Pediatric Advanced Life Support Update for the Emergency Physician: Review of 2010 Guideline Changes
- 1. Abstract: Important changes were introduced in the 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Cardiac arrest remains a leading cause of death in many parts of the world, and despite important advances in medical science, the outcome of cardiopulmonary arrest is poor. The fundamental changes in the American Heart Association 2010 guidelines include the new recommendation to begin resuscitation with chest compression, airway, and breathing. We will review and discuss how to approach a successful pediatric resuscitation with the maintenance of adequate coronary artery and cerebral artery perfusion and, ultimately, how to improve outcomes in infants and children. Keywords: cardiopulmonary resuscitation; C-A-B; chest compression; bag valve mask; endotracheal tube; end-tidal CO2; intraosseous; automatic external defibrillator; dysrhythmia; defibrillation; therapeutic hypothermia; termination of resuscitation Department of Pediatrics, Division of Emergency Medicine, Children's Hospital at Montefiore/Albert Einstein College of Medicine, Bronx, NY. Reprint requests and correspondence: Waseem Hafeez, MD, is to be contacted at Department of Pediatrics, Division of Emergency Medicine, Children's Hospital at Montefiore/Albert Einstein College of Medicine, 3315 Rochambeau Avenue, Bronx, NY 10467. Lorraine Ronca, DO, Theresa Maldonado, MD. whafeez@montefiore.org (W. Hafeez), lronca@montefiore.org (L.T. Ronca), tmaldona@montefiore.org (T.E. Maldonado) 1522-8401/$ - see front matter © 2011 Elsevier Inc. All rights reserved. Pediatric Advanced Life Support Update for the Emergency Physician: Review of 2010 Guideline Changes Waseem Hafeez, MD, Lorraine T. Ronca, DO, Theresa E. Maldonado, MD A 6-month-old female infant was brought into the emergency department (ED) by her mother for respiratory distress. The patient had emesis and diarrhea for the past day and was “not breathing right” since the morning. The infant appeared very pale and was obtunded with agonal respirations. Her fontanelle was sunken, and there was no visible capillary refill. Her tone was limp. Her extremities were cool, and a pulse could not be detected immediately. Chest compressions were begun at a rate of 100/min, at a depth of 1.5 in, using 2 thumbs with the hands encircling the chest. PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO • VOL. 12, NO. 4 255
- 2. 256 VOL. 12, NO. 4 • PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO Compressions were begun immediately because the patient was unresponsive with abnormal breathing and no detection of a pulse within 10 seconds. After 30 compressions were given, the airway was opened with head tilt–chin lift, and no spontaneous respirations were observed. “Look, listen and feel” has been removed from the sequence. Two breaths were delivered with a bag valve mask (BVM) device, and good chest rise was observed. Two effective breaths at 1 second per breath were given with a 450-mL-sized bag connected to an oxygen flow rate of 10 to 15 L/min. The compressionto-ventilation ratio was 15:2, as more than 2 rescuers were present. For 1 cardiopulmonary resuscitation (CPR) rescuer in all ages, a 30:2 ratio is recommended. The patient was intubated with a 3.5-mm (internal diameter) cuffed endotracheal tube (ETT). Cuffed tubes may be used in all ages. Cricoid pressure is no longer recommended. Tube placement was confirmed by physical examination, auscultation, exhaled CO2 detector, and pulse oximeter. Ventilation was provided at 8 to 10 breaths/min. Endotracheal tube placement should be confirmed by capnography. Breathing rate with an advanced airway is 8 to 10 breaths/ min in all ages. Vascular access was not able to be obtained within the first 90 seconds. An intraosseous (IO) needle was inserted into the right tibia. Blood was sent for analysis. Early IO placement is now recommended in all ages if intravascular (IV) access is not available in less than 90 seconds. Further history and physical examination revealed the following: the patient has Bartter syndrome (genetic renal disorder resulting in hyponatremic, hypokalemic metabolic alkalosis) and receives potassium chloride (KCl) supplements, spironolactone, indomethacin, and simethicone at home. She had a gastrostomy tube in place and a Broviac catheter inserted into the right chest. She was discharged from the hospital 5 days ago for treatment of low serum potassium. Upon discharge, the dose of KCl was increased. The cardiac monitor showed a wide-complex ventricular tachycardia (VT) at a rate of 183/min, and no pulse was palpated at the femoral artery. It was determined that the patient was in pulseless VT. While the defibrillator was charging, CPR was continued. Defibrillation with a dose of 2 J/kg was given, and CPR was immediately resumed. The patient was still in pulseless VT, so a second defibrillation dose was given at 4 J/kg followed by epinephrine (0.1 mL/kg of 1:10 000 solution) at a dose of 0.01 mg/kg, and CPR was continued. Cardiopulmonary resuscitation and defibrillation are critical in the management of pulseless VT and ventricular fibrillation (VF). High-dose epinephrine 1:1000 is not recommended for IV or IO dosing, only for ETT delivery. Because the patient did not revert to a perfusing rhythm, defibrillation at 4 J/kg was delivered, followed by amiodarone, 5 mg/kg. Another shock of 4 J/kg and 1 mg/kg of lidocaine was given while CPR was continuously delivered except during delivery of shocks. Recommended sequence for defibrillation is as follows: CPR Y shock (2 J/kg) Y CPR Y shock (4 J/kg) Y drug Y CPR Y shock (4 J/kg). Laboratory analysis of blood revealed the following: for arterial blood gas—pH 7.11, PCO2 46 mm Hg, PO2 120 mm Hg, and HCO3 6 mEq/L, and for serum chemistry—sodium 144 mEq/L, potassium 13 mEq/L, CO2 6 mEq/L, glucose 194 mg/dL, blood urea nitrogen 18 mg/dL, creatinine 0.9 mg/dL, and calcium 6 mg/dL. A 12-lead electrocardiogram (ECG) revealed VT with peaked T waves at a rate of 183/min. Hyperkalemia was immediately treated with calcium chloride, insulin, glucose, sodium bicarbonate, furosemide, and Kayexalate. Identification and treatment of the underlying causes of any pulseless electrical activity (PEA) are imperative. Five Hs and 5 Ps are the most common causes: hypoxemia, hypovolemia, hypoglycemia, hypothermia, hypokalemia/hyperkalemia, pneumothorax, pericardial tamponade, pH—severe acidosis, pulmonary embolism, and poison overdose/toxicology. The repeat potassium level was 6 mEq/L, and the patient converted to normal sinus rhythm and transferred to the pediatric intensive care unit for further management. The pulse oximeter was maintained at 98% while she was in the ED. Arterial oxyhemoglobin saturation was maintained at least 94% but less than 100% to limit the risks of hyperoxemia. PALS SCIENCE UPDATE 2010 This case highlights some important changes that were introduced in the most recent recommendations in the 2010 American Heart Association (AHA) guidelines for CPR and emergency cardiovascular care. These changes mark the 50th anniversary of the landmark 1960 recommendations when researchers combined breaths and compressions to create CPR as we know it today. In 1966, the AHA developed the first CPR guidelines and has periodically updated its recommendations based on research data and clinical experience. 1 In 1992, the International Liaison Committee on Resuscitation, an international consortium of the world's resuscitation councils, was formed to periodically review the current resuscitation literature and issue consensus treatment guidelines. Despite important advances in medical science, cardiac arrest remains a leading cause of death in
- 3. PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO • VOL. 12, NO. 4 257 many parts of the world. In the United States and Canada, every year approximately 350 000 people (almost half of them in-hospital) have cardiac arrest and receive attempted resuscitation. 2 Approximately 25% of patients present with pulseless ventricular arrhythmias and have a better outcome than those who present with asystole or PEA. 3 The outcome of unwitnessed cardiopulmonary arrest in infants and children is poor. Infants are less likely to survive out-of-hospital cardiac arrest than children or adolescents. 4 Only 6% of pediatric patients who have out-of-hospital cardiac arrest survive to discharge, and most are neurologically impaired, whereas the in-hospital survival rate is 27% with a better neurologic outcome. 2,4 Pulseless arrests (PEA/asystole) have the poorest outcome, whereas infants and children with a pulse but with poor perfusion and bradycardia had the best survival (64%) to discharge. For out-of-hospital respiratory arrest and primary VF, bystander resuscitation has had a substantial impact on survival with good neurologic outcome. 5,6 A review of the evidence over the last few years has revealed that rapid and effective CPR administered by a lay rescuer resulted in a successful return of spontaneous circulation (ROSC) with neurologically intact survival in children after out-of-hospital cardiac arrest. 7 The increased use of the automatic external defibrillator (AED) in children with sudden out-of-hospital witnessed arrest secondary to primary VF resulted in survival rates of 20% to 30%. 6 Individuals receiving bystander CPR were 4.5 times more likely to survive and 3 times likely to leave the hospital. Unfortunately, only one third to one half of infants and children who have out-of-hospital cardiopulmonary arrest receive bystander CPR, and when provided, CPR is frequently not begun promptly or done well, even by health care professionals. 7 For untrained rescuers, hands-only chest compression CPR is now approved for the adult victim with sudden collapse. All trained rescuers should provide chest compressions and rescue breaths at a rate of 30:2. At this time, there is insufficient evidence to recommend hands-only CPR in children. 7 HIGHLIGHTS OF PEDIATRIC BASIC LIFE SUPPORT (BLS) AND PALS Pediatric Chain of Survival The critical links in the pediatric cardiac arrest chain of survival are as follows: • Injury prevention and safety • Early CPR–chest compressions and ventilations • Rapid access to emergency medical services —911 • Effective pediatric life support post-cardiac arrest care The leading causes of death in infants and children are congenital malformations, complications of prematurity, sudden infant death syndrome, and injury. 8 The “back to sleep” campaign has been credited with decreasing mortality secondary to sudden infant death syndrome. Motor vehicle crashes are the most common cause of fatal childhood injuries because the rate of survival from traumatic cardiac arrest is rare. 9 Injuries related to accidental or inflicted traumatic events can be prevented by parental education and counseling, the use of passenger safety seats and bicycle helmets, and vigilance for nonaccidental trauma. Check for Response “Look, listen, and feel for breathing” has been removed from the BLS algorithm. 10 In the new “chest compressions first” sequence, breathing is briefly checked as part of a check for cardiac arrest. If the infant or child is unresponsive and not breathing, health care providers may take up to 10 seconds to attempt to feel for a pulse (brachial in an infant and femoral in a child). If, within 10 seconds, the pulse is not palpable, and the victim is unresponsive, not breathing, or only gasping, perform CPR, beginning with chest compressions. Studies show that lay rescuers and many health care providers cannot quickly and reliably determine the presence or absence of a pulse in infants or children; thus, the reliance on the presence of pulse check alone in determining the need for CPR is minimized in the 2010 guidelines. 11 CPR Sequence Change From A-B-C to C-A-B During the past 50 years, the primary emphasis has been to begin resuscitation by the A-B-Cs, the BLS sequence of airway assessment, assisting breathing, and support of circulation. Most adult victims have cardiac arrest as a result of VF or pulseless VT, and the highest survival rates are among patients of all ages who receive immediate chest compression and early defibrillation. 6 The fundamental change in the AHA 2010 guidelines includes the new recommendation to begin resuscitation with C-A-B (chest compression, airway, and breathing). 12 The predominant factor in return of circulation (ROSC) and survival in cardiac arrest victims is the maintenance of adequate coronary artery and cerebral artery perfusion. The most
- 4. 258 VOL. 12, NO. 4 • PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO important concept in understanding the physiology of CPR is the relationship of coronary artery perfusion pressure (CPP) to myocardial blood flow and resuscitation outcome. 13 Ideally, CPP measurement could be used to optimize chest compressions and monitor CPR quality. A measurement of CPP or arterial relaxation (“diastolic”) pressure is accurately done using invasive arterial catheterization, which is unlikely during the initial phase of CPR. Measurement of end-tidal carbon dioxide tension (PETCO2) correlates with CPP and cerebral perfusion pressure and is predictive of the outcomes of CPR. 14 It may be used to monitor the effectiveness of chest compressions during CPR. In persons with sudden cardiac arrest, the bystander rescuer has traditionally been taught to initiate the CPR sequence by opening the airway (which involves head repositioning) and provide breathing (which requires setting up ventilation apparatus and obtaining a proper seal over the mouth), the 2 most difficult and time-consuming tasks for the rescuer, all of which delays the start of CPR. Over the years, the A-B-C technique has been entrenched into everyone so that the lay rescuer who does not feel comfortable doing A (airway) and B (breathing) is unlikely to go on to the C (compression) component. This would explain the reason why so many persons with sudden cardiac arrest receive no bystander CPR. By starting with chest compressions immediately, the most often-cited barriers to performing CPR, A and B, are bypassed. The C-A-B sequence is applicable for infants, children, and adults alike. 10 This recommendation simplifies training and provides consistency to a technique that, for most rescuers, will be used only occasionally. These guidelines are supported by evidence that suggests that participants across the board from physicians to lay people often fail to master CPR skills, with rapid deterioration of learned skills after course completion. 15 Most cardiac arrests in infants and children are primarily respiratory in origin, and resuscitation outcome is best if chest compressions are combined with ventilations. 7 The current recommendation is to individualize the CPR sequence based on the presumed etiology of the arrest. For in-hospital pediatric arrests, health care providers are more likely to work in teams and CPR sequences are often performed simultaneously (chest compressions and rescue breathing), so there is less relevance to which intervention is performed first. During CPR after cardiopulmonary arrest, cardiac output is reduced to approximately 25% to 33% of normal, so oxygen uptake from the lungs and CO2 delivery to the lungs are also reduced. 16 Because both the systemic and pulmonary perfusions are significantly reduced during CPR, oxygen delivery to the heart and brain is limited by blood flow rather than by arterial oxygen content. During the first few minutes of resuscitation, chest compressions are far more important than rescue breaths, and normal ventilation perfusion can be maintained with a lower-minute ventilation. 17 Positive pressure ventilation could reduce CPR efficacy by interrupting chest compressions and increasing intrathoracic pressure, thus reducing coronary perfusion. Rescuers who opened the airway first took 30 critical seconds longer to begin chest compressions, during which time there is no coronary perfusion. By changing the sequence to C-A-B, providing chest compressions initially would rapidly restore adequate coronary and cerebral blood flow. The delay in ventilation should be minimal, approximately 18 seconds, the time required to deliver the first cycle of 30 chest compressions. Chest Compression—Push Hard, Push Fast The most important determinant of a successful resuscitation is to provide high-quality chest compressions. To be effective, deliver effective chest compressions on a firm surface. Components of high-quality CPR include the following: • “Push fast”: perform chest compressions at a rate of at least 100 compressions/min. • “Push hard”: for an infant, the chest should be depressed at least one third the anteriorposterior diameter of the chest or approximately 1.5 in (4 cm). For children and adolescents, depress the chest 2 in (5 cm). • Compression landmarks: in infants, the lone rescuer should compress the sternum with 2 fingers, using the index and ring fingers placed just below the intermammary line. 10 Push straight down, assuring that the compressions are smooth, not jerky. Avoid compression over the xiphoid or ribs, which may damage internal organs. When CPR is provided by 2 rescuers, the 2-thumb encircling-hands technique is recommended. Place both the thumbs together over the lower third of the sternum and encircle the infant's chest with both hands, spreading the fingers around the thorax. 10 Forcefully compress the sternum with the thumbs. There is no benefit in squeezing the thorax at the time of chest compression. The 2-thumb encircling-hands technique is preferred over the 2-finger technique because it provides better force of compression and produces higher CPP. 18 In
- 5. PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO • VOL. 12, NO. 4 259 children, compress the lower half of the sternum with the heel of 1 or 2 hands. For adolescents, compress the lower half of the sternum with the heel of 2 hands. The long axis of both heels should be placed parallel with the long axis of the sternum, and rescuers should straighten their arms and lock their elbows, positioning their shoulders over their arms so that body mass is added to the force of the compressions. • Allow complete chest recoil: after each compression, allowing the chest wall to recoil completely permits the heart to refill with blood and improves the blood flow to the body during CPR. Incomplete chest wall recoil during the decompression phase of CPR increases intrathoracic pressure, which decreases venous return and mean arterial pressure and significantly impairs coronary and cerebral perfusion pressures. 19 • Minimize interruptions of chest compressions: for the lone rescuer, a compressionto-ventilation ratio of 30:2 is recommended. After giving 30 compressions, provide 2 breaths and immediately resume compressions, aiming to provide 5 cycles in about 2 minutes. When chest compressions are interrupted, coronary perfusion pressure rapidly declines, which may require several chest compressions to restore adequate coronary pressure once compressions are resumed. Frequent interruptions of chest compressions should be avoided to reduce the duration of low coronary perfusion pressure and flow. • Rotate the compressor role approximately every 2 minutes: during pediatric CPR, rescuer fatigue is common and can lead to inadequate compression rate and depth, with deterioration in quality, even when the rescuer denies feeling fatigued. Because the quality of chest compressions may deteriorate within minutes, rescuers should switch compression and ventilation roles approximately every 5 cycles (about 2 minutes) to prevent compressor fatigue. To minimize interruptions in chest compressions, the switch should be anticipated by the providers and accomplished as quickly as possible, ideally in less than 5 seconds. Airway and Breathing Resuscitation outcomes in infants and children are best if chest compressions are combined with ventilations because of the higher percentage of asphyxial arrests in the pediatric population. During CPR, providers often deliver excessive ventilation particularly when an advanced airway is in place. 20 Excessive ventilation increases intrathoracic pressure and impedes venous return, which decreases cardiac output, cerebral blood flow, and coronary perfusion. 21 For the single rescuer, a compressionto-ventilation ratio of 30:2 is recommended for all ages, which provides more compressions per minute and a higher CPP. For 2-rescuer infant and child CPR, one provider should perform 15 chest compressions, whereas the second rescuer opens the airway with a head tilt–chin lift maneuver and delivers 2 breaths. A compression-to-ventilation ratio of 15:2 provides more ventilations per minute, which is appropriate for most hypoxic, hypercarbic pediatric arrests. One should use the jaw thrust without head tilt to open the airway if there is concern for spinal trauma. If the jaw thrust is unsuccessful in opening the airway, protect the C-spine and carefully use the head tilt–chin lift maneuver because maintaining a patent airway is critical in providing adequate ventilation. Coordinate compressions with ventilations to avoid simultaneous delivery and minimize interruptions in chest compressions. However, if the patient has an ETT in place, deliver at least 100 chest compressions/min continuously without pauses for ventilations. Ventilation is provided by delivering 8 to 10 breaths/min (a breath every 6 to 8 seconds), being careful to avoid excessive ventilation. BVM Ventilation Bag valve mask ventilation is an essential CPR technique for health care providers. In apneic patients and those in respiratory failure, the initial method for ventilation is with a bag mask apparatus, until all the appropriate equipment and personnel for intubation are assembled. For optimum airway alignment, the head should be kept midline, with the auditory meatus in line with the top of the anterior shoulder. The “sniffing” position is achieved, in an older child, by placing a folded towel under the head and elevating it, and infants, by slightly extending the head with a pad under the shoulders. Flexing or overextending the neck may interfere with adequate ventilation by kinking the airway. Provide ventilation using a BVM device with an appropriate size face mask. The proper size mask extends from the bridge of the nose to the cleft of the chin. The minimum volume for a bag in newborns, infants, and small children is 450 to 500 mL, as smaller bags may not deliver an effective tidal volume. 10 In adolescents, an adult bag should be used. If only an adult bag is available, ventilation of infants and children is
- 6. 260 VOL. 12, NO. 4 • PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO possible using a proper size face mask and administering only enough volume to cause the chest to rise. Maintain an oxygen flow of 10 to 15 L/min into a reservoir attached to a pediatric bag and at least 15 L/min in an adult bag. Proper ventilation with a BVM device is achieved in pediatric patients using the E-C clamp technique. 10 Hold the mask snugly to the face with the left thumb and index finger forming a “C.” While avoiding pressure to the eyes, apply downward pressure over the mask to achieve a good seal. The remaining 3 fingers of the left hand form an “E” and are placed on the mandible to lift the jaw, avoiding compression of the soft tissues of the neck. If CPR is being provided, deliver the breaths at the end of each cycle of chest compressions. An oral airway (used in comatose patients with an absent gag reflex) or nasopharyngeal airway (obtunded patients with an intact gag reflex) may help to maintain a patent airway during BVM resuscitation. Because positive pressure ventilation with a BVM causes distention of the stomach, place a nasogastric tube to decompress air from the stomach to minimize the risk of aspiration. Intubation—Cuffed vs Uncuffed ETTs Tracheal intubation is the best way to manage the airway during CPR. Previously, cuffed ETTs were only used in children older than 8 years; however, newer high-volume, low-pressure cuffed tubes may be used in children of all ages (except newborns). 12 The risk of complications in infants and children is similar with cuffed and uncuffed tracheal tubes. 22 Patients in whom high mean airway pressures or poor lung compliance is expected, such as those with status asthmaticus, a cuffed ETT may be preferable to an uncuffed tube, provided cuff inflation pressure is kept less than 20 to 25 cm H2O. 12 To select the correct tracheal tube size for different ages, the following formulas may be used: Uncuffed ETT = 4 plus ½age in years Ä 4Š Cuffed ETT = 3:5 plus ½age in years Ä 4Š . 12 Exhaled CO2 Detector The new PALS guidelines recommend the use of either a colorimetric detector or capnography to confirm tracheal tube placement for neonates, infants, and children with a perfusing cardiac rhythm in all settings (eg, prehospital, ED, and intensive care unit). 12 Immediately after cardiac arrest, CO2 continues to be produced in the body, but there is no CO2 delivery to the lungs. Continuous quantitative waveform capnography is a reliable and rapid bedside method of confirming ETT placement and for ongoing monitoring of ETT placement and is recommended for intubated patients throughout the periarrest period. Measurement of PETCO2 correlates with coronary and cerebral perfusion pressures and is predictive of the outcomes of CPR. 14 It may be used to help guide therapy especially for monitoring cardiac output and the effectiveness of chest compressions during CPR or shock. As with many devices, there are limitations that can affect results and interpretations. Values of PETCO2 decrease for a short time after administration of epinephrine or other vasoconstrictive medications as a result of a reduced pulmonary blood flow. Colorimetric CO2 detector devices are reliable only with a perfusing rhythm. False-positive readings due to contamination with carbonated beverages in the stomach may be minimized by administering 6 ventilations to clear any residual CO2 from the trachea. In very small infants (b2 kg), there may be insufficient volumes of CO2 exhaled to produce a color change. Cricoid Pressure There is insufficient evidence to recommend routine cricoid pressure application to prevent aspiration during endotracheal intubation in children. 23 Cricoid pressure is used to prevent gastric inflation by the application of pressure on the cricoid cartilage sufficient to occlude the esophagus without compressing the airway lumen or moving the cervical spine. However, cricoid pressure can impede the placement of an ETT and does not entirely prevent aspiration. Cricoid pressure may be considered in an unresponsive patient, only if there is a third health care provider available. 12 Oxygen Oxygen delivery has a paradoxical effect on the injured brain. Inadequate oxygenation may potentiate anoxic injury, whereas hyperoxemia after ROSC from cardiac arrest enhances the oxidative injury after ischemia reperfusion. 24 Until additional information becomes available, current guidelines recommend the use of 100% oxygen during resuscitation. Once circulation is restored, ensure adequate arterial oxygen content by titrating oxygen administration to maintain the oxyhemoglobin saturation between 94% and 99% because an oxygen saturation of 100% may correspond to a PaO2 anywhere between 80 and 500 mm Hg. 12 Laryngeal Mask Airway The laryngeal mask airway (LMA) consists of a tube attached to a mask rimmed with a soft
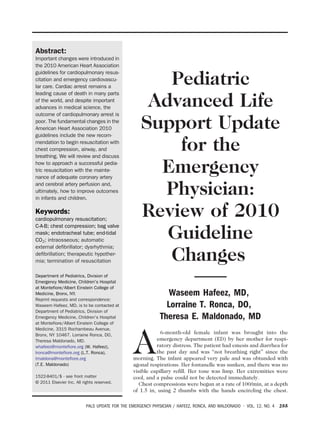
- 7. PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO • VOL. 12, NO. 4 261 inflatable cuff. When properly placed, the LMA rests in the hypopharynx around the glottic opening and directs air into the trachea. It is used in patients with decreased airway reflexes (ie, obtunded or comatose). Unlike a tracheal tube, it will not prevent aspiration of gastric contents into the trachea, making them unsuitable for most emergent situations in infants and children. LMA insertion is associated with a higher incidence of complications in young children compared with older children and adults. 25 There is insufficient evidence to recommend the routine use of an LMA during cardiac arrest in children. The LMA is an acceptable alternative rescue device used by experienced providers when bag mask ventilation and endotracheal intubation are unsuccessful. Rapid Sequence Intubation—Etomidate Contraindicated in Septic Shock Rapid sequence intubation (RSI) involves the sequential injection of preselected sedatives and neuromuscular blocking agents to gain immediate control of the airway. In the critically ill patient with increased intracranial pressure or those who may be hemodynamically unstable or uncooperative, attempting awake tracheal intubation is likely to agitate the patient resulting in worsening symptoms and increasing the risk of vomiting and pulmonary aspiration. The goals of RSI are to create ideal intubating conditions by attenuating airway reflexes and to minimize elevations of intracranial pressure while maintaining adequate blood pressure. The patient is given a short-acting sedative/analgesic (eg, etomidate, thiopental, midazolam, ketamine, fentanyl, or propofol) followed immediately by a short-acting muscle relaxant (eg, succinylcholine or rocuronium). The choice of drug will depend on the clinical situation and individual experience of the provider with these agents. Patients in cardiac arrest or moribund patients rarely require any medications to facilitate intubation. The possibility of an unsuccessful intubation should be anticipated, and preparations for alternate airway management should be arranged before initiation of RSI. Etomidate is a short-acting anesthetic that has minimal hemodynamic effects and decreases intracranial pressure; it is a drug of choice for RSI in most clinical situations in the ED. Etomidate should not be routinely used in pediatric patients with evidence of septic shock because even a single dose causes adrenal suppression, which is associated with a higher mortality rate in children. 26 Vascular Access When IV access is challenging or impossible, such as in cardiac arrest or other emergent situations, do not spend more than 90 seconds attempting peripheral vascular access. The IO approach allows for rapid, safe, and effective access for the administration of medications and fluids and should be attempted immediately while other vascular sites are sought. Intraosseous needle placement is no longer restricted to children younger than 6 years, and currently, various devices are available for all age groups. 12 The primary site for IO insertion is the proximal tibia. The Jamshidi IO needle (Baxter, Deerfield, IL), the Cook IO needle (Cook Medical, Inc, Bloomington, IN), and the newer EZ-IO system, which consists of a small battery-powered driver, are commercially available in sizes for infants, children, and adults. 27 The insertion of EZ-IO needle (Vidacare, Shavano Park, TX) is easier than manually inserted needles because the power drill does the all the work; however, extra precaution is required because it is easy to overshoot the marrow and through the other side. The FAST 1/FAST X (Pying Medical Corporation, British Columbia, Canada) sternal IO infusion system is designed to safely penetrate into the manubrium. Adult and adolescent patients (age, N12 years) have a manubrium thickness deep enough to make the procedure safe. Dysrhythmia Management An approach to pediatric dysrhythmia management is shown in the algorithm (Figure 1) and begins with checking the patient's responsiveness and a rapid pulse check. Unstable signs include altered mental status and abnormal vital signs (temperature, heart rate, blood pressure, respiratory rate, pulse oximeter). All patients require secure vascular access, oxygen therapy, and cardiopulmonary monitoring. The goal of initial management is to restore normal mental status, good oxygenation and perfusion, and adequate urine output. A 12-lead ECG should be obtained to assess the rate, rhythm, absence or presence of P wave, and whether there is a widened QRS complex (N0.09 seconds). Bradycardia Patients with asymptomatic bradycardia have adequate pulses, perfusion, and respirations, and no emergency treatment is necessary. Continue monitoring and proceed with a complete evaluation. In patients with symptomatic bradycardia (heart rate b60 beats/min with cardiovascular compromise), start chest compressions and support airway,
- 8. 262 VOL. 12, NO. 4 • PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO 1. Assess Patient & Check Pulse 2. Calculate Rate 3. Analyze Rhythm: P-wave/QRS PRESENT 4. Treat Patient CHECK PULSE • • • Check Rate ABSENT UNSTABLE SIGNS Altered mental status Hypotension s/s Shock, Resp failure CPR (5 cycles in 2 min) • <8yr: 15 compressions • >8yr: 30 compressions HR >160 bpm HR < 60 bpm • Check ABCs • Start CPR • IV/IO Access • 100% O2 + 2 breaths STABLE UNSTABLE Check Rhythm • Initiate CPR • Epinephrine (1:10,000) 0.1 cc/kg IV q 3-5 min Vagal/Primary AV block: • Atropine (0.02 mg/kg) Min 0.1 mg Max 0.5 mg child 1 mg adolescent • Consider Pacing • Check ABCs • 100% O2 • Monitor • Evaluate Check QRS NARROW QRS ≤ 0.09 PRESENT WIDE QRS > 0.09 VT / VF UNSTABLE ABSENT PEA/EMD ASYSTOLE Check P-wave Epinephrine • IV (1:10,000) 0.1 ml/kg IV q 3-5 min • ETT (1:1,000) 0.1 ml/kg ABNORMAL OR ABSENT NORMAL PROBABLE SINUS TACHYCARDIA • Infant <220 bpm ; child <180 bpm) • Identify and treat cause PROBABLE SVT (infant >220 bpm; child >180 bpm) STABLE: • Check ABCs • Give 100% O2 • IV access • Vagal stimulation (no delay) • Adenosine: rapid push / large IV + 5-10 ml NS flush First dose 0.1 mg/kg IV push (6 mg maximum) repeat dose 0.2 mg/kg IV push (12 mg maximum) • Consider Synchronized Cardioversion UNSTABLE: • Cardioversion 0.5 - 1 J/kg (max: Mono 100, 200, 300, 360 J / Biphasic 100, 200 J) Adapted from AHA 2010 Guidelines • • • • • Identify/Treat Causes: • Pneumothorax • Pericardial Tamponade • pH- Acidosis • Pulmonary Embolism • Poisons – Drug OD Hypoxemia Hypovolemia Hypoglycemia Hypothermia Hypo/hyperkalemia PULSELESS VENTRICULAR TACH - FIBRILLATION • Continue CPR (while defibrillator charges) • Defibrillate X 1@2 J/kg (max 200 J – mono/biphasic) • Defibrillate 4 J/kg (max mono 360 J / biphasic 200 J) • Epinephrine (1:10,000) 0.1 ml/kg IV q 3 - 5 min • Amiodarone 5 mg/kg (max 300 mg) IV bolus → shock 4 J/kg or Lidocaine 1 mg/kg (max 100 mg) IV bolus → shock 4 J/kg • Torsades: Magnesium 25 - 50 mg/kg (2 G max) • Repeat sequence : CPR→ shock 4 J/kg → drug → CPR VENTRICULAR TACHYCARDIA STABLE: • Check ABCs / 100% O2 / IV access • Amiodarone 5 mg/kg (max 150 mg) IV in 20-60 min or Lidocaine 1 mg/kg (max 100 mg) IV bolus UNSTABLE: • Synchronized Cardioversion 0.5 - 2 J/kg (max: Mono 100, 200, 300, 360 J / Biphasic 100, 200 J) Figure 1. Pediatric dysrhythmia algorithm. NO PULSE
- 9. PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO • VOL. 12, NO. 4 263 ventilation, and oxygenation. If bradycardia persists, administer epinephrine 0.01 mg/kg (0.1 mL/kg of 1:10 000 solution). If bradycardia is caused by increased vagal tone or primary atrioventricular conduction block, administer atropine 0.02 mg/kg (minimum dose, 0.1 mg; maximum dose, 0.5 mg in child, 1 mg in adolescent). If the bradycardia is caused by complete heart block or congenital or acquired heart disease, consider emergent transcutaneous pacing. Pacing is typically not useful for bradycardia caused by postarrest hypoxia or ischemic myocardial failure. Narrow-Complex Tachycardia (QRS ≤0.09 Seconds) Patients with supraventricular tachycardia without hemodynamic compromise may respond to vagal stimulation. In infants and young children, apply ice to the face without pressure to the eyes or occluding the airway. Older children may perform a Valsalva maneuver by bearing down forcefully or blowing through an occluded straw. If ineffective, attempt pharmacologic cardioversion with adenosine (0.1 mg/kg; maximum dose, 6 mg) using the 2-syringe technique; give adenosine rapidly with 1 syringe and immediately flush with 5 to 10 mL of normal saline with another syringe attached to a stopcock. If necessary, adenosine may be repeated at a dose of 0.2 mg/kg (maximum dose, 12 mg). Verapamil (0.1-0.3 mg/kg) may be used as a secondline therapy, with pediatric cardiology consultation. Use of verapamil in infants is not recommended because it may cause myocardial depression, hypotension, and potential cardiac arrest. Wide-Complex Tachycardia (QRS N0.09 Seconds) QRS duration varies with age and is considered prolonged if it is more than 90 milliseconds (0.09 second) for a child younger than 4 years and 100 milliseconds or more (0.1 second) for a child between the ages of 4 and 16 years. 28 The current PALS guideline defines a QRS width more than 0.09 second as prolonged for the pediatric patient, a change of 0.01 second from previous recommendations, which can only be detected by computer interpretation of the ECG rhythm strip. 12 Ventricular tachycardia may be monomorphic (identical QRS complexes originating from a single focus) or polymorphic (torsade de pointes—irregular rhythm, varying QRS waveform). Ventricular fibrillation is a pulseless, grossly disorganized, rapid ventricular rhythm that varies in interval and morphology and may be difficult to distinguish from rapid, polymorphic VT. The ED treatment of acute VT depends on the clinical state of the patient. Stable patients with monomorphic VT and normal perfusion may be treated with either amiodarone (5 mg/kg IV for 20-60 minutes) or procainamide (15 mg/kg IV for 30-60 minutes), although not simultaneously because both will prolong the QT interval. 12 One must monitor the ECG and blood pressure because these drugs may cause widening of the QRS complex and hypotension. If the patient does not respond or becomes hemodynamically unstable, synchronized cardioversion is recommended using an initial dose of 0.5 to 1 J/kg, increasing to 2 J/kg, if necessary. At times, it may be difficult to differentiate supraventricular tachycardia with aberrant conduction from VT. In such cases, adenosine may be used, provided there are monomorphic QRS complexes with a regular rhythm. Avoid using adenosine in patients known to have WolffParkinson-White syndrome who present with a wide-complex tachycardia. Pulseless VT and polymorphic VT are treated similar to VF with high-energy unsynchronized shocks (defibrillation). Survival is better in primary than in secondary VF, and the probability of survival declines by 7% to 10% for each minute of arrest without CPR and defibrillation. 29 In such patients, begin high-quality CPR and deliver a single defibrillation dose of 2 J/kg, immediately resuming chest compressions for about 2 minutes. On the next rhythm check, if VF persists, give a second shock at 4 J/kg. If subsequent rhythm checks reveal VF, administer epinephrine 0.01 mg/kg (0.1 mL/kg of 1:10 000 solution) followed by defibrillation at 4 J/kg. Other medications used to treat VF/VT include amiodarone (5 mg/kg IV bolus) or lidocaine (1 mg/kg), and for torsades de pointes, magnesium sulfate (25-50 mg/kg) is indicated. 12 The goal is to provide continuous CPR with minimal interruptions between shock deliveries. The resuscitation sequence should be as follows: CPR (stop only to deliver shock) Y defibrillation (2 J/kg) Y CPR Y defibrillation (4 J/kg) Y medication Y CPR Y defibrillation (4 J/kg). In prior AHA guidelines, 3 stacked shocks were delivered based on the low first shock efficacy of monophasic defibrillators and also to decrease transthoracic impedance. Current biphasic defibrillators have a high first shock efficacy. With these devices, if one shock fails to eliminate VF, the incremental benefit of another immediate shock is low. Resumption of CPR is likely to provide improved coronary perfusion, which increases the likelihood of a successful defibrillation with the delivery of a subsequent shock. Another disadvantage of a
- 10. 264 VOL. 12, NO. 4 • PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO 3-shock sequence was the delay of 29 to 37 seconds between delivery of the first shock and the beginning of the first postshock chest compression, the period during which there is no coronary perfusion. Automatic External Defibrillator Automated external defibrillators may be used for children and adults with witnessed sudden arrest who have no signs of circulation. 12 An AED can accurately detect VF in children and can differentiate “shockable” from “nonshockable” rhythms with a high degree of sensitivity and specificity. 30 Neither the lowest-energy dose for effective defibrillation nor the upper limit for safe defibrillation is known in pediatric patients. Automatic external defibrillators that deliver relatively high-energy doses have been successfully used in infants in cardiac arrest with no clear adverse effects and achieved good neurologic outcomes. In infants and children 1 to 8 years old (weight, 10-25 kg; length, b50 in), use an AED with a pediatric attenuator system, which decreases the delivered energy to a dose suitable for children. In infants younger than 1 year, a manual defibrillator is preferred. 12 The recommended first energy dose for defibrillation is 2 J/kg, and if a second dose is required, it should be doubled to 4 J/kg. If a manual defibrillator is not available, an AED with a dose attenuator may be used in infants. Pulseless Arrest—Asystole/PEA The treatment of asystole and PEA is to provide high-quality chest compression and adequate ventilation and to maintain perfusion to vital organs. Administer epinephrine 0.01 mg/kg IV/IO (0.1 ml/kg of 1:10 000 solution), or if there is no vascular access, administer ETT at 0.1 mg/kg (0.1 ml/kg of 1:1000 solution). The epinephrine dose can be repeated every 3 to 5 minutes. There is no role in PALS for the routine use of high-dose epinephrine, atropine, calcium, or vasopressin in asystole. 12 During resuscitation, it is vital to identify and treat the reversible cause of arrest: the 5 Hs (hypoxemia, hypovolemia, hypothermia, hypoglycemia, hypokalemia/hyperkalemia) and the 5 Ps (pneumothorax, pericardial tamponade, pH—severe acidosis, pulmonary embolism, poisons—drug overdose). 12 Therapeutic Hypothermia Cardiac arrest commonly contributes to the brain injury caused by hypoxia and global ischemia. Multiple mechanisms are involved in neuronal damage, both by hypoxia-induced encephalopathy and by reperfusion-induced cellular and tissue injury. The neuroprotective role of hypothermia is achieved by multiple mechanisms. It reduces the metabolic oxygen utilization in the brain, decreasing cerebral electrical activity and minimizing free radical formation, which is associated with reperfusion injury. The AHA has recommended the use of induced hypothermia in comatose adult patients with ROSC after out-of-hospital VF cardiac arrest. 12 Based on existing randomized controlled trials in adults and newborns, the AHA recommends that hypothermia therapy may be considered in children who remain comatose after resuscitation from cardiac arrest. 31 The ideal method and duration of cooling and rewarming are not known. Cooling should be initiated within 6 hours after ROSC, with a hypothermia target of 32°C to 34°C (89.6°F to 93.2°F) for 12 to 24 hours. 12 Although there are multiple methods for inducing hypothermia, no single method has proved to be optimal. Termination of Resuscitation Currently, there are no reliable predictors of outcome during resuscitation to guide when to terminate in-hospital resuscitation efforts. Bystander CPR for witnessed collapse and a short interval from collapse to arrival of EMS improves the chances of survival. Children with prolonged resuscitation efforts without ROSC after 2 doses of epinephrine were considered unlikely to survive; however, intact survival after an unusually prolonged in-hospital resuscitation has been documented in children with VF or VT, drug toxicity, and primary hypothermic insult. 32 CONCLUSION Successful resuscitation requires a well-organized team approach, with each member knowing his or her preassigned responsibilities. 33 Pediatric-sized equipment and precalculated weight-based medication dosing devices or the Broselow tape must be available and organized for easy access. It is imperative that the staff have training in PALS and routinely practice mock pediatric resuscitations in their unit. The most important determinant of successful resuscitation is the maintenance of adequate coronary artery and cerebral artery perfusion. These can be achieved by implementing the new guidelines of the AHA, by beginning resuscitation with C-A-B. Resuscitation outcomes in infants and children can be improved by providing high-quality chest compressions combined with effective ventilations.
- 11. PALS UPDATE FOR THE EMERGENCY PHYSICIAN / HAFEEZ, RONCA, AND MALDONADO • VOL. 12, NO. 4 265 REFERENCES 1. Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA 1960;173:1064-7. 2. Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 2006;295: 50-7. 3. Meaney PA, Nadkarni VM, Kern KB, et al. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med 2010;38:101-8. 4. Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry–Cardiac Arrest. Circulation 2009;119:1484-91. 5. Lopez-Herce J, Garcia C, Rodriguez-Nunez A, et al. Longterm outcome of paediatric cardiorespiratory arrest in Spain. Resuscitation 2005;64:79-85. 6. Mogayzel C, Quan L, Graves JR, et al. Out-of-hospital ventricular fibrillation in children and adolescents: causes and outcomes. Ann Emerg Med 1995;25:484-91. 7. Kitamura T, Iwami T, Kawamura T, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet 2010;375:1347-54. 8. Xu JQ, Kochanek KD, Murphy SL, et al. Deaths: final data for 2007. National vital statistics reports; vol 58 no 19. Hyattsville, MD: National Center for Health Statistics; 2010. 9. Crewdson K, Lockey D, Davies G. Outcome from paediatric cardiac arrest associated with trauma. Resuscitation 2007; 75:29-34. 10. Berg MD, Schexnayder SM, Chameides L, et al. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care science. Part 13: pediatric basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122: S862-75. 11. Tibballs J, Russell P. Reliability of pulse palpation by healthcare personnel to diagnose paediatric cardiac arrest. Resuscitation 2009;80:61-4. 12. Kleinman ME, Chameides L, Schexnayder SM, et al. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care science. Part 14: pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122:S876-908. 13. Paradis NA, Martin GB, Rivers EP, et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 1990;263: 1106-13. 14. Kolar M, Krizmaric M, Klemen P, et al. Partial pressure of endtidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study. Crit Care 2008;12:1-13. 15. Smith KK, Gilcreast D, Pierce K. Evaluation of staff's retention of ACLS and BLS skills. Resuscitation 2008;78:59-65. 16. Paradis NA, Martin GB, Goetting MG, et al. Simultaneous aortic, jugular bulb, and right atrial pressures during 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. cardiopulmonary resuscitation in humans: insights into mechanisms. Circulation 1989;80:361-8. Baskett P, Nolan J, Parr M. Tidal volumes which are perceived to be adequate for resuscitation. Resuscitation 1996;31:231-4. Menegazzi JJ, Auble TE, Nicklas KA, et al. Two-thumb versus two-finger chest compression during CPR in a swine infant model of cardiac arrest. Ann Emerg Med 1993;22:240-3. Yannopoulos D, McKnite S, Aufderheide TP, et al. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation 2005;64:363-72. Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA 2005;293:305-10. Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation 2004;109:1960-5. Newth CJ, Rachman B, Patel N, et al. The use of cuffed versus uncuffed endotracheal tubes in pediatric intensive care. J Pediatr 2004;144:333-7. Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: a riskbenefit analysis. Ann Emerg Med 2007;50:653-65. Kilgannon JH, Jones AE, Shapiro NI, et al, for the Emergency Medicine Shock Research Network (EMShockNet) Investigators. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 2010;303:2165-71. Harnett M, Kinirons B, Heffernan A, et al. Airway complications in infants: comparison of laryngeal mask airway and the facemask-oral airway. Can J Anaesth 2000;47:315-8. den Brinker M, Hokken-Koelega AC, Hazelzet JA, et al. One single dose of etomidate negatively influences adrenocortical performance for at least 24 h in children with meningococcal sepsis. Intens Care Med 2008;34:163-8. Tay ET, Hafeez W. Intraosseous access. E-Med J, Available at: http://www.emedicine.com/proc/topic80431.htm. Accessed 7-5-2011. Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram. Part III: intraventricular conduction disturbances. Circulation 2009;119:e235-40. Larsen MP, Eisenberg MS, Cummins RO, et al. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med 1993;22:1652-8. Samson RA, Berg RA, Bingham R, et al. Use of automated external defibrillators for children: an update. An advisory statement from the pediatric advanced life support task force, International Liaison Committee on Resuscitation. Circulation 2003;107:3250-5. Fink EL, Clark RS, Kochanek PM, et al. A tertiary care center's experience with therapeutic hypothermia after pediatric cardiac arrest. Pediatr Crit Care Med 2010;11:66-74. Young KD, Gausche-Hill M, McClung CD, et al. A prospective, population-based study of the epidemiology and outcome of out-of hospital pediatric cardiopulmonary arrest. Pediatrics 2004;114:157-64. Hafeez W. Resuscitation. In: Crain EF, Gershel JC, editors. Clinical manual of emergency pediatrics, 5th ed. New York, NY: Cambridge University Press 2009. p. 1-29.