a major step toward improving safety in 2. Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, the difficult airway patient. This is well illustrated by Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology 2005;103:33–9 a comparison of the complication rates of AEC- 3. Cooper RM. The use of an endotracheal ventilation catheter in assisted reintubations and tracheal extubations in the management of difficult extubations. Can J Anaesth difficult airway patients who had had their AEC 1996;43:90 –3 4. Dosemeci L, Yilmaz M, Yegin A, Cengiz M, Ramazanoglu A. removed before their declaration of extubation intol- The routine use of pediatric airway exchange catheter after erance (Tables 2 and 3). Despite this high success rate extubation of adult patients who have undergone maxillofacial for AEC-assisted reintubation, the practitioner and the or major neck surgery: a clinical observational study. Critical airway team must be prepared for the possibility that Care 2004;8:385–90 5. Cooper RM. Extubation and changing endotracheal tubes. In: the patient may fail the extubation trial and require Benumof J. ed. Airway management: principles and practice. St. emergent or urgent intubation of the trachea by a Louis: Mosby, 1995 Vol. 105, No. 5, November 2007 © 2007 International Anesthesia Research Society 1361
- 6. 6. Loudermilk EP, Hartmanngruber M, Stoltfus DP, Langevin PB. 19. Hines R, Barash PG, Watrous G, O’Connor T. Complications A prospective study of the safety of tracheal extubation using a occurring in the post-anesthesia care unit: a survey. Anesth pediatric airway exchange catheter for patients with a known Analg 1992;74:503–9 difficult airway. Chest 1997;111:1660 –5 20. Biancofiore G, Bindi ML, Romanelli AM, Boldrini A, Bisa M, 7. Benumof JL. Airway exchange catheters: simple concept, poten- Esposito M, Urbani L, Catalano G, Mosca F, Filipponi F. tially great danger. Anesthesiology 1999;91:342– 4 Immediate tracheal extubation following liver transplantation: 8. Baraka AS. Tension pneumothorax complicating jet ventilation fast track in liver transplantation: 5 years’ experience. Eur J via Cook airway exchange catheter. Anesthesiology 1999; Anaesthesiol 2005;22:584 –90 91:557– 8 21. Epstein SK. Preventing post-extubation respiratory failure. Crit Care Med 2006;34:1547– 8 9. DeLima L, Bishop M. Lung laceration after tracheal extubation 22. Hagberg C, ed. Handbook of difficult airway management. over a plastic tube changer. Anesth Analg 1991;73:350 –1 Philadelphia: Churchill Livingstone, 2000. Chapter 16: Extuba- 10. Seitz PA, Gravenstein N. Endobronchial rupture from endotra- tion of the difficult airway cheal reintubation with an endotracheal tube guide. J Clin 23. Miller K, Harkin C, Bailey PL. Postoperative tracheal extuba- Anesth 1989;1:214 –7 tion. Anesth Analg 1995;80:149 –72 11. Benumof JL, Gaughan SD. Concerns regarding barotrauma 24. Topf AI, Eclayea A. Extubation of the difficult airway. Anesthe- during jet ventilation. Anesthesiology 1992;76:1072–3 siology 1996;85:1213– 4 12. Fetterman D, Dubovoy A, Reay M. Unforeseen esophageal 25. Mort TC. Emergency tracheal intubation: complications associ- misplacement of airway exchange catheter leading to gastric ated with repeated laryngoscopic attempts. Anesth Analg perforation. Anesthesiology 2006;104:1111–2 2004;99:607–13 13. Bedger RC, Chang JL. A jet-stylet endotracheal catheter for 26. Rosenblatt WH. Preoperative planning of airway management difficult airway management. Anesthesiology 1987;66:221–3 in critical care patients. Crit Care Med 2004;32:186 –92 14. Darmon J, Rauss A, Dreyfuss D, Bleichner G, Elkharrat D, 27. Mort TC. The incidence and risk factors for cardiac arrest during Schlemmer B, Tenaillon A, Brun-Buisson C, Huet Y. Evaluation emergency tracheal intubation: A justification for incorporating of risk factors for laryngeal edema after tracheal extubation in the ASA Guidelines in the remote location. J Clin Anesth adults and its prevention by dexamethasone. Anesthesiology 2004;16:508 –16 1992;77:245–51 28. Le Tacan S, Wolter P, Rusterholtz T, Harlay M, Gayol S, Sauder 15. Ho L, Harn H, Lien T, Hu P, Wang J. Postextubation laryngeal P, Jaeger A. Complications of difficult tracheal intubations in a critical care unit. Ann Fr Anesth Reanim 2000;19:719 –24 edema in adults. Intensive Care Med 1996;22:933– 6 29. Mort TC. The importance of a laryngoscopy strategy and 16. Epstein SK, Ciubotaru RL. Independent effects of etiology of optimal conditions in emergency intubation. Anesth Analg failure and time to reintubation on outcome for patients failing 2005;100:900 (author reply to letter) extubation. Am J Respir Crit Care Med 1998;158:489 –93 30. Mort TC. Preoxygenation in critically ill patients requiring 17. Epstein SK. Decision to extubate. Intensive Care Med 2002; emergency tracheal intubation. Crit Care Med 2005;33:2672–5 28:535– 46 31. Dworkin R, Benumof JL, Benumof R, Karagianes TG. The 18. Esteban A, Frutos-Vivar F, Ferguson ND, Arabi Y, Apezteguia effective tracheal diameter that causes air trapping during jet C, Gonzalez M, Epstein SK, Hill NS, Nava S, Soares MA, ventilation. J Cardiothorac Anesth 1990;4:731– 6 D’Empaire G, Alia I, Anzueto A. Noninvasive positive-pressure 32. Asai T, Shingu K. Difficulty in advancing a tracheal tube over a ventilation for respiratory failure after extubation. N Engl J Med fiberoptic bronchoscope: incidence, causes and solutions. BJA 2004;350:2452– 60 2004;92:870 – 81 1362 Extubation of the Difficult Airway ANESTHESIA & ANALGESIA