Gastrocon 2016 - Drug Induced Liver Disease
- 1. DRUG INDUCED LIVER DISEASEDRUG INDUCED LIVER DISEASE S. P. SINGHS. P. SINGH
- 2. DEFINITIONDEFINITION The liver diseaseThe liver disease resulting from the inhalation,resulting from the inhalation, ingestion or parenteral administrationingestion or parenteral administration of anyof any pharmacological or chemical agent is called drugpharmacological or chemical agent is called drug induced liver diseaseinduced liver disease (DILD)(DILD)
- 3. DRUG HEPATITIS !DRUG HEPATITIS ! DILIDILI [Drug Induced Liver Injury]?[Drug Induced Liver Injury]?
- 4. Drug Induced Liver DisordersDrug Induced Liver Disorders • When Liver Biopsy has been performed: lesion should be named according to histological findings, e.g. ‘cirrhosis’, ‘CLD’,’hepatic necrosis’ or ‘hepatitis’. • In the absence of histological data: such terms should not be used. The preferred term is “liver injury”. CIOMS
- 5. LIVER INJURY • This term should be used if there is an increase in over 2 N in ALT [alanine aminotransferase] or CB [Conjugated Bilirubin] OR • Combined increase in AST [aspartate aminotransferase], AP [Alk Phos] & TB [Total Bil] provided one of them is above 2N. CIOMS
- 6. LIVER INJURY • Hepatocellular: Increase of over 2N in ALT alone or R ≥ 5 [R = serum activity of ALT/serum activity of AP – each expressed as multiple of N] • Cholestatic: Increase in over 2N in AP alone or R ≤ 2. • Mixed: Both ALT above 2N & AP are increased, & 2 < R < 5 CIOMS
- 7. ABNORMALITIES OF LIVER TESTS • Isolated increase even over 2N in AST, AP or TB should be considered only a biochemical abnormality and not necessarily a sign of liver injury • When the increase in ALT, AST, AP or TB is between N & 2N, the term – ‘abnormality of liver tests’ should be used & not ‘liver injury’. CIOMS
- 8. CLINICAL FEATURESCLINICAL FEATURES Drugs can cause nearly any type of liver disorder and can mimic many well-recognized clinical syndromes
- 9. CLINICAL FEATURES • Abnormal liver tests • Acute viral hepatitis-like injury • Acute [fulminant] liver failure • Cholestatic hepatitis • Liver disease with signs of hypersensitivity • Autoimmune hepatitis-like injury • Acute venous outflow obstruction • Obstructive jaundice-like • Chronic cholestasis • Cirrhosis • Primary hepatic neoplasms
- 10. DRUG INDUCED LIVER DISEASE [CLINICO-PATHOLOGICAL TYPES] HEPATOCELLULAR CHOLESTATIC VASCULAR MIXED STEATOSIS TUMOR GRANULOMATOUS
- 11. MECHANISMS OF HEPATOTOXICITY • Intrinsic hepatotoxins • Idiosyncratic hepatotoxins Hypersensitivity Metabolic Idiosyncrasy • Damage to the genome?
- 13. The hepatocyte in the center of the field is under- going apoptosis, while the other liver cells are swollen or ballooned. The inflammatory response is predomi- nantly lymphocytic. Acute hepatitis-like injury in a patient taking INH
- 14. Submassive (zone 3) hepatic necrosis, Lytic type, following halothane anesthesia
- 15. Submassive (zone 3) coagulative necrosis caused by an overdose of acetaminophen
- 16. The biopsy on the left has relatively ‘bland” Cholestasis. Biopsy on the right shows a com -bined hepatocellular and cholestatic injury
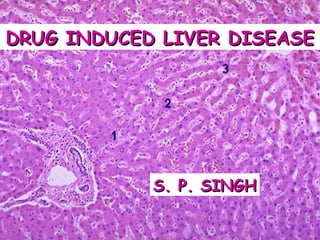
- 17. HEPATOCELLULAR & CANALICULAR CHOLESTASIS Bile is present within transversely (open arrow) or long- itudinally sectioned bile canaliculi (long arrows). Several hepatocytes at upper right (curved arrows) contain bile
- 18. Granulomatous hepatitis in a patient taking phenylbutazone
- 19. Severe chronic hepatitis in a patient who had taken α-methyldopa for 3 months
- 20. Severe liver injury in an atypical pattern, suggesting a drug-induced cause
- 21. Amiodarone phospholipidosis: foam cells and Mallory bodies
- 22. LIVER BIOPSY FINDINGS THAT SUGGEST DRUG HEPATOTOXICITY • Prominent Eosinophils in inflammatory infiltrate • Granulomatous Hepatitis with granulomas + hepatitis-like hepatocellular injury • Cholestatic Hepatitis: combined hepatocellular & cholestatic injury • Severe acute injury • Any unusual combination of histologic findings, atypical for any of the common primary liver diseases.
- 24. NAILING THE CULPRIT • Drug induced Liver disease can simulate nearly any clinical syndrome or pathologic lesion. • Diagnosis can not be made on morphologic grounds alone or on the basis of specific laboratory test ! • Careful correlation of history with clinical, laboratory & histologic data.
- 25. In every instance, the morphologic findings must be correlated with the following • A complete drug or chemical history: All exposures must be considered. • Specific and detailed time-related drug information: It is essential to know exactly when the drug was taken in relation to the signs, symptoms, and laboratory evidence of liver disease. • The results of the laboratory tests: These are essential in determining the onset, duration, and degree of injury.
- 26. The following should be determined from the history and lab studies: • Temporal eligibility • Exclusion of other causes • Precedent • Pattern of injury • Dechallenge and rechallenge • Toxicologic analysis
- 27. TEMPORAL ELIGIBILITY • Did the administration of the drug precede the onset of the liver disease by a reasonable time interval (latent period) for that drug? • An obvious but often overlooked point is that if the patient was already ill when he or she began taking the suspected drug, then the drug could not have caused the illness • It is also important to recognize that each drug that can cause liver injury does so after a latent period that is characteristic for that drug. In most cases, this is approximately 3 weeks to 3 months • If a drug has been taken regularly with no problems for years, it is extremely unlikely that it is responsible for a newly recognized injury
- 28. “Other causes besides the suspected drug need to be carefully considered and excluded if possible” EXCLUSION
- 29. PRECEDENT • Any drug that has been in use for some time will have a record that can be used to assess the likelihood of its having caused the suspected injury • However, any newly marketed drugs that the patient has taken should be considered too although they will not have a track record • When a list of drugs and dates has been assembled, each drug should be checked for potential hepatotoxicity • Resources: Physicians' Desk Reference & Medline-PubMed database [ http://www.nchi.nlm.nih.gov/entre2/query.fcgi ]
- 30. PATTERN OF INJURY • Pattern of injury produced by each drug tends to be consistent, or at least falls within a defined range. • For example, some drugs, such as erythromycin, typically produce cholestatic injury, wherease others, such as isoniazid, are nearly always hepatocellular. • The literature search is often helpful in establishing whether the type of injury seen in an individual case is typical or unusual for the suspected drug and will contribute to the assessment of the likelihood of a drug-induced cause
- 31. DECHALLENGE & RECHALLENGE • Dechallenge and rechallenge are very helpful in the final analysis • If the patient recovers after the drug is stopped, the likelihood that the drug was the cause is increased • However, lack of recovery does not always exclude the drug. In particular, recovery from a cholestatic injury can be very prolonged
- 32. RECHALLENGE • Deliberate rechallenge is never recommended, because it puts the patient at risk for a more serious injury • However if a drug is inadvertently readministered (eg, before it was suspected), the prompt return of the injury is extremely strong evidence that the drug is the causative agent
- 33. TOXICOLOGY • Toxicologic analysis of blood, tissue, or other body fluids can establish direct toxicity (overdose or poisoning) in selected cases only. • In most cases, however, drug hepatotoxicity is caused by idiosyncratic reactions, and so toxicology is of no use.
- 34. INTERNATIONAL CONSENSUS CRITERIA for Diagnosis of drug induced hepatotoxicity • The time from drug intake and withdrawal to the apparent onset of the reaction was "suggestive" (5-90 days from initial drug intake) or "compatible" (less than five or more than 90 days from initial drug intake and not more than 15 days of drug withdrawal for "hepatocellular" reaction and not more than 30 days of drug withdrawal for cholestatic reaction) with drug hepatotoxicity. • Course of the reaction after cessation of the drug was "very suggestive" (decrease in the liver enzymes by at least 50% of the excess over the upper limit of normal within eight days) or "suggestive" (decrease in the liver enzymes by at least 50% within 30 days for "hepatocellular" reaction and 180 days for "cholestatic" reaction) of drug reaction. • Alternative cause of the reaction had been excluded by detailed investigations, including a liver biopsy in each case. • There was a positive response to rechallenge (at least a doubling of liver enzymes) when such information was available. J Hepatol 1990;11:272-276
- 35. FINALLY AFTER A CASE HAS BEEN EVALUATED, IT CAN BE CLASSIFIED ON THE BASIS OF ‘CERTAINTY’ • Causative: Cases in which toxicologic analysis establishes a drug level in the toxic range. • Probable: Cases in which the drug is temporally eligible and in which the type of tissue injury is the same as that observed in previous experience with the drug. • Possible: Cases in which the type of injury can be associated with the drug but in which other factors or possible causes cannot be excluded. • Coincidental: Cases in which drug-induced disease appears to be most unlikely but cannot be absolutely denied. • Negative: Cases in which the possibility of a drug injury can be clearly eliminated.
- 36. HEPATOTOXICITY SCALES • Council for International Organizations of Medical Sciences (CIOMS) scale • Maria & Victorino (M&V) Clinical scale or CDS [Clinical Diagnostic Scale]
- 37. CLINICAL DIAGNOSTIC SCALE COMPONENT ELEMENTS I. Temporal relationship between drug intake and the reaction II. Exclusion of alternative causes III.Extrahepatic manifestations IV. Intentional or accidental re-exposure to the drug V. Previous report in the literature of cases of hepatotoxicity associated with the drug Maria & Victorino (M&V)
- 38. Scores for Individual Axes of the M&V Diagnostic Scale • From drug intake until onset event +1 to+3 • From drug withdrawal until onset event -3 to +3 • Course of the reaction 0 to +3 • Exclusion alternative causes -3 to +3 • Extrahepatic manifestations 0 to +3 • Bibliographic data -3 to +2 • Rechallenge 0 to +3 Axis Score
- 39. TEMPORAL RELATIONSHIP BETWEEN DRUG INTAKE & REACTION • Time: Intake – Onset of 1st clinical or Lab manifestation 4 Days – 8 Weeks 3 < 4 Days or > 8 Weeks 1 • Time: Drug withdrawal – Onset of manifestations 0 – 7 Days 3 8 – 15 Days 0 > 15 Days -3 • Time: Drug withdrawal – Normalization of Lab values [Decrease to values 2 x ULN] < 6 mo [Chole/mixed] or 2 mo [Hep] 3 > 6 mo [Chole/mixed] or 2 mo [Hep] 0 Clinical Diagnostic Scale
- 40. EXCLUSION OF ALTERNATIVE CAUSES • Complete Exclusion: 3 • Partial Exclusion: 0 • Possible alternate cause detected -1 • Probable alternative cause detected -1
- 41. EXTRAHEPATIC MANIFESTATIONS [rash, fever, arthralgia, eosinophilia, cytopenia] • 4 or more 3 • 2 or 3 2 • 1 1 • None 0
- 42. CLINICAL DIAGNOSTIC SCALE: CONTINUED • INCIDENTAL / ACCIDENTAL RE-EXPOSURE Positive re-challenge test 3 Negative or absent re-challenge test 0 • PREVIOUS REPORT IN LITERATURE OF DILI Yes 2 No [drugs marketed for up to 5 years] 0 No [drugs marketed for > 5 years] -3
- 43. CDS: VALIDITY • CDS score of > 9 identified the cases of drug-related hepatotoxicity with 88% sensitivity and 92% specificity. • Patients with scoring ≤ 9 on CDS scale require further investigation & / or follow-up. • CDS scoring useful in evaluation of suspected hepatotoxic drug reactions Aithal et al, J Hepatol 2000
- 44. Scores for Individual Axes of the CIOMS Scale • From drug intake until onset event +2 to+1 • From drug withdrawal until onset event +1 to 0 • Course of the reaction +1 to 0 Risk factors • Age +1 to 0 • Alcohol +1 to 0 • Concomitant therapy -3 to 0 • Exclusion non-drug-related causes -3 to +2 • Bibliographic data 0 to +2 • Rechallenge -2 to +3 Axis Score
- 45. Summary of “Diagnosis” • Drug-induced liver disease is a relatively common, but often unrecognized, cause of liver injury • Drugs are great imitators, capable of producing nearly any clinical scenario and histopathologic lesion • When dealing with a liver biopsy from a patient with an undiagnosed liver disease, the diagnosis of drug hepatotoxicity is made by first having a high index of suspicion, and then by careful correlation
- 46. MANAGEMENT ?
- 47. PREVENTION OF DILD • With the exception of acetaminophen hepatotoxicity , there is little effective treatment for drug-induced liver disease. • All physicians must report suspected adverse effects to monitoring agencies or publish them. • Minimize DILI through avoidance of overuse of hepatotoxic drugs; avoid polypharmacy. • For dose-dependent hepatotoxins, prevention depends on adherence to dosage guidelines or use of blood levels.
- 48. ACTIVE MANAGEMENT • Active management might include removal of the drug and the administration of antidotes and anti-inflammatory and cytoprotective agents. In practice, management is usually confined to discontinuation of hepatotoxic drugs. • For ingested toxins like metals, poisonous mushrooms, and acetaminophen,removal of unabsorbed drug through the aspiration of stomach contents may be appropriate. • Thiol replacement therapy, usually N- acetylcysteine (NAC), is indicated as an antidote for acetaminophen poisoning .
- 49. ACTIVE MANAGEMENT • Beyond discontinuation of the offending agent, the management of drug hepatitis and cholestasis is symptomatic and supportive. • In cases of acute liver failure, hepatic transplantation should be considered.
- 50. ACTIVE MANAGEMENT • Ursodeoxycholic acid has some promise for chronic cholestasis and pruritus. • Glucocorticoids have little role in the management of drug-induced cholestasis or hepatitis and are ineffective in chlorpromazine-, methyldopa-, and isoniazid-induced hepatitis and in drug- induced fulminant hepatic failure. • Case reports attest to their occasional effectiveness in protracted cases of hepatitis caused by etretinate, allopurinol, diclofenac, or ketoconazole. • Glucocorticoids should be reserved for atypical and refractory cases, particularly those with vasculitis.
- 51. THANK YOU
- 52. COLOMBO BECKONS For all queries, write to: saasl.secy@gmail.com
- 55. Measures proposed to reduce risk of severe hepatic adverse effects during ATT • First, patients with underlying liver test abnormalities should not be given pyrazinamide. • Second, isoniazid & pyrazinamide should be administered at the lowest dosage within their respective therapeutic ranges. • Third, Se transaminase levels should be determined twice weekly during first 2 wks of treatment, every 2 wks during the rest of the first 2 mos, and every mo thereafter. Durand et al, 1996
- 56. Measures proposed to reduce risk of severe hepatotoxicity during ATT • When Se transaminase ↑to > 3 times ULN, therapy with isoniazid, rifampicin and pyrazinamide should be stopped. • After Se transaminase levels have returned to normal, INH can be re-introduced at a low daily dose, without rifampicin. • Pyrazinamide may not be re-introduced: risk of recurrence & poor prognosis of pyrazinamide-induced hepatitis. • Although nephrotoxic, streptomycin is an alternative in patients with LFT abnormalities during ATT. Durand et al, 1996
- 58. Challenge Reintroduction Dosages • Isoniazid: Introduce at 50 mg/day; increase sequentially to 300 mg/day after 2–3 days if no reaction occurs, and then continue. • Rifampicin: Added after a further 2–3 days without reaction: 75 mg/day increase to 300 mg after 2–3 days, & then to 450 mg (<50 kg) or 600 mg (>50 kg) as appropriate after further 2–3 days without reaction, and then continued. • Pyrazinamide: Added finally: 250 mg/day, increase to 1.0 g after 2–3 days; then to 1.5 g (<50 kg) or 2 g (>50 kg).
- 60. Clinical Infectious Diseases 2010; 50:833–839.
- 61. Three Different Regimens for Reintroduction of Anti-Tuberculosis Drugs SK Sharma et al. Clinical Infectious Diseases 2010
- 62. SK Sharma et al. Clinical Infectious Diseases 2010 Summary of the ATT Re-introduction Study
- 65. Acetaminophen induced DILI • N-acetylcysteine reduces mortality even if commenced late • Reduces Inotrope Requirements • Decreases Cerebral Edema • Increases the rate of survival by about 30%30%* * Keays et al. IV NAC in paracetamol induced FHF: A prospective controlled trial.
- 66. Valproate induced DILI • IV Carnitine* • Overcomes inhibition of β-oxidation of Fatty Acids caused by Valproate • Also es↑ β-oxidation of Valproate • IV is better than Oral supplementation* • ↑ Survival* * Bohan et al. Effect of L-carnitine treatment for valproate-induced hepatotoxicity.
- 67. • Silymarin alone or combination of Silymarin + Benzylpenicillin for Mushroom (Amanita phalloides) toxaicity1 • Corticosteroids: can be attempted in cholestatic hepatitis with f/o hypersensitivity (rash & fever)2 1. Enjalbert et al. Treatment of amatoxin poisoning: 20-yr retrospective analysis. J Toxicol Clin Toxicol 2002
Notas del editor
- Acute hepatitis-like injury in a patient taking isoniazid. The hepatocyte in the center of the field is undergoing apoptosis, while the other liver cells are swollen or ballooned. The inflammatory response is predominantly lymphocytic.
- Submassive (zone 3) hepatic necrosis, lytic type, following halothane anesthesia. There is loss of hepatocytes and stromal collapse surrounding terminal hepatic venules (“central veins”) with central-central and sometimes central-portal bridging.
- Submassive (zone 3) coagulative necrosis caused by an overdose of acetaminophen. Viable hepatocytes surround the portal areas, while the terminal hepatic venules (arrows) are surrounded by necrotic tissue. Inset (lower right) shows the necrotic hepatocytes at high magnification.
- Cholestatic injury. The biopsy on the left has relatively ‘bland” cholestasis with numerous canalicular bile plugs (arrows) but relatively little hepatocellular injury. The biopsy on the right shows a combined hepatocellular and cholestatic injury with canalicular bile plugs (arrows), as well as hepatocyte ballooning and dropout, producing disarray of the liver cell plates.
- Hepatocellular and canalicular cholestasis. Bile is present within transversely (open arrow) or longitudinally sectioned bile canaliculi (long arrows). Several hepatocytes at upper right (curved arrows) contain bile (hematoxylin and eosin, original magnification × 400).
- Granulomatous hepatitis in a patient taking phenylbutazone. There are two young granulomas (arrows) composed of epithelioid histiocytes, lymphocytes, and a few eosinophils, and the surrounding parenchyma also has spotty hepatocyte dropout and lymphocytic inflammation.
- Severe chronic hepatitis in a patient who had taken α-methyldopa for 3 months. The biopsy resembles autoimmune hepatitis with diffuse hepatocellular ballooning, portal expansion, and fibrosis. There are numerous plasma cells in the portal inflammatory infiltrate, and there is marked interface hepatitis around the circumference of the expanded portal tract.
- Severe liver injury in an atypical pattern, suggesting a drug-induced cause. The liver biopsy shows confluent zone 3 necrosis and collapse (left) but the surrounding inflammation consists of epithelioid histiocytes and giant cells (upper right) and numerous plasma cells. Because the combination of histologic features was so unusual and unlike any naturally occurring liver disease, a drug reaction was suspected. Further inquiry into the history revealed that the patient had been taking trovafloxacin before becoming ill.
- Amiodarone phospholipidosis. A, Black and white photomicrograph (H and E x 160) showing foam cells in right upper corner and Mallory bodies (arrows).B, A closer view of area with foam cells in the same patient. C, Electron microphotograph (x22,600) of the same case showing multiple dense, laminated inclusions (myelin figures) in the hepatocyte cytoplasm. Another cardiac medication that may cause toxicity to the liver and other organs is amiodarone, an antiarrhythmia agent. Dose-related hepatotoxicity, with an incidence of 15% to 50% [1] may become manifest 1 month to more than 1 year of therapy. The clinical picture varies from asymptomatic transaminase elevation to fulminant hepatic failure [25]. Severe cholestasis may be present and fatal cirrhosis can ensue. The hepatic accumulation of amiodarone can be detected by CT because the drug is iodinated; however, the increased density does not correlate with the degree of liver damage [26]. Unlike alcoholic hepatitis, in which the damage tends to be centrilobular, amiodarone hepatotoxicity is mainly periportal [27]. The possible mechanism of the steatosis is discussed in Figure 6-33. (Courtesy of K. Ishak.)