Causes, Diagnosis and Treatment of Rickets
- 2. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA
- 3. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA Nutritional Vit D deficiency Congenital Vit D deficiency Secondary Vit D deficiency -Malabsorption -Increased degradation -Decreased liver 25-hydroxylase Vit D–dependent rickets type 1 Vit D–dependent rickets type 2 Chronic renal failure
- 4. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA Low intake -Diet -Premature infants (rickets of prematurity) Malabsorption -Primary disease -Dietary inhibitors of calcium absorption
- 5. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA Inadequate intake -Premature infants (rickets of prematurity) -Aluminum-containing antacids
- 6. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA XL Hypophosphatemic rickets AD Hypophosphatemic rickets Hereditary hypophosphatemic rickets with hypercalciuria Overproduction of phosphatonin -Tumor-induced rickets -McCune-Albright syndrome -Epidermal nevus syndrome -Neurofibromatosis Fanconi syndrome Dent disease
- 7. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA
- 8. • DIAGNOSIS OF RICKETS: • HISTORY • PHYSICAL FINDINGS • RADIOGRAPHICAL CHANGES • LAB TESTS
- 9. • Clinical Evaluation. • HISTORY REGARDING: • 1.Diet intake of Vit D, Calcium • 2.Sun exposure • 3.Maternal risk factors for vit D deficiency. • 4.Child's medication history. • 5.History of liver or intestinal disease – malabsorption of vit D • 6.History of Renal disease • 7.Family history of bone disease, short stature, unexplained sibling death. • 8.History of dental caries, poor growth, delayed walking, waddling gait, pneumonia, and hypocalcemic symptoms.
- 10. • CLINICAL FEATURES: • GENERAL • Failure to thrive • Listlessness • Protuding abdomen • Muscle weakness (especially proximal) • Fractures
- 11. • CLINICAL FEATURES: • HEAD • Craniotabes • Frontal bossing • Delayed fontanelle closure • Delayed dentition; caries • Craniosynostosis
- 12. • CLINICAL FEATURES: • CHEST • Rachitic rosary • Harrison groove • Respiratory infections and atelectasis • BACK • Scoliosis • Kyphosis • Lordosis
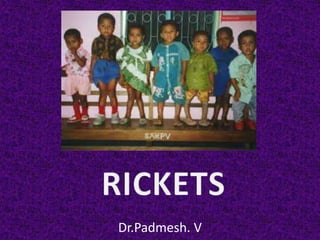
- 13. • CLINICAL FEATURES: • EXTREMITIES • Enlargement of wrists and ankles • Valgus or varus deformities • Anterior bowing of the tibia and femur • Coxa vara • Leg pain
- 14. • CLINICAL FEATURES: • EXTREMITIES • Enlargement of wrists and ankles • Valgus or varus deformities • Anterior bowing of the tibia and femur • Coxa vara • Leg pain
- 15. • CLINICAL FEATURES: • EXTREMITIES • Enlargement of wrists and ankles • Valgus or varus deformities • Anterior bowing of the tibia and femur • Coxa vara • Leg pain
- 16. • CLINICAL FEATURES: • EXTREMITIES • Enlargement of wrists and ankles • Valgus or varus deformities • Anterior bowing of the tibia and femur • Coxa vara • Leg pain
- 17. • CLINICAL FEATURES: • EXTREMITIES • Valgus or varus deformities • Windswept deformity (combination of valgus deformity of 1 leg with varus deformity of the other leg) • Anterior bowing of the tibia and femur • Coxa vara
- 18. • CLINICAL FEATURES: • HYPOCALCEMIC SYMPTOMS: • Tetany • Seizures • Stridor due to laryngeal spasm
- 19. • CLINICAL FEATURES: • Craniotabes: • Softening of cranial bones. • Detected by applying pressure at the occiput or parietal bones.
- 20. • CLINICAL FEATURES: • Craniotabes: • Craniotabes may also be secondary to -osteogenesis imperfecta, -hydrocephalus, -syphilis. • May be a normal finding in many newborns, especially near the suture lines, but disappears within a few months of birth.
- 21. • CLINICAL FEATURES: • Rachitic Rosary: • Widening of costochondral junctions Rachitic rosary. • Feels like beads of a rosary as the examiner's fingers move along the costochondral junctions from rib to rib. • Growth plate widening: • This is also responsible for the enlargement at wrists and ankles.
- 23. • CLINICAL FEATURES: • Harrison groove: • Horizontal depression along lower anterior chest. • Due to pulling of softened ribs by diaphragm during inspiration. • Softening of ribs impairs air movement & predisposes to atelectasis. • Risk of pneumonia high in children with rickets
- 24. • RADIOLOGY: • Decreased calcification Thickening of growth plate. • FRAYING: Edge of metaphysis loses its sharp border. • CUPPING: Edge of metaphysis changes from convex or flat to concave surface. Most easily seen at distal ends of radius, ulna, fibula. • Widening of distal end of metaphysis Clinically causes thickened wrists and ankles, and rachitic rosary.
- 25. • RADIOLOGY: • Especially on PA view of wrist. Also in other growth plates. • Other radiologic features: -Coarse trabeculation of diaphysis -Generalized rarefaction.
- 28. • LAB TESTS: • Initial laboratory tests in Rickets should include: • Serum calcium; • Phosphorus; • Alkaline phosphatase; • Parathyroid hormone (PTH); • 25-hydroxyvitamin D; • 1,25-dihydroxyvitamin D3; • Creatinine; and • Electrolytes.
- 29. • Urinalysis: Useful for detecting glycosuria and aminoaciduria (positive dipstick for protein) in Fanconi syndrome. • Evaluation of urinary excretion of calcium (24 hr collection for calcium or calcium-creatinine ratio) : If hereditary hypophosphatemic rickets with hypercalciuria or Fanconi syndrome is suspected. • Direct measurement of other fat-soluble vitamins (A, E, and K) or indirect assessment of deficiency (prothrombin time for vitamin K deficiency) : if malabsorption is a consideration.
- 30. • Laboratory Findings in Disorders Causing Rickets:
- 31. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA
- 32. • VITAMIN D: 7-DEHYDROCHOLESTEROL UV radiation in sunlight Inhibited by melanin VITAMIN D3 Bound to Vit D binding protein Transported to liver 25-Hydroxylase 25-D 1 α Hydroxylase Kidney 1,25 D Binds to intracellular receptor and forms a COMPLEX CALCIUM PHOSPHORUS BONE PTH secrn Inhibits its own absorption absorption resorption synthesis in kidney
- 33. • NOTE: • PTH Increased Calcium, Decreased Phosphate • 1,25 D Increased Calcium, Increased Phosphate • Calcitonin Decreased Calcium
- 34. • NUTRITIONAL VIT D DEFICIENCY: • Most common cause of rickets globally. • Etiology: • Most common in infancy: Due to poor intake + inadequate cutaneous synthesis. • Transplacental transport of vitamin D, mostly 25-D,provides vitamin D for 1st 2 mo of life unless there is severe maternal vitamin D deficiency. • Breast-fed infants, because of low vitamin D content of breast milk, rely on cutaneous synthesis or vitamin supplements. • Infants who receive formula receive adequate vitamin D, even without cutaneous synthesis.
- 35. • NUTRITIONAL VIT D DEFICIENCY: • Most common cause of rickets globally. • Etiology: • Cutaneous synthesis is limited by ineffective winter sun; and by increased skin pigmentation. • Mothers may have same risk factors decreased maternal vitamin D reduced vitamin D in breast milk + less transplacental delivery of vitamin D. • Unconventional dietary practices, such as vegan diets that use unfortified soy milk or rice milk.
- 36. • NUTRITIONAL VIT D DEFICIENCY: • Laboratory Findings. • Elevated PTH Hypophosphatemia • Variable hypocalcemia • Hypophosphatemia & hyperparathyroidism Upregulation of renal 1α-hydroxylase Wide variation in 1,25-D levels (low, normal, or high) • 1,25-D is only low when there is severe vitamin D deficiency. • Some have metabolic acidosis secondary to PTH-induced renal bicarbonate-wasting. • There may be generalized aminoaciduria.
- 37. • VITAMIN D: 7-DEHYDROCHOLESTEROL UV radiation in sunlight Inhibited by melanin VITAMIN D3 Bound to Vit D binding protein Transported to liver 25-Hydroxylase 25-D 1 α Hydroxylase Kidney 1,25 D Binds to intracellular receptor and forms a COMPLEX CALCIUM PHOSPHORUS BONE PTH secrn Inhibits its own absorption absorption resorption synthesis in kidney
- 38. • NUTRITIONAL VIT D DEFICIENCY: • DIAGNOSIS: • History of poor vitamin D intake & risk factors for decreased cutaneous synthesis. • Radiographic changes consistent with rickets, and • Laboratory findings. • Normal PTH level almost never occurs with vitamin D deficiency and suggests a primary phosphate disorder. • Calcium deficiency may occur with or without vitamin D deficiency. • A normal level of 25-D and a dietary history of poor calcium intake support a diagnosis of isolated calcium deficiency.
- 39. • NUTRITIONAL VIT D DEFICIENCY: • Treatment: • Vitamin D + Calcium + Phosphorus. • 2 strategies for vitamin D admn: • Stoss therapy: 300,000–600,000 IU of vitamin D oral or IM as 2–4 doses over 1 day. • Because doses are observed, stoss therapy is ideal where adherence to therapy is questionable. • Alternative: Daily, high-dose vitamin D, with doses ranging from 2,000–5,000 IU/day over 4–6 wk. • Either strategy should be followed by daily vitamin D intake of 400 IU/day, typically given as a multivitamin. • Ensure adequate dietary calcium & phosphorus; (milk, formula, and other dairy products)
- 40. • NUTRITIONAL VIT D DEFICIENCY: • Treatment: • Symptomatic hypocalcemia: IV Calcium acutely, followed by oral calcium supplements, tapered over 2–6 wk in children who receive adequate dietary calcium. • Transient use of intravenous or oral 1,25-D (calcitriol) to reverse hypocalcemia in acute phase. (by providing active vitamin D during the delay as supplemental vitamin D is converted to active vitamin D. )
- 41. • NUTRITIONAL VIT D DEFICIENCY: • Prognosis. • Most: Excellent response to treatment. • Radiologic healing within a few months. • Laboratory tests normalize rapidly. • Many of the bone malformations improve dramatically, but children with severe disease may have permanent deformities. • Short stature does not resolve in some children. • Prevention. • Universal administration of daily multivitamin containing 200–400 IU of vitamin D to children who are breast-fed. • For other children, diet should have sources of vitamin D.
- 42. • CONGENITAL VIT D DEFICIENCY: • Occurs if severe maternal vitamin D deficiency during pregnancy. • Maternal risk factors: -Poor dietary intake of vitamin D, -Lack of adequate sun exposure, and -Closely spaced pregnancies.
- 43. • CONGENITAL VIT D DEFICIENCY: • Newborns may have: -symptomatic hypocalcemia, -intrauterine growth retardation, -decreased bone ossification, and -classic rachitic changes. • Subtler maternal vitamin D deficiency: -adverse effect on neonatal bone density -adverse effect on birthweight, -defect in dental enamel, and -predispose to neonatal hypocalcemic tetany.
- 44. • CONGENITAL VIT D DEFICIENCY: • Treatment of congenital rickets: -Vitamin D supplementation -Adequate intake of Calcium and Phosphorus. • Prevention: -Use of prenatal vitamins containing vitamin D.
- 45. • SECONDARY VIT D DEFICIENCY: • Etiology. -inadequate intake, -inadequate absorption, -decreased hydroxylation in liver, and -increased degradation.
- 46. • SECONDARY VIT D DEFICIENCY: • Etiology. -inadequate intake, -inadequate absorption, -decreased hydroxylation in liver & -increased degradation. Liver & gastrointestinal diseases: -Cholestatic liver disease, -Defects in bile acid metabolism -Cystic fibrosis -Other causes of pancreatic dysfunction, -Celiac disease, -Crohn disease. -Intestinal lymphangiectasia -After intestinal resection.
- 47. • SECONDARY VIT D DEFICIENCY: • Etiology. -inadequate intake, -inadequate absorption, -decreased hydroxylation in liver -increased degradation. Severe Liver disease: -Insufficient enzyme axn (25 hydroxylase)
- 48. • SECONDARY VIT D DEFICIENCY: • Etiology. -inadequate intake, -inadequate absorption, -decreased hydroxylation in liver & -increased degradation. -Drugs by inducing P450 -Anticonvulsants: Phenobarb, Phenytoin. -ATT : Isoniazid, Rifampin
- 49. • SECONDARY VIT D DEFICIENCY: • Treatment. • 1. Malabsorption: • Requires high doses of vitamin D. • 25-D (25–50 μmg/day or 5–7 μmg/kg/day)-Better absorption - superior to vitamin D3. • Alternatively: • 1,25-D (also better absorbed in presence of fat malabsorption) or • Parenteral vitamin D. • 2. In rickets due to increased degradation of Vit D by P450 system: Require same acute therapy as for nutritional deficiency, followed by Long-term administration of high doses of Vit D (e.g., 1,000 IU/day), (With dosing titrated based on serum levels of 25-D) Some patients require as much as 4,000 IU/day.
- 50. • VITAMIN D–DEPENDENT RICKETS, TYPE 1. • Autosomal Recessive. • Mutations in gene encoding renal 1α-hydroxylase. • Prevent conversion of 25-D into 1,25-D. • Normally present during 1st 2 yr of life. • Can have any features of rickets, including symptomatic hypocalcemia.
- 51. • VITAMIN D–DEPENDENT RICKETS, TYPE 1. • Normal levels of 25-D, but low levels of 1,25-D. • Occasionally, 1,25-D levels may be low normal. • High PTH. • Low serum phosphorus levels. • Metabolic acidosis & generalized aminoaciduria. (Due to renal tubular dysfunction)
- 52. • VITAMIN D: 7-DEHYDROCHOLESTEROL UV radiation in sunlight Inhibited by melanin VITAMIN D3 Bound to Vit D binding protein Transported to liver 25-Hydroxylase 25-D 1 α Hydroxylase Kidney 1,25 D Binds to intracellular receptor and forms a COMPLEX CALCIUM PHOSPHORUS BONE PTH secrn absorption absorption resorption
- 53. • VITAMIN D–DEPENDENT RICKETS, TYPE 1. • Normal levels of 25-D, but low levels of 1,25-D. • Occasionally, 1,25-D levels may be at the lower limit of normal, but this is inappropriate, given the high PTH and low serum phosphorus levels, both of which should increase the activity of renal 1α- hydroxylase and cause elevated levels of 1,25-D. • As in nutritional vitamin D deficiency, renal tubular dysfunction may cause a metabolic acidosis and generalized aminoaciduria.
- 54. • VITAMIN D–DEPENDENT RICKETS, TYPE 1. • TREATMENT: • Long-term treatment with 1,25-D (calcitriol). • Initial: 0.25–2 μmg/day, with lower doses used once the rickets has healed. • During initial therapy, ensure adequate intake of calcium. • Periodic monitoring of urinary calcium excretion, with target of <4 mg/kg/day.
- 55. • VITAMIN D–DEPENDENT RICKETS, TYPE 2. • Autosomal Recessive. • Mutations in gene encoding the vitamin D receptor. • Prevents a normal physiologic response to 1,25-D. • Levels of 1,25-D are extremely elevated. • Less severe disease is associated with a partially functional vitamin D receptor.
- 56. • VITAMIN D–DEPENDENT RICKETS, TYPE 2. • Most patients present during infancy. • Less severely affected patients may not be diagnosed until adulthood. • 50–70% of children have alopecia.
- 57. • VITAMIN D–DEPENDENT RICKETS, TYPE 2. • Treatment. • Some patients, especially those without alopecia, respond to extremely high doses of vitamin D2, 25-D, or 1,25-D. • Due to partially functional vitamin D receptor. • 3–6 month trial of high-dose vitamin D and oral calcium.
- 58. • VITAMIN D–DEPENDENT RICKETS, TYPE 2. • Treatment. • The initial dose of 1,25-D should be 2 μmg/day, but some patients require doses as high as 50–60 μmg/day. • Calcium doses range from 1,000–3,000 mg/day.
- 59. • CHRONIC RENAL FAILURE: • Decreased activity of 1α-hydroxylase in kidney diminished production of 1,25-D. • In chronic renal failure, unlike the other causes of vitamin D deficiency, patients have hyperphosphatemia as a result of decreased renal excretion. • Along with inadequate calcium absorption and secondary hyperparathyroidism, the rickets may be worsened by the metabolic acidosis of chronic renal failure.
- 60. • VITAMIN D: 7-DEHYDROCHOLESTEROL UV radiation in sunlight Inhibited by melanin VITAMIN D3 Bound to Vit D binding protein Transported to liver 25-Hydroxylase 25-D 1 α Hydroxylase Kidney 1,25 D Binds to intracellular receptor and forms a COMPLEX CALCIUM PHOSPHORUS BONE PTH secrn absorption absorption resorption
- 61. • CHRONIC RENAL FAILURE: • Treatment. • A form of vitamin D which can act without 1-hydroxylation by kidney should be used for therapy (Calcitriol). • Calcitriol permits both adequate absorption of calcium and directly suppresses the parathyroid gland. • Dietary phosphorus restriction & Oral phosphate binders. (Because hyperphosphatemia is a stimulus for PTH secretion) • Chronic metabolic acidosis should be corrected with alkali.
- 62. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA
- 63. • CALCIUM DEFICIENCY: • CAUSES: • After weaning / early weaning. • Low calcium content in diet. (<200 mg/day) • Grains & green leafy vegetables high in phytate, oxalate, and phosphate decrease absorption of dietary calcium. • In children getting IV nutrition without adequate calcium. • Malabsorption of calcium: -in celiac disease, -intestinal abetalipoproteinemia, and -after small bowel resection.
- 64. • CALCIUM DEFICIENCY: • Clinical Manifestations. • Classic signs and symptoms of rickets. • Presentation: infancy or early childhood, although some are diagnosed in teenagers. • Because calcium deficiency occurs after cessation of breast-feeding, it tends to occur LATER than nutritional vitamin D deficiency that is associated with breast-feeding.
- 65. • CALCIUM DEFICIENCY: • Diagnosis. • Laboratory findings: • Increased levels of Alkaline phosphatase, PTH, and 1,25-D. • Calcium levels may be normal or low, although symptomatic hypocalcemia is uncommon. • Decreased urinary excretion of calcium. • Secondary hyperparathyroidism Low Serum phosphorus levels. • In some children, there is coexisting nutritional vitamin D deficiency Low 25-D.
- 66. • VITAMIN D: 7-DEHYDROCHOLESTEROL UV radiation in sunlight Inhibited by melanin VITAMIN D3 Bound to Vit D binding protein Transported to liver 25-Hydroxylase 25-D 1 α Hydroxylase Kidney 1,25 D Binds to intracellular receptor and forms a COMPLEX CALCIUM PHOSPHORUS BONE PTH secrn Inhibits its own absorption absorption resorption synthesis in kidney
- 67. • CALCIUM DEFICIENCY: • Treatment. • Calcium supplement (350–1,000 mg/day of elemental calcium). • Vitamin D supplementation if concurrent vitamin D deficiency. • Prevention: -Discourage early cessation of breast-feeding. -Increase dietary sources of calcium.
- 68. • CAUSES OF RICKETS: • 1. VITAMIN D DISORDERS • 2. CALCIUM DEFICIENCY • 3. PHOSPHORUS DEFICIENCY • 4. RENAL LOSSES • 5. DISTAL RTA
- 69. • INADEQUATE INTAKE. • Only in starvation or severe anorexia. • Malabsorption of phosphorus.(celiac disease, cystic fibrosis, cholestatic liver disease); But rickets is primarily due to malabsorption of vitamin D and/or calcium. • Isolated malabsorption of phosphorus: in long-term use of aluminum-containing antacids.
- 70. • PHOSPHATONIN. Phosphatonin (a humoral mediator) Decreases renal tubular reabsorption Decreases activity of renal of phosphate 1α-hydroxylase Increased excretion of Phosphorus Decrease in production of 1,25-D. Decreases S.phosphorus • Fibroblast growth factor-23 (FGF-23) is the most well characterized phosphatonin.
- 71. • X-LINKED HYPOPHOSPHATEMIC RICKETS. • X-linked hypophosphatemic rickets (XLH) is the most common genetic cause of Rickets. • Defective gene is on X chromosome. • Female carriers are affected, so it is X-linked dominant. • Pathophysiology. • Defective gene: ‘PHEX’ (PHosphate-regulating gene with homology to Endopeptidases on X chromosome)
- 72. PHEX GENE Product of this gene inactivates phosphatonin Increased Phosphatonin Decreased Phosphorus
- 73. • X-LINKED HYPOPHOSPHATEMIC RICKETS. PHEX GENE Product of this gene inactivates phosphatonin Increased Phosphatonin Decreased Phosphorus
- 74. • X-LINKED HYPOPHOSPHATEMIC RICKETS. • Clinical Manifestations. • Rickets. • Abnormalities of lower extremities and poor growth are the dominant features. • Short stature • Delayed dentition, tooth abscesses.
- 75. • X-LINKED HYPOPHOSPHATEMIC RICKETS. • Laboratory Findings. • High renal excretion of phosphate, • Hypophosphatemia, • Increased alkaline phosphatase, • PTH and serum calcium levels are normal. • Hypophosphatemia normally upregulates renal 1α- hydroxylase, and should lead to an increase in 1,25-D, but these patients have low or inappropriately normal levels.
- 76. • X-LINKED HYPOPHOSPHATEMIC RICKETS. • Treatment. • Patients respond well to combination of oral phosphorus and 1,25-D (calcitriol). • Daily : 1–3 g of elemental phosphorus divided into 4–5 doses. • Frequent dosing helps to prevent prolonged decrements in serum phosphorus because there is a rapid decline after each dose. • In addition, frequent dosing decreases diarrhea, a complication of high-dose oral phosphorus. • Calcitrol : 30–70 ng/kg/day divided into 2 doses.
- 77. • X-LINKED HYPOPHOSPHATEMIC RICKETS. • Complications of treatment occur when there is no balance between phosphorus supplementation and calcitriol. • Excess phosphorus decrease enteral calcium absorption secondary hyperparathyroidism worsening of bone lesions. • Excess calcitriol hypercalciuria and nephrocalcinosis; it may even cause hypercalcemia. • Hence, laboratory monitoring of treatment includes : Serum calcium, phosphorus, alkaline phosphatase, PTH, and urinary calcium; Periodic renal ultrasounds to evaluate nephrocalcinosis.
- 78. • X-LINKED HYPOPHOSPHATEMIC RICKETS. • Normalization of alkaline phosphatase levels is a more useful method of assessing therapeutic response than measuring serum phosphorus. • For children with significant short stature, growth hormone is an effective option. • Children with severe deformities may need osteotomies, but done only when treatment has led to resolution of the bone disease.
- 79. • AUTOSOMAL DOMINANT HYPOPHOSPHATEMIC RICKETS. • Less common than XLH. • Incomplete penetrance and variable age of onset. • Mutation in gene encoding FGF-23. • Mutation prevents degradation of FGF-23 by proteases, leading to increased levels of this phosphatonin. • In ADHR, as in XLH, abnormal laboratory findings are hypophosphatemia, an elevated alkaline phosphatase level, and a low or inappropriately normal 1,25-D level . • Treatment is similar as in XLH.
- 80. • Rickets Associated with Renal Tubular Acidosis : • Rickets may be present in RTA, particularly in type II or proximal RTA. • Hypophosphatemia and phosphaturia are common. (Also characterized by hyperchloremic metabolic acidosis, various degrees of bicarbonaturia, and frequently, hypercalciuria and hyperkaluria. ) • Proximal RTA is treated with both bicarbonate and oral phosphate supplements to heal rickets. • Vitamin D given to offset the secondary hyperparathyroidism that complicates oral phosphate therapy.
- 81. • Rickets Associated with Renal Tubular Acidosis • Bone demineralization without overt rickets: in type I or distal RTA. • Bone pain, growth retardation, osteopenia, and, occasionally, pathologic fractures. • Bone demineralization in distal RTA probably due to dissolution of bone because calcium carbonate in bone serves as a buffer against metabolic acidosis due to hydrogen ions retained in RTA. • Administration of sufficient bicarbonate to reverse acidosis stops bone dissolution and the hypercalciuria that is common in distal RTA. • Following therapy, growth in patients with type II (proximal) RTA is greater than in patients with primary Fanconi syndrome.
- 82. • RICKETS OF PREMATURITY : • Pathogenesis. • Transfer of calcium and phosphorus from mother to fetus occurs throughout pregnancy, but 80% occurs during the 3rd trimester. • Premature birth interrupts this process rickets develop. • Most cases of rickets of prematurity occur in birthweight <1,000 g. • More likely to develop in infants with lower birthweight and younger gestational age. • Rickets occurs because unsupplemented breast milk and standard infant formula do not contain enough calcium and phosphorus to supply the needs of the premature infant.
- 83. • RICKETS OF PREMATURITY • Clinical Manifestations. • Rickets of prematurity presents 1–4 mo after birth. • Infants may have nontraumatic fractures. • Fractures & softening of ribs decreased chest compliance respiratory distress due to atelectasis & poor ventilation. • Rachitic respiratory distress usually develops >5 weeks after birth, distinguishing it from the early-onset respiratory disease of premature infants.
- 84. • RICKETS OF PREMATURITY • Clinical Manifestations. • Poor linear growth. • Enamel hypoplasia. • Poor bone mineralization dolichocephaly. • Classic rachitic findings MAY be present. • Most infants with rickets of prematurity have no clinical manifestations, and diagnosis is based on radiographic & lab findings.
- 85. • RICKETS OF PREMATURITY • Laboratory Findings. • Due to inadequate intake: serum phosphorus level is low or low- normal. • Renal conservation of phosphate : Low urine phosphate level; • Most patients have normal levels of 25-D, unless there has been inadequate intake or poor absorption . • Hypophosphatemia stimulates renal 1α-hydroxylase 1,25-D is high or high-normal. These high levels may contribute to bone demineralization because 1,25-D stimulates bone resorption.
- 86. • RICKETS OF PREMATURITY • Laboratory Findings. • Serum calcium is low, normal, or high, and patients often have hypercalciuria. • Elevated serum calcium levels and hypercalciuria are secondary to: -increased intestinal absorption and bone dissolution due to elevation of 1,25-D levels and -the inability to deposit calcium in bone because of an inadequate phosphorus supply. • There is an inadequate supply of calcium and phosphorus, but the deficiency in phosphorus is greater.
- 87. • RICKETS OF PREMATURITY • Laboratory Findings. • Alkaline phosphatase often elevated, but some have normal levels. • No single blood test is 100% sensitive for the diagnosis of rickets. • The diagnosis should be suspected in infants with : -alkaline phosphatase level more than 5–6 times the upper limit of normal for adults (unless there is concomitant liver disease) or -phosphorus level <5.6 mg/dL.
- 88. • RICKETS OF PREMATURITY • Laboratory Findings. • Confirmed by radiologic evidence of rickets- best seen on films of1 wrists and ankles. • Rachitic rosary may be visible on chest x-ray. • Unfortunately, x-rays are not able to detect early demineralization of bone because changes are not evident until there is >20–30% reduction in bone mineral content.
- 89. • RICKETS OF PREMATURITY • Diagnosis. • Screening tests are recommended. • Weekly measurements of calcium, phosphorus, and alkaline phosphatase. • Periodic measurement of serum bicarbonate is important because metabolic acidosis causes dissolution of bone. • At least 1 screening x-ray for rickets at 6–8 wk of age; additional films in very high-risk infants.
- 90. • RICKETS OF PREMATURITY • Prevention. • Adequate amounts of calcium, phosphorus & vitamin D decreases the risk of rickets of prematurity. • Parenteral nutrition is often necessary initially in very premature infants. Current amino acid preparations allow for higher concentrations of calcium and phosphate. • Early transition to enteral feedings is also helpful. • Soy formula should be avoided because there is decreased bioavailability of calcium and phosphorus.
- 91. • RICKETS OF PREMATURITY • Prevention. • Human milk fortified with calcium & phosphorus or preterm infant formula, which has higher concentrations of calcium and phosphorus than standard formula. • Increased mineral feedings should continue until the infant weighs 3–3.5 kg. • These infants should also receive approximately 400 IU/day of vitamin D via formula and vitamin supplements. • Treatment. • Ensure adequate calcium, phosphorus, and vitamin D.
- 92. T h a n k y o u . . .
Notas del editor
- CA, PHOSPH, ALK.PHOSH, VID D VARIOUS FORMS,
