Treatment of failed roux en-y hepaticojejunostomy after post cholecystectomy bile duct injuries
- 1. Treatment of failed Roux-en-Y hepaticojejunostomy after post-cholecystectomy bile ducts injuries Amine Benkabbou, MD,a Denis Castaing, MD,a,b,c Chady Salloum, MD,a Ren Adam, MD, PhD,a,c,d e Daniel Azoulay, MD, PhD,a,c and Eric Vibert, MD, PhD,a,b,c Villejuif, France Background. Roux-en-Y hepaticojejunostomy (RYHJ) is the most well-accepted treatment for most post- cholecystectomy bile duct injuries (BDI). RYHJ failure is a complex situation that requires expert planning and the possibility of using a combination of operative, radiologic, and endoscopic techniques. The aim of this study was to report our experience with a multidisciplinary approach to failed RYHJ after post-cholecystectomy BDI. Methods. Between January 1996 and March 2008, 44 consecutive patients were managed for RYHJ failure in our department. They presented with recurrent cholangitis in 40 patients (91%) and/or jaundice in 9 (20%). First-line treatment consisted of primary revisionary surgery in 26 cases (59%; repeat RYHJ in 22 and hepatectomy in 4) and a percutaneous approach in 18 cases (41%; biliary interventions in 16 and portal vein embolization in 2). Results. Postoperative mortality was nil. Postoperative morbidity was 11% after repeat RYHJ without hepatectomy, 80% (bile leaks) after hepatectomy, and 10% (mild cholangitis and hemobilia) after a percutaneous approach. Delayed revisionary surgery with the intent to wait for bile duct dilation failed in all 5 patients. With a mean follow-up of 49 ± 40 months, second- or third-line treatment was attempted in 7 patients (16%). One patient (2%) died because of suicide. Overall clinical success defined by the absence of incapacitating biliary symptoms after treatment was achieved in 39 patients (89%). Conclusion. An immediate, multidisciplinary approach including repeat biliary surgery and/or a percutaneous approach in a tertiary hepatobiliary center is required to obtain good, long-term results when treating the failure of RYHJ post-cholecystectomy BDI. (Surgery 2013;153:95-102.) From the AH-HP,a H^pital Paul Brousse, Centre Hpato-Biliaire, Inserm,b Unite 785, the Universit o e e Paris-Sud,c and Inserm,d Unite 776, Villejuif, France ROUX-EN-Y HEPATICOJEJUNOSTOMY (RYHJ) is the stan- of this complex situation requires careful and ex- dard treatment for most post cholecystectomy bile pert management and the possibility of having a duct injuries (BDI) with long-term clinical success combination of operative, radiologic, and endo- rates reaching 90%.1 Some patients who undergo scopic techniques. Few reports have specifically RYHJ for BDI will experience incapacitating biliary analyzed the results of failed biliary repairs for symptoms, such as jaundice or recurrent cholangi- post-cholecystectomy BDI.2-6 The aim of our study tis.2 However, in addition to anastomotic stricture, was to evaluate the short- and long-term results of several other, isolated or associated pathogenic fac- a multidisciplinary approach regarding failed tors for RYHJ failure include intrahepatic calculi, RYHJ after post-cholecystectomy BDI. intrahepatic stricture, and improper technical construction of the Roux-en-Y limb. Management PATIENTS AND METHODS Between January 1996 and March 2008, 44 Accepted for publication June 14, 2012. consecutive patients were treated in our depart- Reprint requests: Eric Vibert, MD, PhD, 12 avenue Paul Vaillant ment (Centre Hpato-Biliaire, Paul Brousse Hos- e Couturier, 94804 Villejuif Cedex, France. E-mail: eric.vibert@ pital, Assistance Publique des Hopitaux de Paris, pbr.aphp.fr. Villejuif, France) for the failure of RYHJ per- 0039-6060/$ - see front matter formed because of post-cholecystectomy BDI. Ó 2013 Mosby, Inc. All rights reserved. Our group of patients comprised 13 males (30%) http://dx.doi.org/10.1016/j.surg.2012.06.028 and 31 females (70%) with a mean (± SD) age of SURGERY 95
- 2. 96 Benkabbou et al Surgery January 2013 Table I. Serum biochemistry findings at referral Normal range Median Min Max PT (%) 70 94 68 100 Bilirubin (mmol/L) 17 13 5 134 AP (UI/L) 120 183 123 1,128 GGT (UI/L) 50 210 52 2,074 AST (UI/L) 35 48 15 491 ALT (UI/L) 43 62 9 776 Creatinine (mmol/L) 18–106 64 47 140 Protein (g/L) 60–80 71 48 80 Albumin (g/L) 38 41 29 50 Leukocytes (N./mL) 4,800–10,800 6,150 3,240 14,800 Hemoglobin (g/dL) 12–16 12.9 8 15.8 Platelets (N.103/mL) 150–400 256 85 658 ALT, Alanine aminotransferase; AP, alkaline phosphatase; AST, aspartate aminotransferase; GGT, gamma glutamyl transferase; PT, prothrombin time. 51 ± 14 years (range, 17–78). All BDI were abnormalities were present (Table I). Leukocytosis sustained during cholecystectomy performed and thrombocytopenia were present in 3 patients for cholecystolithiasis. The approach for the cho- (7%) and 1 patient (2%), respectively. lecystectomy was laparoscopic in 35 patients (80%) Vascular and liver parenchymal assessments and open in 9 patients (20%). The level of BDI was (Table II) were performed using routine abdominal assessed according to Bismuth’s classification (7): ultrasonography and computed tomography of the Type 1 in 2 patients (5%), type 2 in 18 (41%), type liver with intravenous contrast. These imaging mo- 3 in 12 (27%), type 4 in 5 (11%), and type 5 in 7 dalities revealed liver atrophy in 7 patients (16%), (16%). The time elapsing between BDI and initial and evidence of injury to the main (2 patients repair (RYHJ) was a median of 6 days (range, 0– [4%]) or right branch (6 patients [14%]) of the he- 703). The initial repair was performed very early patic artery injury in 8 patients (18%). Liver atrophy (48 hours) in 9 patients (20%), early (45 days) and vascular injury were both present in 2 patients. in 22 (50%), and delayed (45 days) in 13 (30%). Biliary assessments were performed using per- The BDI was incurred and the failed RYHJ was cutaneous cholangiography in 34 patients (77%) performed in the same hospital in 34 patients and/or magnetic resonance cholangiography in 23 (72%). Before referral to our department, an (52%). These procedures revealed intrahepatic initial revisionary operation for the failed RYHJ calculi in 18 patients (41%) and bile duct dilation was performed in 10 patients (23%), and involved in 11 (25%). The level of obstruction was suspected a hepaticojejunostomy repair in 3 patients, Roux- to be hilar or suprahilar in 39 patients (89%). en-Y limb repair in 2 patients, and percutaneous Treatment strategy was defined at a multidisci- dilatation of a stricture in 5 patients. These 10 plinary staff meeting including surgeons, radiolo- patients were referred to our department because gists, and hepatogastroenterologists during a of persistent biliary symptoms despite this revision- case-by-case analysis in our tertiary center that offers ary operation. different multidisciplinary approaches to hepato- The patients were admitted to our department biliary disorders (operative, endoscopy and inter- for recurrent cholangitis in 40 patients (91%) ventional radiology). The treatment strategy and/or jaundice in 9 (20%). Recurrent cholangitis comprised 2 types of treatments: Revisionary sur- was defined as fever 388C or episodic right upper gery, including a revision of hepaticojejunostomy quadrant pain with no identifiable source outside and/or hepatectomy, or a percutaneous approach, the hepatobiliary system occurring a minimum of 3 including biliary maneuvers and/or portal vein times in the preceding year. Continuous or inter- embolization. These treatments were performed mittent biliary symptoms had developed within a alone or in combination and subsequently defined median period 4 months (range, 0–204) since the the different lines of treatment in the same patient. pre-referral procedure. An external biliary drain Revisionary surgery was considered in patients was present in 7 patients (16%), and no patient in good general condition without uncontrolled had an active bile leak. biliary sepsis and was designed to perform an end- Cholestasis had been present in all patients. No to-side, wide, healthy, mucosa–mucosa hepaticoje- major coagulation and renal function junostomy without tension and with a 70-cm long
- 3. Surgery Benkabbou et al 97 Volume 153, Number 1 Table II. Radiologic findings at referral bile duct. A hepatotomy between segments 5 and 4 Findings n through of the bed of the gallbladder was used to access the secondary right biliary confluence. Calculi 18 (41%) Visual magnifying aids were used routinely to Bile duct dilation 18 (41%) optimize biliary dissection, the recognition of Bilateral 11 healthy mucosa, and the anastomoses. These anas- Left liver 4 Right liver 1 tomoses were performed using 5/0 or 6/0 inter- Right sector 2 rupted, nonabsorbable, monofilament sutures with Vascular injury 8 (18%) the knots tied on the external surface of the Right branch of hepatic artery 6 anastomosis. An ultrasonic dissector and bipolar Hepatic artery 2 coagulation forceps were used routinely during any Parenchymal liver atrophy 7 (16%) hepatectomy. Right liver 5 Percutaneous approaches. All percutaneous Left lateral lobe 1 procedures were carried out in the operating Segment 4 1 room under full aseptic conditions as applicable Level of biliary obstruction to any operative procedure.7 The operating suite Infrahilar 5 (11%) was equipped with a Doppler Ultrasound (Aloka Hilar 25 (57%) Suprahilar 14 (32%) SSD 680, Aloka, Tokyo, Japan) and a light ampli- fier (Diasonics 3800; Diasonics, Milpitas, CA). These procedures were performed under either local anesthesia, neuroleptic analgesia with pre- retrocolic Roux-en-Y limb. In patients with a lon- medication, or general anesthesia with intubation gitudinal stricture extending into the intrahepatic if the duration of the procedure was expected to bile ducts, associated with liver atrophy, a hepatec- be of a greater duration. Biliary maneuvers con- tomy was performed with or without RYHJ revi- sisted of 3 successive stages: Establishing adequate sion. A percutaneous approach was considered in transhepatic and/or transjejunal8 access to the patients with a (1) marked worsening in their biliary tract if not present, performing the re- general condition or hepatic function, or severe quired intervention, and obtaining a contrast sepsis, all of which contraindicated an operative study to demonstrate if the procedure was success- procedure, (2) a local contraindication at the level ful. When necessary, endoscopic control of the of the bile duct owing to a cavernous transforma- procedure was ensured using a pediatric broncho- tion of a thrombosed portal vein or after numer- scope (diameter, 4 mm). Strictures were treated ous previous biliary interventions, or (3) an by balloon dilatation and calculi by extraction isolated short intra-hepatic biliary stricture.7 Portal and/or lithotripsy (Lithotron EL27, Walz Elektro- vein embolization was performed in patients with nik GMBH, Germany). Portal vein embolization an isolated longitudinal intrahepatic biliary stric- was performed via a transhepatic approach. ture in attempt to induce parenchymal atrophy Follow-up data were obtained by means of in the distribution of the diseased bile ducts. review of hospital and outpatient records. All Techniques of revisionary surgery. An end-to- patients were seen 1 month after hospital dis- side, wide, healthy, mucosa–mucosa hepaticojeju- charge and underwent computed tomography nostomy without tension and with a 70-cm long and a complete biochemical assessment. Thereaf- retrocolic Roux-en-Y limb was the goal in each ter, they were followed with liver ultrasonography patient. Operative exploration consisted of 3 stages: every 4 months during the first year and every 6 Verification of the erroneous construction of the months for 2 years, and the yearly thereafter. Roux-en-Y limb, exposure of the anastomotic area Postoperative morbidity was assessed according to with collection of a sample of bile, and assessment the Clavien-Dindo classification.9 Clinical outcome of biliary anatomy and/or abnormalities (calculi, was determined according to the Terblanche classi- stricture) using intraoperative cholangiography. fication10: grade I, no biliary symptoms; grade II, When feasible in patients with intra-hepatic bile transitory symptoms and no current symptoms; duct dilation, a preoperative transhepatic cholan- grade III, biliary symptoms requiring medical giography followed by transhepatic biliary drainage therapy; and grade IV, recurrent biliary symptoms was performed. Intraoperatively, this drainage was requiring correction or related to death. Ter- very useful in localizing the bile duct after removal blanche class IV constituted a poor result. Ter- of the RYHJ and dissecting the hilar plate to expose blanche I, II, and III constituted a clinical success the primary biliary confluence and notably the left with excellent, good, and fair results, respectively.
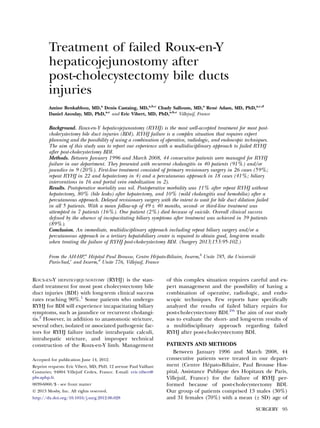
- 4. 98 Benkabbou et al Surgery January 2013 RESULTS thus optimize revision. None of these patients The mean (± SD) follow-up period was 49 ± 40 developed bile duct dilation after a mean of months (range, 2–153). One patient (2%) died as waiting time of 20 ± 17 months. During this period, a result of suicide 44 months after the initial 4 patients developed recurrent cholangitis. Liver hepatectomy. In 7 patients (16%), $2 treatments abscess and pylephlebitis of the right portal branch were required, with a mean follow-up of 33 ± 36 occurred in 1 patient with a previous injury of the months (range, 2–85). At the time of last follow- right branch of the hepatic artery. up, clinical success had been achieved in 39 Revisionary surgery without hepatectomy (n = 26 pro- patients (89%): 34 patients (77%) were asymptom- cedures in 25 patients): Revisionary surgery without atic (Terblanche I–II), and 5 patients (11%) had hepatectomy was performed as first-line treatment experienced an improvement in their symptoms in 22 patients, as second-line treatment in 3 (Terblanche III). The overall result was poor patients (after a percutaneous approach), and as (Terblanche IV) in 5 patients (11%). An overview third-line treatment in 1 patient (after revisionary of the results is shown in Fig 1. First-line treatment surgery followed by a second-line percutaneous (Fig 2) consisted of primary revision surgery (first- approach). Morbidity occurred after 3 of 26 pro- line revisionary surgery) in 26 patients (59%) and cedures (11%): Abdominal hematoma managed a percutaneous approach (first-line percutaneous with transfusion in 1 patient (Clavien-Dindo II), approach) in 18 patients (41%). cholangitis managed with antibiotics in 1 (Clavien- First-line revisionary surgery (n = 26 [59%]; Dindo II), and acute pancreatitis that required Table III). The Roux-en-Y limb was found to be exploratory laparotomy for suspected biliary peri- short (70 cm) in 12 patients (44%) and was re- tonitis in 1 (Clavien-Dindo IIIb). modeled to a length of 70 cm. Revisionary surgery Revisionary surgery with hepatectomy (n = 5 proce- included repeat hepaticojejunostomy in 23 patients dures in 4 patients): Hepatectomy was performed (89%), which involved more than a single duct in as first-line treatment in 4 patients and as second- 13 (54%; (range, 1–5). In 3 patients (11%), revi- line treatment in one who underwent operation sionary surgery was suboptimal because an anasto- twice. Bile leaks occurred after 4 procedures mosis of the isolated right sector duct (1 case) or (80%). Morbidity occurred as Clavien-Dindo II segment 4 duct (2 cases) was impossible. Drains after 3 procedures and Clavien-Dindo IIIb after were placed through the hepaticojejunostomy in 4 1 first-line procedure complicated by a bilio- patients (17%). An access limb of jejunum was pleural fistula managed with prolonged drainage placed under the abdominal wall to enable subse- that progressed to a chronic external fistula re- quent percutaneous access in 3 patients (13%). quiring repeat hepatectomy. Hepatectomy was performed in 4 patients (15%) in- Percutaneous approach (n = 120 procedures in 21 pa- cluding 2 right hepatectomies, 1 left hepatectomy, tients): A percutaneous approach was adopted as and 1 left lateral sectionectomy). first-line treatment in 18 patients and as addi- First-line percutaneous approach (n = 18 [41%]; tional treatment in 3 (after initial revisionary Table IV). Access to the biliary tract was established surgery). In 1 patient, additional treatment con- by catheterization of the jejunal limb (the ‘‘cul-de- sisted of a combination of biliary maneuvers and sac’’) in 9 patients (54%), transhepatic catheteriza- right sectoral portal vein embolization. There was tion in 4 patients (23%), or combined techniques no mortality. No morbidity was observed after in 4 (23%). The procedures were performed un- portal vein embolization. Hemobilia that did not der biliary endoscopic control in 12 patients require a blood transfusion (Clavien-Dindo I) (27%). Balloon dilatation of a stricture, extraction and/or cholangitis managed with IV antibiotics of calculi and/or biliary cast, and lithotripsy were (Clavien-Dindo I) occurred after 10% of the performed in 12 (70%), 8 (47%), and 4 patients biliary interventions. (23%), respectively. In 2 patients with calculi, su- Long-term results. Revisionary surgery without tures exposed in the bile duct lumen were re- hepatectomy (n = 22 patients): Satisfactory primary moved percutaneously under endoscopic control results were achieved in 18 patients (82%): 17 via access of the jejunal limb. Transhepatic portal patients (94%) became asymptomatic (Terblanche vein embolization was performed in 2 patients I–II) and 1 patient (6%) improved, although with (right posterior sectoral portal branch and right some symptoms (Terblanche III). In 4 patients portal branch). (9%), the symptoms did not improve (Terblanche Short-term results. In 5 patients (20%), first-line IV). One of these patients experienced generally revisionary surgery was delayed at referral in at- fair results (Terblanche III) after an additional tempt to wait for bile duct dilation to develop and percutaneous approach.
- 5. Surgery Benkabbou et al 99 Volume 153, Number 1 Fig 1. Overview of the results as a function of the Terblanche classification of 44 patients, achieved with 1, 2 or 3 step(s). HJ, Hepaticojejunostomy; PVE, portal vein embolization; T, Terblanche classification10; TI, no biliary symptoms; TII, transitory biliary symptoms, no current symptoms; TIII, biliary symptoms requiring medical therapy; TIV, recurrent bil- iary symptoms requiring correction or related to death. and 4 (29%) had improvement in their symptoms (Terblanche III). In 2 patients (6%), the symptoms were not primarily improved (Terblanche IV), but both became asymptomatic (Terblanche I–II) after further revisionary surgery. Portal vein embolization (n = 2 patients): Poor results were obtained in these 2 patients. One patient who underwent portal vein embolization alone had overall good results (Terblanche II) after additional revisionary surgery, whereas the second with initial combined portal vein emboli- zation and biliary interventions was listed for liver transplantation because of development of second- ary biliary cirrhosis. Fig 2. Overall results of the revisionary approach. Full line: Overall results including additional revision. Dotted DISCUSSION line: Results after first-line revision. This study shows that with an experienced multidisciplinary approach (according to the strat- Revision surgery with hepatectomy (n = 4 patients): egy summarized in Fig 3), patients with a failed Good primary results were achieved in 3/4 patients RYHJ after post-cholecystectomy BDI can achieve who were asymptomatic (Terblanche I–II), but the good long-term clinical success in 89%. These re- symptoms did not improve in the other patient. sults required more than the first-line revision in This patient (Terblanche IV) underwent addi- 16% of patients. Although we showed that waiting tional repeat hepatectomy for a bile leak from an for bile duct dilation before revisionary surgery was excluded segment 4 with histologic evidence of not successful; moreover, we were unable to iden- secondary biliary cirrhosis, but this procedure tify any prognostic predictive factor at referral in failed. She died from suicide. our small and heterogeneous population. Biliary interventions (n = 16 patients): Good pri- Concordant data suggest that both repair of mary results were achieved in 14 patients (87%): BDI repair by an expert hepatobiliary surgeon11 10 (71%) were asymptomatic (Terblanche I–II) and a multidisciplinary approach involving
- 6. 100 Benkabbou et al Surgery January 2013 Table III. Revisionary surgery procedures (n = 31) Table IV. Percutaneous approach procedures First line Additional (n = 21) (n = 26) (n = 5*) First line Additional (n = 18) (n = 3) Hepaticojejunostomy revision 23 (88%) 4 (80%) Number of ducts/anastomosis Portal vein embolization 2 (11%) 1 1 13 2 Right branch 1 — 2 5 1 Right posterior sector branch 1 1 3 6 — Biliary maneuvers 17 (94%) 3 (100%) 4 1 1 Catheterization approach 5 1 — Transhepatic 9 1 Endobiliary extraction 18 (69%) 2 (40%) Transjejunal 4 — Calculi and/or biliary cast 15 2 Combined 4 2 Clips 2 — Endoscopic control 12 (67%) 2 Alimentary 1 1 Procedures R-en-Y revision with 12 (46%) 0 Stricture dilatation 12 (70%) 3 Hepatectomy 4 (15%) 1 (20%) Calculi and/or biliary cast 8 (47%) 1 Right liver 2 — extraction Left liver 2 — Lithotripsy 4 (23%) 1 Left lateral lobe 1 — Suture extraction 2 (12%) — Segment 4 (excluded bile leak) — 1 Median number of procedures 5 (2–23) 10 (2–24) *Second-line in 4 patients and third-line in 1 patient. (range) gastroenterologists, radiologists, and surgeons12 favorably affects outcomes. RYHJ has been success- although at the time of initial biliary repair only fully used in such cases since the 1970s13 and is cur- 38% of them had an injury or stricture at that level. rently the standard treatment, with success rates Hence, a precise assessment of bile duct anatomy of up to 91% and very long-term (10 years) and the level of the stricture are critical to the stricture-free survival.14,15 Nevertheless, $10% of success of any revisionary strategy.4,16 In this set- these patients will suffer from a failure of the ting, percutaneous cholangiography can be consid- RYHJ.2 ered as the ‘‘gold standard’’ because it provides This failure involves isolated or associated critical information on the biliary anatomy and pathogenic factors responsible for recurrent epi- ductal communication. Magnetic resonance chol- sodes of cholangitis in 90% of patients and/or angiography has been claimed to be as reliable as jaundice in 20%.16 These symptoms of biliary ob- the percutaneous approach in defining biliary struction may occur without anastomotic stricture tree anatomy20 and may be the procedure of and are possibly caused by the passage of calculi choice in selected patients. or by enterobiliary reflux induced by inappropri- The second major problem encountered in the ate construction of the Roux-en-Y limb.2 Between management of RYHJ failure is an absence of intra- 80% and 90% of patients with failure of the biliary hepatic bile duct dilation that complicates the repair develop symptoms within 5–7 years.3,17 This biliary repair. This situation was observed in 59% delay can vary from a few days to several years18 (a of our patients. It should be noted that revisionary maximum of 17 years in our series), which empha- surgery was delayed in 5 patients specifically to wait sizes the need for prolonged follow-up. By con- for bile duct dilation, but this strategy failed in all 5 trast, some patients who are clinically ‘‘normal’’ patients and was associated with severe morbidity after repair can continue to experience mild during the waiting period. We, therefore, consider increases in serum bilirubin and/or gamma glu- that when surgical revision criteria are fulfilled, an tamyl transferase activity during long-term fol- elective procedure assisted by the routine use of low-up.19 optical magnification should be scheduled without The management of RYHJ failure is hampered waiting for bile duct dilation. by the fact that biliary strictures are found at a From a technical point of view, if the biliary higher level than before the first attempt at BDI confluence is intact, a wide stoma of healthy duct repair. Indeed, with each failed attempt, the level can be achieved by extending the opening in the of the scarred biliary stricture recedes higher into bile duct to the extrahepatic portion of the left the hepatic hilum. In our experience, 89% of hepatic duct.21 If the biliary confluence is obliter- referred patients had hilar or suprahilar strictures, ated, and the left and right hepatic ducts are
- 7. Surgery Benkabbou et al 101 Volume 153, Number 1 Fig 3. Initial treatment algorithm in failed RYHJ after post-cholecystectomy BDI. isolated, hilar plate dissection is necessary up to analysis and an immediate multidisciplinary ap- the level at which a healthy duct can be found. proach in tertiary hepatobiliary centers. When the results of revision of the hepaticojeju- nostomy are expected to be problematic because REFERENCES of a suprahilar longitudinal stricture and/or liver 1. Murr MM, Gigot JF, Nagorney DM, Harmsen WS, Ilstrup atrophy, hepatectomy must be considered. The ra- DM, Farnell MB. Long-term results of biliary reconstruction tionale for partial liver resection in patients with after laparoscopic bile duct injuries. Arch Surg 1999;134: complex RYHJ failure is that hepatectomy removes 604-9. 2. Kozicki I, Bielecki K, Kawalski A, Krolicki L. Repeated re- irreversible fibrotic parenchyma and prevents the construction for recurrent benign bile duct stricture. Br J progressive liver damage caused by permanent Surg 1994;81:677-9. bile stasis and/or recurrent cholangitis.1,22 Hepa- 3. Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stric- tectomy with biliary reconstruction in the setting ture. Patterns of recurrence and outcome of surgical ther- of complex BDI produces excellent long-term re- apy. Am J Surg 1984;147:175-80. 4. Chaudhary A, Chandra A, Negi SS, Sachdev A. Reoperative sults despite a high rate of severe postoperative surgery for postcholecystectomy bile duct injuries. Dig Surg complications.22 Total hepatectomy followed by 2002;19:22-7. liver transplantation has been considered when re- 5. Walsh RM, Vogt DP, Ponsky JL, Brown N, Mascha E, Hen- visionary surgery and percutaneous approaches derson JM. Management of failed biliary repairs for major have failed or were not technically feasible in the bile duct injuries after laparoscopic cholecystectomy. J Am Coll Surg 2004;199:192-7. presence of diffuse, secondary biliary cirrhosis.23,24 6. Pottakkat B, Sikora SS, Kumar A, Saxena R, Kapoor VK. Re- In difficult cases, and especially in patients who current bile duct stricture: causes and long-term results of have undergone $2 previous operative repairs surgical management. J Hepatobiliary Pancreat Surg 2007; and/or in whom portal hypertension is present,4 14:171-6. a percutaneous biliary approach is very useful to as- 7. Castaing D, Vibert E, Bhangui P, Salloum C, Smail A, Adam R, et al. Results of percutaneous manoeuvres in biliary dis- sess the precise level of the stricture and the health ease: the Paul Brousse experience. Surg Endosc 2011;25: of the mucosa. In this setting, endoluminal dilata- 1858-65. tion associated with complete extraction of all in- 8. Castaing D, Azoulay D, Bismuth H. [Percutaneous catheter- traductal debris may represent either a chance ization of the intestinal loop of hepatico-jejunostomy: a new for long-term remission or a step toward revision- possibility in the treatment of complex biliary diseases]. Gastroenterol Clin Biol 1999;23:882-6. ary surgery.7 9. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, In conclusion, good long-term results can be Schulick RD, et al. The Clavien-Dindo classification of surgi- achieved after a failed RYHJ failure after post- cal complications: five-year experience. Ann Surg 2009;250: cholecystectomy BDI by means of a case-by-case 187-96.
- 8. 102 Benkabbou et al Surgery January 2013 10. Terblanche J, Worthley CS, Spence RA, Krige JE. High or 18. Tocchi A, Costa G, Lepre L, Liotta G, Mazzoni G, Sita A. low hepaticojejunostomy for bile duct strictures? Surgery The long-term outcome of hepaticojejunostomy in the 1990;108:828-34. treatment of benign bile duct strictures. Ann Surg 1996; 11. Stewart L, Way LW. Bile duct injuries during laparoscopic 224:162-7. cholecystectomy. Factors that influence the results of treat- 19. Fialkowski EA, Winslow ER, Scott MG, Hawkins WG, Line- ment. Arch Surg 1995;130:1123-8. han DC, Strasberg SM. Establishing normal values for liver 12. de Reuver PR, Rauws EA, Bruno MJ, Lameris JS, Busch OR, function tests after reconstruction of biliary injuries. J Am van Gulik TM, et al. Survival in bile duct injury patients after Coll Surg 2008;207:705-9. laparoscopic cholecystectomy: a multidisciplinary approach 20. Chaudhary A, Negi SS, Puri SK, Narang P. Comparison of of gastroenterologists, radiologists, and surgeons. Surgery magnetic resonance cholangiography and percutaneous 2007;142:1-9. transhepatic cholangiography in the evaluation of bile 13. Bismuth H, Franco D, Corlette MB, Hepp J. Long term duct strictures after cholecystectomy. Br J Surg 2002;89: results of Roux-en-Y hepaticojejunostomy. Surg Gynecol 433-6. Obstet 1978;146:161-7. 21. Hepp J. Hepaticojejunostomy using the left biliary trunk for 14. Chapman WC, Halevy A, Blumgart LH, Benjamin IS. Post- iatrogenic biliary lesions: the French connection. World J cholecystectomy bile duct strictures. Management and out- Surg 1985;9:507-11. come in 130 patients. Arch Surg 1995;130:597-602. 22. Laurent A, Sauvanet A, Farges O, Watrin T, Rivkine E, Bel- 15. Gigot JF. Bile duct injury during laparoscopic cholecystec- ghiti J. Major hepatectomy for the treatment of complex tomy: risk factors, mechanisms, type, severity and immedi- bile duct injury. Ann Surg 2008;248:77-83. ate detection. Acta Chir Belg 2003;103:154-60. 23. Nordin A, Makisalo H, Isoniemi H, Halme L, Lindgren L, 16. Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Hockerstedt K. Iatrogenic lesion at cholecystectomy re- Talamini MA, et al. Postoperative bile duct strictures: manage- sulting in liver transplantation. Transplant Proc 2001;33: ment and outcome in the 1990s. Ann Surg 2000;232:430-41. 2499-500. 17. Pitt HA, Miyamoto T, Parapatis SK, Tompkins RK, Longmire 24. Thomson BN, Parks RW, Madhavan KK, Garden OJ. Liver WP Jr. Factors influencing outcome in patients with postop- resection and transplantation in the management of iatro- erative biliary strictures. Am J Surg 1982;144:14-21. genic biliary injury. World J Surg 2007;31:2363-9.
