Parathyroid disorders.pdf
- 1. PRESENTATION ON MANAGEMENT OF PATIENTWITH PARATHYROID DISORDERS MRS. JISHA SRIVASTAVA 1
- 2. OBJECTIVES 2 After the class the students will be able Explain the structures and function of Parathyroid gland. Explain the age affect on parathyroid gland. Describe the definition, etiology, risk factors, pathophysiology, medical management, surgical management and Nursing management of Hyperparathyroidism. Describe the definition, etiology, risk factors, pathophysiology, medical management, surgical management and Nursing management of Hypothyroidism. List down the health education for Hyperparathyroidism and Hypoparathyroidism.
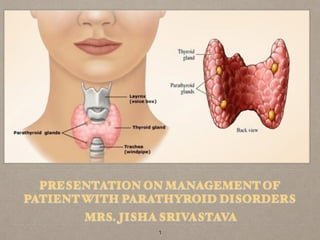
- 3. ANATOMY AND PHYSIOLOGY OF PARATHYROID GLAND
- 4. ANATOMY AND PHYSIOLOGY OF PARATHYROID GLANDS Four parathyroid glands, two on the back of each lobe of the thyroid gland. The hormone they produce is called parathyroid hormone (PTH), which is an antagonist to calcitonin; it maintains normal blood levels of calcium and phosphate. Target organs of PTH are bone, small intestine and kidneys. PTH increases the resorption of calcium and phosphate from the bones to the blood, which raises their blood levels. Absorption of calcium and phosphate from food in the small intestine is also increased by PTH through its action of activating vitamin D (calcitriol) in the kidneys. PTH also increases the resorption of calcium by the kidneys and the excretion of phosphate (more than is obtained from bones). 4
- 5. ANATOMY AND PHYSIOLOGY OF PARATHYROID GLANDS Overall effect of PTH is to raise the blood calcium level and lower the blood phosphate level. Secretion of PTH is stimulated by hypocalcemia (a low blood calcium level) and is inhibited by hypercalcemia. PTH is probably the most important regulator of the blood calcium level. Calcium ions in the blood are essential for normal excitability of neurons and muscle cells and for the process of blood clotting. 5
- 6. FUNCTION OF THE PARATHYROID GLANDS Parathyroid glands produce parathyroid hormone, which plays a key role in the regulation of calcium levels in the blood. Precise calcium levels are important in the human body, since small changes can cause muscle and nerve problems. Release of calcium by bones into the bloodstream Absorption of calcium from food by the intestines Conservation of calcium by the kidneys Stimulates cells in the kidney to transforms weaker forms of vitamin D into the form that is strongest at absorbing calcium from the intestines 6
- 8. DEFINITION Hyperparathyroidism (HPT) is the most common type of parathyroid disease. In HPT, one or more glands are overactive. As a result, the glands make too much PTH. This may result in too much calcium in the blood—a condition called hypercalcemia. Hyperparathyroidism, a disorder caused by overactivity of one or more of the parathyroid glands, is classified as primary, secondary, or tertiary. 8
- 9. INCIDENCE Primary hyperparathyroidism occurs two to four times more often in women than in men and is most common in patients between 60 and 70 years of age. About 100,000 new cases of hyperparathyroidism are detected each year in the United States. The disease is rare in children younger than 15 years, but the incidence increases tenfold between the ages of 15 and 65 years. 9
- 10. INCIDENCE It usually occurs in clients older than 60 and affects women twice as often as men, and clients with renal failure. The overall incidence of hyperparathyroidism is 27 per 100.000. Half of the patients diagnosed with hyperparathyroidism do not have symptoms. Secondary hyperparathyroidism, with manifestations similar to those of primary hyperparathyroidism, occurs in patients with chronic renal failure and so called renal rickets as a result of phosphorus retention, increased stimulation of the parathyroid glands, and increased parathyroid hormone secretion 10
- 11. Adenoma or Hyperplasia or a benign tumor of the parathyroid glands. Hereditary. Some cancers can also make a substance that mimics PTH and causes hypercalcemia. Serum calcium may be reduced in kidney disease because of the kidneys’ failure to activate vitamin D 11 ETIOLOGY
- 12. Primary hyperparathyroidism develops when the normal regulatory relationship between serum calcium levels and parathyroid hormone (PTH) secretion is interrupted. 12 CLASSIFICATION
- 13. Secondary hyperparathyroidism occurs when the glands are hyperplastic because of malfunction of another organ system. It is usually the result of renal failure and cancers such as multiple myeloma, Or carcinoma with bone metastasis. Tertiary hyperparathyroidism occurs when PTH production is irresponsible(autonomous) in clients with normal or low Serum calcium levels 13 CLASSIFICATION
- 14. The normal function of TH is to increase bone resorption, thereby maintaining the proper balance of calcium and phosphorus the blood. Excessive circulating PTH leads to bone damage, hypercalcemia, and kidney damage. 14 PATHOPHYSIOLOGY
- 15. Primary Hyperparathyroidism : The severity of hypercalcemia reflects the quantity of hyper functioning parathyroid tissue. Excessive PTH stimulates transport or calcium into the blood from the intestine, kidneys, and bone. Nephrolithiasis is secondary to calcium phosphate kidney stones and deposition of calcium in the soft tissues of the kidney. Pyelonephritis may complicate the nephrolithiasis. Bone resorption related to hypercalcemia may develop. 15 PATHOPHYSIOLOGY
- 16. Secondary Hyperparathyroidism: Chronic renal failure and hyperphosphatemia cause secondary hyperparathyroidism. As the glomerular filtration rate (GFR) decreases in chronic renal failure, serum phosphorus levels rise, which causes the serum calcium level to fall. PTH secretion is stimulated. This increase decreases renal tubular absorption of phosphorus, causing serum phosphorus levels to return to normal. As the GFR continues to decrease, PTH is secreted in increased amounts to decrease tubular reabsorption of phosphorus and maintain serum phosphorus level at or close to normal limits. 16 PATHOPHYSIOLOGY
- 17. Apathy, fatigue, muscle weakness, nausea, vomiting, constipation, hypertension, and cardiac dysrhythmias may occur; all are attributable to the increased concentration of calcium in the blood. Psychological manifestations may vary from irritability and neurosis to psychoses caused by the direct effect of calcium on the brain and nervous system. An increase in calcium produces a decrease in the excitation potential of nerve and muscle tissue. 17 CLINICAL MANIFESTATIONS
- 19. The formation of stones in one or both kidneys, related to the increased urinary excretion of calcium and phosphorus Renal damage results from the precipitation of calcium phosphate in the renal pelvis and parenchyma, resulting in renal calculi (kidney stones), obstruction, pyelonephritis, and renal failure. 19 CLINICAL MANIFESTATIONS
- 20. Musculoskeletal symptoms accompanying hyperparathyroidism may result from demineralization of the bones or bone tumors composed of benign giant cells resulting from overgrowth of osteoclasts. The patient may develop skeletal pain and tender- ness, especially of the back and joints; pain on weight bearing; pathologic fractures; deformities; and shortening of body stature. 20 CLINICAL MANIFESTATIONS
- 21. Bone loss attributable to hyperparathyroidism increases the risk for fracture. The incidence of peptic ulcer and pancreatitis is increased with hyperparathyroidism and may be responsible for many of the gastrointestinal symptoms that occur. Hypercalcemia can cause serious problems, including: osteoporosis, kidney stones, heart disease, high blood pressure 21 CLINICAL MANIFESTATIONS
- 22. Most people with primary HPT have no symptoms. Some people experience mild symptoms, such as: muscle weakness, fatigue, increased need for sleep, depression, aches and pains in the joints and bones Symptoms for people with more severe disease may include: loss of appetite, nausea, vomiting, constipation, confusion or impaired thinking and memory, increased thirst and urination 22 CLINICAL MANIFESTATIONS
- 23. In rare cases, two or more of the glands are overactive. This is called hyperplasia. HPT is most often diagnosed in people between the ages of 50 and 60. Women are affected about three times as often as men. Some people have HPT due to a rare genetic disorder called familial hypocalciuric hypercalcemia. This condition is typically benign and does not require treatment. kidney failure causes the parathyroid glands to become overactive. This is called secondary HPT. 23 CLINICAL MANIFESTATIONS
- 24. Primary hyperparathyroidism is diagnosed by persistent elevation of serum calcium levels and an elevated level of parathormone. Radioimmunoassays for parathormone are sensitive and differentiate primary 24 DIAGNOSTIC FINDINGS S. N O TEST NORMA L VALUES FINDINGS 1 Parathyroid hormone 25 pg/mL ↑ in primary hyperparathyroidism ↓ in primary hypoparathyroidism, parathyroid trauma during thyroid surgery ↑ in some cancers, hyperparathyroidism ↓ in hypothyroidism ↑ in hypoparathyroidism ↓ in hyperparathyroidism 2 Calcium 8.5–10.5 mg/dL 3 Phosphorus 2 . 4 – 4 . 7 mg/dL
- 25. An elevated serum calcium level alone is a nonspecific finding because serum levels may be altered by diet, medications, and renal and bone changes. Bone changes may be detected on x-ray or bone scans in advanced disease. The double antibody parathyroid hormone test is used to distinguish between primary hyperparathyroidism and malignancy as a cause of hypercalcemia. 25 DIAGNOSTIC FINDINGS
- 26. Ultrasound, MRI, thallium scan, and fine-needle biopsy have been used to evaluate the function of the parathyroids and to localize parathyroid cysts, adenomas, or hyperplasia. Bone densitometry (DEXA, DXA): Bone densitometry, also called DEXA or DXA, uses a very small dose of ionizing radiation to produce pictures of the inside of the body (usually the lower spine and hips) to measure bone loss. DXA is simple, quick and noninvasive. 26 DIAGNOSTIC FINDINGS
- 27. Ultrasound: Ultrasound imaging uses sound waves to produce pictures of the inside of the body. Ultrasound is safe, noninvasive, and does not use radiation. Computed tomography (CT) - body: CT scans use a combination of x rays and computer technology to create three-dimensional (3-D) images. A CT scan may include the injection of contrast material. 27 DIAGNOSTIC FINDINGS
- 28. HYPERCALCEMIC CRISIS Acute hypercalcemic crisis can occur with extreme elevation of serum calcium levels. Serum calcium levels higher than 15 mg/dL (3.7 mmol/L) result in neurologic, cardiovascular, and renal symptoms that can be life-threatening. 28 COMPLICATIONS
- 29. HYPERCALCEMIC CRISIS Treatment includes rehydration with large volumes of intravenous fluids, diuretic agents to promote renal excretion of excess calcium, and phosphate therapy to correct hypophosphatemia and decrease serum cal- cium levels by promoting calcium deposit in bone and reducing the gastrointestinal absorption of calcium. Cytotoxic agents (mithramycin), calcitonin, and dialysis may be used in emergency situations to decrease serum calcium levels quickly . 29 COMPLICATIONS
- 30. HYPERCALCEMIC CRISIS The patient requires expert assessment and care to minimize complications and reverse the life-threatening hypercalcemia. Medications are administered with care, and attention is given to fluid balance to promote return of normal fluid and electrolyte bal- ance. Supportive measures are necessary for the patient and family. 30 COMPLICATIONS
- 31. The recommended treatment of primary hyperparathyroidism is the surgical removal of abnormal parathyroid tissue. In some patients without symptoms and with only mildly elevated serum calcium levels and normal renal function, surgery may be delayed and the patient followed closely for worsening of hypercalcemia, bone deterioration, renal impairment, or the development of kidney stones. 31 MEDICAL MANAGEMENT
- 32. Lowering severely elevated calcium levels and long- term management of hypercalcemia with drugs to increase bone resorption of calcium. Serum calcium levels are lowered by hydration and calciuria. Hydration can be achieved with an infusion of normal saline solution. Normal saline is the fluid of choice because it both expands the volume and acts in the kidney to inhibit the resorption of calcium. 32 MEDICAL MANAGEMENT
- 33. Furosemide (Lasix), a loop diuretic, may also be used to promote calciuria after rehydration has occurred.. A client with hypercalcemia should have a diet low in calcium and vitamin D. Drugs that inhibit bone resorption include plicamycin (Mithracin), gallium nitrate (Ganite), phosphates, and calcitonin. Plicamycin is a chemotherapeutic drug that is effective in lowering serum calcium levels. MEDICAL MANAGEMENT
- 34. The hypocalcemic effect occurs after 24 hours and lasts about 1 to 2 weeks. Gallium nitrate, a newer drug, is now being used more often because it has even fewer side effects. Glucocorticoids may be used to reduce hypercalcemia by decreasing the gastrointestinal absorption of calcium. Etidronate (Didronel) or calcitonin can be used to decrease the release of calcium by bones. 34 MEDICAL MANAGEMENT
- 35. Parathyroidectomy :Definitive treatment of primary hyperparathyroidism is surgical removal of the gland or glands causing hyper secretion of PTH. Intraoperative, rapid parathyroid hormone assay measurement affords the ability to ensure removal of all hyper functioning parathyroid tissue. Autotransplantation of the parathyroid glands is a useful modality for the management of certain forms of hyperparathyroidism and radical neck surgery. 35 SURGICAL MANAGEMENT
- 36. After partial parathyroidectomy, it is possible to transplant the remaining healthy parathyroid tissue to a safer location, such as the brachioradial muscle of the forearm. Re-exploration of the neck in the future may cause laryngeal nerve damage and influence complications of the original surgery. 36 SURGICAL MANAGEMENT
- 37. Transplantation procedures take some time to come to full effect. In the meantime, he client must supplement the diet with calcium and vitamin D to prevent hypoparathyroidism and hypocalcemia. If hyperparathyroidism is surgically treated early in its Course, the chance of total recovery is good. Bone pain may disappear within 3 days after removal of parathyroid tissue, and bone lesions may heal completely. unfortunately, serious renal disease might not be reversible by parathyroid surgery. 37 SURGICAL MANAGEMENT
- 38. Complications after parathyroidectomy are similar to those following thyroidectomy and rarely Occur. Hypocalcemia is a potentially life-threatening complication even if some parathyroid glands are left untouched because edema reduces their function. The client may also experience respiratory distress related to either to hemorrhage or to recurrent laryngeal nerve damage. The cure rate for primary hyperparathyroidism after surgical removal is greater than 95%. 38 SURGICAL MANAGEMENT
- 39. The nursing management of the patient undergoing parathyroidectomy is essentially the same as that of a patient undergoing thyroidectomy. However, the previously described precautions about dehydration, immobility, and diet are particularly important in the patient awaiting and recovering from parathyroidectomy. Although not all parathyroid tissue is removed during surgery in an effort to control the calcium–phosphorus balance, the nurse closely monitors the patient to detect symptoms of tetany (which may be an early postoperative complication). Most patients quickly regain function of the remaining parathyroid tis- sue and experience only mild, transient postoperative hypocalcemia. 39 NURSING MANAGEMENT
- 40. Nursing Interventions Monitor BP lying, sitting, and standing, if able. Note widened pulse pressure. Monitor central venous pressure (CVP), if available. Investigate reports of chest pain or angina. Assess pulse and heart rate while patient is sleeping. Auscultate heart sounds, note extra heart sounds, development of gallops and systolic murmurs. Monitor ECG, noting rate and rhythm. Document dysrhythmias. Auscultate breath sounds. Note adventitious sounds. Monitor temperature; provide cool environment, limit bed linens or clothes, administer tepid sponge baths. 40 RISK FOR DECREASED CARDIAC OUTPUT RELATED TO DYSRHYTHMIAS DUE TO INCREASED CALCIUM LEVEL IN THE BLOOD
- 41. Nursing Interventions Observe signs and symptoms of severe thirst, dry mucous membranes, weak or thready pulse, poor capillary refill, decreased urinary output, and hypotension. Record I&O. Note urine specific gravity. Weigh daily. Encourage chair rest or bedrest. Limit unnecessary activities. Note history of asthma and bronchoconstrictive disease, sinus bradycardia and heart blocks, advanced HF, or current pregnancy. Observe for adverse side effects of adrenergic antagonists: severe decrease in pulse, BP; signs of vascular congestion/HF; cardiac arrest. Administer IV fluids as indicated. Administer medications as indicated: Thyroid hormone antagonists: propylthiouracil (PTU), methimazole (Tapazole) [beta]-blockers: propranolol (Inderal), atenolol (Tenormin), nadolol (Corgard), pindolol (Visken) 41 RISK FOR DECREASED CARDIAC OUTPUT RELATED TO DYSRHYTHMIAS DUE TO INCREASED CALCIUM LEVEL IN THE BLOOD
- 42. Monitor vital signs, noting pulse rate at rest and when active. Note development of tachypnea, dyspnea, pallor, and cyanosis. Provide for a quiet environment; cool room, decreased sensory stimuli, soothing colors, quiet music. Encourage patient to restrict activity and rest in bed as much as possible. Provide comfort measures: touch therapy or massage, cool showers. Patient with dyspnea will be most comfortable sitting in high Fowler’s position. Provide for diversional activities that are calming, e.g., reading, radio, television. 42 FATIGUE RELATED TO DISEASE CONDITION AS EVIDENCED BY VERBALISATION OF OVERWHELMING LACK OF ENERGY TO MAINTAIN THE USUAL ROUTINE, DECREASED PERFORMANCE.
- 43. Nursing Interventions Assess the thinking process. Determine attention span, orientation to place, person, or time. Note changes in behavior. Assess the level of anxiety. Provide a quiet environment; decreased stimuli, cool room, dim lights. Limit procedures and/or personnel. Reorient to person, place, or time as indicated. Present reality concisely and briefly without challenging illogical thinking. Provide clock, calendar, room with outside window; alter the level of lighting to simulate day or night. 43 RISK FOR DISTURBED THOUGHT PROCESSES RELATED TO PHYSIOLOGICAL CHANGES: INCREASED CNS STIMULATION/ACCELERATED MENTAL ACTIVITY
- 44. Nursing Interventions Monitor daily food intake. Weigh daily and report losses. Encourage patient to eat and increase the number of meals and snacks. Give or suggest high-calorie foods that are easily digested. Provide a balanced diet, with six meals per day. Avoid foods that increase peristalsis and fluids that cause diarrhea. Consult with a dietitian to provide a diet high in calories, protein, carbohydrates, and vitamins. Administer medications as indicated: glucose, vitamin B complex, insulin (small doses). 44 RISK FOR IMBALANCED NUTRITION: LESS THAN BODY REQUIREMENTS RELATED NAUSEA/ VOMITING.
- 45. Nursing Interventions Observe behavior indicative of the level of anxiety. Monitor physical responses, noting palpitations, repetitive movements, hyperventilation, insomnia. Stay with the patient, maintaining a calm manner. Acknowledge fear and allow the patient’s behavior to belong to the patient. Describe and explain procedures, surrounding environment, or sounds that may be heard by the patient. Speak in brief statements. Use simple words. Reduce external stimuli: Place in a quiet room; provide soft, soothing music; reduce bright lights; reduce the number of persons having contact with the patient. Discuss with patient and/or SO reasons for emotional lability and/or psychotic reaction. Reinforce the expectation that emotional control should return as drug therapy progresses. Administer antianxiety agents or sedatives and monitor effects. Refer to support systems as needed: counseling, social services, pastoral care. 45 ANXIETY RELATED TO PHYSIOLOGICAL FACTORS: HYPER METABOLIC STATE AS EVIDENCED BY INCREASED FEELINGS OF APPREHENSION, SHAKINESS, LOSS OF CONTROL
- 46. Nursing Interventions Review the disease process and future expectations. Provide information appropriate to individual situation. Identify stressors and discuss precipitators to thyroid crises: personal or social and job concerns, infection, pregnancy. Provide information about signs and symptoms of hypothyroidism and the need for continuous follow- up care. 46 DEFICIENT KNOWLEDGE RELATED TO LACK OF EXPOSURE/RECALL AS EVIDENCED BY QUESTIONS, REQUEST FOR INFORMATION
- 49. DEFINITION Hypoparathyroidism is an uncommon condition in which your body produces abnormally low levels of parathyroid hormone (PTH). PTH is key to regulating and maintaining a balance of two minerals in your body calcium and phosphorus. 49
- 50. INCIDENCE Hypoparathyroidism is diagnosed in women more often than men. The incidence is related to thyroid surgery. The incidence of temporary hypoparathyroidism after total thyroidectomy ranges from 6.9% to 25%. The incidence after subtotal thyroidectomy is 1.6% to 9%. 50
- 51. ETIOLOGY Iatrogenic (treatment-induced) or idiopathic (without a specific cause). 51
- 52. ETIOLOGY Iatrogenic causes include accidental removal of the parathyroid glands during thyroidectomy. Infarction of the parathyroid glands because of an inadequate blood supply to the glands during surgery Strangulation of one or more of the glands by postoperative scar tissue. Health maintenance actions include monitoring of PTH, calcium, and phosphorus levels. 52
- 53. ETIOLOGY Calcium supplements are required for life to prevent tetany. In rare occurrences idiopathic hypoparathyroidism may exist. Like Graves' disease and Hashimoto's disease, it may be an autoimmune disorder with a genetic basis. Pseudohypoparathyroidism (Albright's hereditary osteodystrophy) is an inherited form of hypoparathyroidism that involves a lack of end-organ responsiveness to PTH. 53
- 54. ETIOLOGY Neck surgery. Autoimmune disease. Hereditary hypoparathyroidism. Low levels of magnesium in your blood. Normal magnesium levels are required for normal production of parathyroid hormone. Extensive cancer radiation treatment of face or neck. 54
- 55. PATHOPHYSIOLOGY PTH acts to increase bone resorption, which maintains proper serum calcium levels. PTH also regulates phosphate clearance by the renal tubules, thereby maintaining the correct inverse balance between serum calcium and serum phosphate levels. Consequently when parathyroid secretion is reduced, bone resorption slows, serum calcium levels fall, and severe neuromuscular irritability develops. 55
- 56. PATHOPHYSIOLOGY Calcifications form in various organs, Such as the eyes and basal ganglia. Without sufficient PTH, fewer phosphorus ions are secreted by the distal tubules of the kidney, renal excretion of phosphate falls, and serum phosphate levels rise. The client may fully recover from the effects of hypoparathyroidism if the conditions diagnosed early, before serious complications begin. Unfortunately, cataracts and brain calcification, once formed, are irreversible. 56
- 57. PATHOPHYSIOLOGY Symptoms of hypoparathyroidism are caused by a deficiency of parathormone that results in elevated blood phosphate (hyperphosphatemia) and decreased blood calcium (hypocalcemia) levels. In the absence of parathormone, there is decreased intestinal absorption of dietary calcium and decreased resorption of calcium from bone and through the renal tubules. Decreased renal excretion of phosphate causes hypophosphaturia, and low serum calcium levels result in hypocalciuria. Muscular hyper irritability Uncontrolled spasm, Hypo calcemic Tetany. 57
- 58. CLINICAL MANIFESTATIONS Hypocalcemia causes irritability of the neuromuscular system and contributes to the chief symptom of hypoparathyroidism—tetany. Tetany is a general muscle hypertonia, with tremor and spasmodic or uncoordinated contractions occurring with or without efforts to make voluntary movements. Symptoms of latent tetany are numbness, tingling, and cramps in the extremities, and the patient complains of stiffness in the hands and feet. 58
- 59. CLINICAL MANIFESTATIONS In overt tetany, the signs include bronchospasm, laryngeal spasm, carpopedal spasm (flexion of the elbows and wrists and extension of the carpophalangeal joints), dysphagia, photophobia, cardiac dysrhythmias, and seizures. Other symptoms include anxiety, irritability, depression, and even delirium. ECG changes and hypotension also may occur. Tingling or burning in your fingertips, toes and lips. 59
- 60. CLINICAL MANIFESTATIONS Twitching or spasms of your muscles, particularly around your mouth, but also in your hands, arms and throat Fatigue or weakness Painful menstrual periods Patchy hair loss, Dry, coarse skin, Brittle nails Depression or anxiety 60
- 61. CLASSIFICATION Acute Hypoparathyroidism : Acute hypoparathyroidism is caused by accidental damage to parathyroid tissues during thyroidectomy. It is characterized by greatly increased neuromuscular irritability, which results in tetany. Clients with tetany experience painful muscle spasms, irritability, grimacing, tingling of the fingers, laryngospasm, and dysrhythmias. Assessment also reveals Chvostek's and Trousseau’s signs. 61
- 62. CLASSIFICATION Chronic Hypoparathyroidism: Chronic hypoparathyroidism is usually idiopathic, resulting in lethargy; thin, patchy hair; brittle nails; dry, scaly skin; and personality changes. Ectopic or unexpected calcification may appear in the eyes and basal ganglia. Thus cataracts and permanent brain damage, accompanied by psychosis or convulsions, may develop. In addition, severe persistent hypocalcemia adversely affects the heart, causing dysrhythmias and eventual cardiac failure. The diagnosis of hypoparathyroidism is based on the following physical examination findings related to hypocalcemia. 62
- 63. DIAGNOSTIC FINDINGS Presence of Chvostek's sign , Trousseau’s sign , Hyperactive deep tendon reflexes (DTRS): A positive Trousseau’s sign or a positive Chvostek’s sign suggests latent tetany. Trousseau’s sign is positive when carpopedal spasm is induced by occluding the blood flow to the arm for 3 minutes with a blood pressure cuff. Chvostek’s sign is positive when a sharp tapping over the facial nerve just in front of the parotid gland and anterior to the ear causes spasm or twitching of the mouth, nose, and eye Circumoral paresthesia Numbness and tingling of fingers 63
- 64. COMPLICATIONS Reversible complication. Cramp like spasms of your hands and fingers that can be prolonged and painful, or muscle pain and twitches or spasms of the muscles of your face, throat or arms. When these spasms occur in your throat, they can interfere with breathing, creating a possible emergency. feeling, in your lips, tongue, fingers and toes. Seizures. Malformed teeth, affecting dental enamel and roots, in cases when hypoparathyroidism occurs at an early age when teeth are developing. Problems with kidney function. Heart arrhythmias and fainting, even heart failure. 64
- 65. COMPLICATIONS Irreversible complications: Stunted growth Slow mental development in children Calcium deposits in the brain, which can cause balance problems and seizures Clouded vision due to cataracts 65
- 66. PREVENTION There are no specific actions to prevent hypoparathyroidism. However, if you're scheduled to have thyroid or neck surgery, talk to your surgeon about the risk of damage to your parathyroid glands during the procedure. Test your calcium, parathyroid hormone and vitamin D levels and have you begin supplementation if needed before surgery. 66
- 67. PREVENTION If you've had surgery involving your thyroid or neck, watch for signs and symptoms that could indicate hypoparathyroidism, such as a tingling or burning sensation in your fingers, toes or lips, or muscle twitching or cramping. If they occur, your doctor might recommend prompt treatment with calcium and vitamin D to minimize the effects of the disorder. 67
- 68. MEDICAL MANAGEMENT The goal of therapy is to raise the serum calcium level to 9 to 10 mg/dL (2.2 to 2.5 mmol/L) and to eliminate the symptoms of hypoparathyroidism and hypocalcemia. When hypocalcemia and tetany occur after a thyroidectomy, the immediate treatment is to administer calcium gluconate intravenously. Because of neuromuscular irritability, the patient with hypocalcemia and tetany requires an environment that is free of noise, drafts, bright lights, or sudden movement. Tracheostomy or mechanical ventilation may become necessary, along with bronchodilating medications, if the patient develops respiratory distress. 68
- 69. MEDICAL MANAGEMENT The patient receiving parathormone is monitored closely for allergic reactions and changes in serum calcium levels. Because of neuromuscular irritability, the patient with hypocalcemia and tetany requires an environment that is free of noise, drafts, bright lights, or sudden movement. Tracheostomy or mechanical ventilation may become necessary, along with bronchodilating medications, if the patient develops respiratory distress. Therapy for the patient with chronic hypoparathyroidism is determined after serum calcium levels are obtained. A diet high in calcium and low in phosphorus is prescribed. Although milk, milk products, and egg yolk are high in calcium, they are restricted because they also contain high levels of phosphorus. 69
- 70. MEDICAL MANAGEMENT If this does not decrease neuromuscular irritability and seizure activity immediately, sedative agents such as pentobarbital may be administered. Parenteral parathormone can be administered to treat acute hypoparathyroidism with tetany. The high incidence of allergic reactions to injections of parathormone, however, limits its use to acute episodes of hypocalcemia. The patient receiving parathormone is monitored closely for allergic reactions and changes in serum calcium levels. Because of neuromuscular irritability, the patient with hypocalcemia and tetany requires an environment that is free of noise, drafts, bright lights, or sudden movement. Tracheostomy or mechanical ventilation may become necessary, along with bronchodilating medications, if the patient develops respiratory distress. Therapy for the patient with chronic hypoparathyroidism is determined after serum calcium levels are obtained. A diet high in calcium and low in phosphorus is prescribed. Although milk, milk products, and egg yolk are high in calcium, they are restricted because they also contain high levels of phosphorus. 70
- 71. MEDICAL MANAGEMENT Spinach also is avoided because it contains oxalate, which would form insoluble calcium substances. Oral tablets of calcium salts, such as calcium gluconate, may be used to supplement the diet. Aluminum hydroxide gel or aluminum carbonate (Gelusil, Amphojel) also is administered after meals to bind phosphate and promote its excretion through the gastrointestinal tract. Variable dosages of a vitamin D preparation—dihydrotachysterol (AT 10 or Hytakerol), ergocalciferol (vitamin D), cholecalciferol (vitamin D)—are usually required and enhance calcium absorption from the gastrointestinal tract. The goal of treatment is to relieve symptoms and to normalize levels of calcium and phosphorus in your body. A treatment regimen usually includes: Oral calcium carbonate tablets. Oral calcium supplements can increase calcium levels in your blood. However, at high doses, calcium supplements can cause gastrointestinal side effects, such as constipation, in some people. 71
- 72. MEDICAL MANAGEMENT Vitamin D. High doses of vitamin D, generally in the form of calcitriol, can help your body absorb calcium and eliminate phosphorus. Magnesium. If your magnesium level is low and you're experiencing symptoms of hypoparathyroidism, your doctor may recommend that you take a magnesium supplement. Thiazide diuretics. If your calcium levels remain low even with treatment, thiazide diuretics can help decrease the amount of calcium lost through your urine. However, some people with hypoparathyroidism, including people who inherited the condition, shouldn't take thiazide diuretics. Parathyroid hormone (Natpara). The U.S. Food and Drug Administration has approved this once-daily injection for treatment of low blood calcium due to hypoparathyroidism. Because of the potential risk of bone cancer (osteosarcoma), at least in animal studies, this drug is available only through a restricted program to people whose calcium levels can't be controlled with calcium and vitamin D supplements and who understand the risks. blood-calcium levels rise or fall 72
- 73. MEDICAL MANAGEMENT If you need immediate symptom relief, your doctor might recommend hospitalization so that you can receive calcium by intravenous (IV) infusion, as well as oral calcium tablets. After hospital discharge, you'll continue to take calcium and vitamin D orally. Your doctor will regularly check your blood to monitor levels of calcium and phosphorus. Initially, these tests will probably be weekly to monthly. Eventually, you'll need blood tests just twice a year. Because hypoparathyroidism is usually a long-lasting disorder, treatment generally is lifelong, as are regular blood tests to determine whether calcium is at normal levels. Your doctor will adjust your dose of supplemental calcium if your blood-calcium levels rise or fall 73
- 74. MEDICAL MANAGEMENT A diet high in calcium and low in phosphorus is prescribed. Although milk, milk products, and egg yolk are high in calcium, they are restricted because they also contain high levels of phosphorus. Spinach also is avoided because it contains oxalate, which would form insoluble calcium substances. 74
- 75. Rich in calcium. This includes dairy products, green leafy vegetables, broccoli and foods with added calcium, such as some orange juice and breakfast cereals. Low in phosphorus. This means avoiding carbonated soft drinks, which contain phosphorus in the form of phosphoric acid, and limiting meats, hard cheeses and whole grains DIET 75
- 76. Tracheotomy or Mechanical ventilation may become necessary, along with Broncho dilating medication if patient develops respiratory distress. Hormonal replacement therapy . A loss of central or peripheral vision blindness or changes in vision chronic eye pain SURGICAL MANAGEMENT 76
- 77. Prevent Respiratory Arrest. When caring for a client with severe hypoparathyroidism, always be prepared for laryngeal spasm and respiratory obstruction. Have an endotracheal tube, laryngoscope, and tracheostomy set available when caring for a client with acute tetany. When a client is at risk for sudden hypocalcemia, as after thyroidectomy, an ampule of intravenous calcium carbonate is usually kept at the bedsicde for immediate use if necessary. When the intravenous tubing is removed, it is sometimes capped so that rapid venous access is available. Sometimes clients are encouraged to ingest a ready source of calcium carbonate, such as Tums. If hypocalcemia is transient after a thyroidectomy, it usually resolves as edema decreases. If it is chronic, the client is usually able to manage the therapeutic regimen with minimal difficulty. Monitor for signs of tetany and report immediately to RN or physician so treatment can be instituted quickly. Make sure a tracheostomy set, endotracheal tube, and intravenous calcium are available for emergency use if laryngospasm occurs. Consult a dietitian for high-calcium diet teaching. The patient may need a lifelong high-calcium diet. Teach the patient about the importance of diet and medication therapy, and follow-up laboratory test- ing. The patient needs to understand self-care for follow-up at home. INEFFECTIVE BREATHING PATTERN RELATED TO HYPERVENTILATION AND LARYNGOSPASM CAUSED BY NEUROMUSCULAR IRRITABILITY. 77
- 78. Interventions Monitor vital signs, to assess elevating temperature, tachycardia, respiratory distress. Observe for nerve muscular irritability, e,g. numbness, paresthesias, twitching. Avoid restraining during seizures. Keep side rails raised and padded. Monitor serum calcium level. Administer anticonvulsants as prescribed to control the seizures activity. Ask for regular medical follow-up to monitor effectiveness of therapy and for prevention of fatal complications. RISK FOR INJURY: MUSCLE TETANY RELATED TO DECREASED SERUM CALCIUM LEVELS. 78
- 79. Establish guidelines and goals of activity with the patient. Evaluate the need for additional help at home. Have the patient perform the activity more slowly, in a longer time with more rest or pauses, or with assistance if necessary. Gradually increase activity with active range-of-motion exercises in bed, increasing to sitting and then standing. Dangle the legs from the bed side for 10 to 15 minutes. Refrain from performing nonessential activities or procedures. Assist with ADLs while avoiding patient dependency. Provide bedside commode as indicated. ACTIVITY INTOLERANCE RELATED TO WEAKNESS AND APATHY. 79
- 80. Ascertain healthy body weight for age and height. Refer to a dietitian for complete nutrition assessment and methods for nutritional support. Set appropriate short-term and long-term goals. Provide a pleasant environment. Promote proper positioning. Provide good oral hygiene and dentition. If patient lacks strength, schedule rest periods before meals and open packages and cut up food for patient. Provide companionship during mealtime. Consider the use of seasoning for patients with changes in their sense of taste; if not contraindicated. Consider six small nutrient-dense meals instead of three larger meals daily to lessen the feeling of fullness. For patients with physical impairments, refer to an occupational therapist for adaptive devices. RISK FOR IMBALANCED NUTRITION: LESS THAN BODY REQUIREMENT (CALCIUM LEVEL) R/T INADEQUATE CALCIUM DIET OR INTAKE. 80
- 81. Assist with treatment for underlying problems, such as anorexia, brain injury/increased intracranial pressure, sleep disorders, biochemical imbalances. Reorient to time/place/person, as needed. Have patient write name periodically; keep this record for comparison and report differences. Provide safety measures (e.g., side rails, padding, as necessary; close supervision, seizure precautions), as indicated. DISTURBED THOUGHT PROCESSES RELATED TO HYPOCALCEMIA INDUCED NEUROLOGIC DYSFUNCTION 81
- 82. Discuss the importance of long-term management and follow- up care, especially periodic checks of the patient's serum calcium levels. Advise the patient that long-term replacement therapy will be necessary. Instruct him to take the medication as ordered and not to discontinue it abruptly. Instruct the patient to take calcium supplements with or after meals and to chew the tablets well. Encourage the patient to wear a medical identification bracelet and to carry his medicatíon with him at all times HEALTH EDUCATION 82
- 83. Teach the patient and his family to identify and report signs and symptoms of hypercalcemia, tetany, and respiratory distress Teach the patient protective measures to decrease stress and to avoid fatigue and infection. Advise the patient to follow a high- calcium, low-phosphorus diet. Discuss foods high in calcium; for example, dairy products, salmon, egg yolks, shrimp, and green, leafy vegetables. Caution him to avoid high-phosphate foods, such as spinach, rhubarb, and asparagus. HEALTH EDUCATION 83
- 85. Parathyroid disorders can be controlled and the manifestations reversed if they are discovered in a timely manner and prompt and proper treatment is begun. You are an important resource for these clients, who require considerable education. You are also responsible for closely monitoring any client who needs Surgery for the parathyroid gland. SUMMARY AND CONCLUSION 85
- 86. RESEARCH scienti fi c reports Joon Ho, Donggyu Kim, Ji-Eun Lee, Namki Hong, Byung Moon Kim, Dong Joon Kim, Jinkyong Kim, Cho Rok Lee, Sang-Wook Kang, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung & Yumie Rhee Scienti fi c Reports volume 12, Article number: 7058 (2022) Cite this article • 301 Accesses • 1 Altmetric • Metrics Parathyroid venous sampling for the preoperative localisation of parathyroid adenoma in patients with primary hyperparathyroidism Abstract Preoperative localisation studies are essential for parathyroidectomy in patients with primary hyperparathyroidism. If the location of abnormal parathyroid glands cannot be identified through non-invasive studies, parathyroid venous sampling (PVS) may be employed. In this study, we evaluated the utility of preoperative PVS in parathyroid surgery. Patients with primary hyperparathyroidism who underwent preoperative PVS at Severance Hospital between January 2015 and June 2020 were identified. Patients for whom the results of non-invasive imaging studies were inconsistent or negative underwent PVS. The results of PVS were compared with operative findings and pathologic results. For 14 patients, the results of preoperative ultrasonography and 99mTc-sestamibi single-photon emission computed tomography (SPECT) were negative; for 20 patients, either the result of only one test was positive, or the results of the two tests were inconsistent. With respect to the lateralisation of diseased adenoma, the results of PVS and pathological examination were inconsistent only for one patient in either group (total: 2/34 patients). This study showed that PVS could be used effectively for preoperative localisation in patients with primary hyperparathyroidism in whom the location of diseased parathyroid glands cannot be determined through non-invasive image studies. Conclusions PVS may have certain limitations, but it is an exact technique for the preoperative localisation of parathyroid lesions and diseased parathyroid glands whose locations cannot be determined through non-invasive imaging studies. Therefore, PVS may be a sufficient complementary means when the location of the diseased parathyroid cannot be confirmed by imaging tests such as US, SPECT, 4D-CT, and PET. Consequently, with the use of PVS, it is possible to eliminate the need to perform operative bilateral neck exploration and enable the use of MIS, which is associated with less invasiveness to patients.
- 87. BIBLIOGRAPHY Brunner & suddarth’s, Medical-Surgical nursing,(2015) 10th edition, Page1743-47 Joyce.M.Black, Medical-Surgical nursing,(2020) 6th edition, Page 1687-1708 Williams.S. Linda,Understanding Medical Surgical Nursing, 3rd edition(2007), page 678-690 Taylor Carol, Fundamentals of nursing(2010), 5th edition Chintamani, Lewis Medical-surgical nursing,( 2011), 2nd edition,CBS Publications Priscilla Lemonne, Medical Surgical Nursing, 2nd edition https://accesspharmacy.mhmedical.com/data/interactiveguide/physexam/heent/ neckexamination.html https://pubmed.ncbi.nlm.nih.gov/21250067/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858710/