Respiratory failure
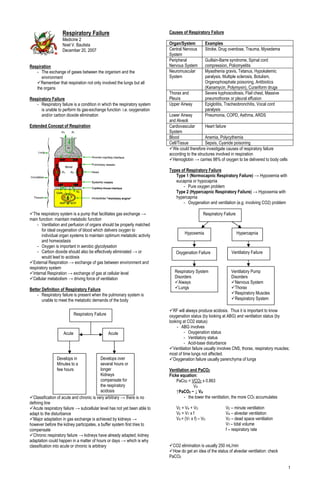
- 1. Respiratory Failure Causes of Respiratory Failure Medicine 2 Noel V. Bautista Organ/System Examples December 20, 2007 Central Nervous Stroke, Drug overdose, Trauma, Myxedema System Peripheral Guillain-Barre syndrome, Spinal cord Respiration Nervous System compression, Poliomyelitis - The exchange of gases between the organism and the Neuromuscular Myasthenia gravis, Tetanus, Hypokalemic environment System paralysis, Multiple sclerosis, Botulism, Remember that respiration not only involved the lungs but all Organophosphate poisoning, Antibiotics the organs (Kanamycin, Polymyxin), Curariform drugs Thorax and Severe kyphoscoliosis, Flail chest, Massive Respiratory Failure Pleura pneumothorax or pleural effusion - Respiratory failure is a condition in which the respiratory system Upper Airway Epiglotitis, Tracheobronchitis, Vocal cord is unable to perform its gas-exchange function i.e. oxygenation paralysis and/or carbon dioxide elimination Lower Airway Pneumonia, COPD, Asthma, ARDS and Alveoli Extended Concept of Respiration Cardiovascular Heart failure System Blood Anemia, Polycythemia Cell/Tissue Sepsis, Cyanide poisoning We could therefore investigate causes of respiratory failure according to the structures involved in respiration Hemoglobin → carries 98% of oxygen to be delivered to body cells Types of Respiratory Failure Type 1 (Normocapnic Respiratory Failure) → Hypoxemia with eucapnia or hypocapnia - Pure oxygen problem Type 2 (Hypercapnic Respiratory Failure) → Hypoxemia with hypercapnia - Oxygenation and ventilation (e.g. involving CO2) problem The respiratory system is a pump that facilitates gas exchange → Respiratory Failure main function: maintain metabolic function - Ventilation and perfusion of organs should be properly matched for ideal oxygenation of blood which delivers oxygen to Hypoxemia Hypercapnia individual organ systems to maintain optimum metabolic activity and homeostasis - Oxygen is important in aerobic glycolysation - Carbon dioxide should also be effectively eliminiated → or Oxygenation Failure Ventilatory Failure would lead to acidosis External Respiration → exchange of gas between environment and respiratory system Internal Respiration → exchange of gas at cellular level Respiratory System Ventilatory Pump Cellular metabolism → driving force of ventilation Disorders Disorders Aiways Nervous System Better Definition of Respiratory Failure Lungs Thorax - Respiratory failure is present when the pulmonary system is Respiratory Muscles unable to meet the metabolic demands of the body Respiratory System RF will always produce acidosis. Thus it is important to know Respiratory Failure oxygenation status (by looking at ABG) and ventilation status (by looking at CO2 status) - ABG involves Acute Acute - Oxygenation status - Ventilatory status - Acid-base disturbance Ventilation failure usually involves CNS, thorax, respiratory muscles; most of time lungs not affected. Develops in Develops over Oxygenation failure usually parenchyma of lungs Minutes to a several hours or few hours longer Ventilation and PaCO2 Kidneys Ficke equation: compensate for PaCo2 = VCO2 x 0.863 the respiratory VA acidosis ↑PaCO2 ~ ↓ VA Classification of acute and chronic is very arbitrary → there is no - the lower the ventilation, the more CO2 accumulates defining line Acute respiratory failure → subcellular level has not yet been able to VE = V A + V D VE – minute ventilation adapt to the disturbance VE = V T x f VA – alveolar ventilation Major adaptation in gas exchange is achieved by kidneys → VA = (VT x f) – VD VD – dead space ventilation however before the kidney participates, a buffer system first tries to VT – tidal volume compensate f – respiratory rate Chronic respiratory failure → kidneys have already adapted; kidney adaptation could happen in a matter of hours or days → which is why classification into acute or chronic is arbitrary CO2 elimination is usually 250 mL/min How do get an idea of the status of alveolar ventilation: check PaCO2 1
- 2. Minute ventilation affected by: Dalton’s Law: Tidal volume, respiratory rate, and dead space ventilation PB (barometric pressure) = PN2 + PO2 + PCO2 + PH2O ↑ Respiratory rate (tachypneic) does not assure you adequacy of = 760 mmHg (at sea level) ventilation normal atmospheric pressure Ventilatory Pump Failure Barometric pressure is the sum of all the partial - Central nervous system pressures of the most important gases in atmosphere - Peripheral nervous system Nitrogen is an inert gas; we breathe it without any - Thorax & Pleura physiological consequence - Respiratory muscles → myasthenia gravis Gas that we inhale is humidified Hypercapnia results from disturbance in ventilatory pump PiO2 = FiO2 x PB Causes of Hypoventilation (Hypercapnia) FiO2 = PiO2/PB = 160/760 = 21% - Brainstem PiO2 → fraction contributed by O2 - brainstem injury due to trauma, hemorrhage, infarction, FiO2 → available oxygen hypoxia, infection etc - metabolic encephalopathy Effects of Altitude on Barometric Pressure - depressant drugs - Spinal cord Altitude (Feet) PB (mmHg) PiO2 (mmHg) - trauma, tumor, transverse myelitis 0 760 159 - Nerve root injury 10,000 523 110 - Nerve 20,000 349 73 - trauma 30,000 226 47 - neuropathy eg Guillain Barre 40,000 141 29 - motor neuron disease 50,000 87 18 - Neuromuscular junction In the urban setting, decreased FiO2 is rarely the reason for - myasthenia gravis respiratory failure, except in cases of fire, CO poisoning - neuromuscular blockers - Respiratory muscles Alveolar Gases - fatigue - amount O2 that reaches alveoli - disuse atrophy - myopathy - malnutrition - Respiratory system - airway obstruction (upper or lower) - decreased lung, pleural or chest wall compliance Alveolar Air Saturated O2 100 mmHg (13%) N2 573mmHg (76%) Causes of Ventilatory Failure CO2 5mmHg (40%) H2O 47mmHg (6%) Increased VCO2 Fever, hypermetabolism Increased VD and Lung parenchyma disorders e.g. COPD, Decreased VA asthma, ARDS, pulmonary embolism Alveolar air equation: Decreased VA Decreased ventilatory drive e.g. sedation or PAO2 = (PB – PH2O) x FiO2 – (PaCO2/RQ) “Pump” failure e.g. neuromuscular disease = (760 – 47) x FiO2 – (PaCO2/RQ) If blood gases reveal hypercapnea, try to categorize them into the = 713 x FiO2 – (PaCO2/RQ) above three pathophysiological processes: = 713 x 0.21 – (40/0.8) = 99.7 mmHg 1. Increased CO2 production; rarely the cause, but can be an additional factor that adds to hypercapnea Alveolar Capillary Membrane More important factor is still diminished alveolar ventilation, not - When O2 reaches alveoli, next step is perfusion increase CO2 production so can forget about this, usually it is - Fick’s law: involves diffusion of gas on surface only co-conspirator however by itself will not cause hypercapnia 2. Increase in dead space (Minute ventilation is sum of alveolar ventilation and dead space ventilation) which will decrease alveolar ventilation. CO2 accumulates. Seen in obstructive airway diseases 3. Decreased alveolar ventilation Respiratory System Oxygenation - Inspired gases (PiO2, PiCO2) - Alveolar ventilation (Va, PAO2, PACO2) - Diffusion of gas through the respiratory membrane (DmO2) - Perfusion of pulmonary capillaries - Ventilation-perfusion matching (V/Q) Fick’s Law of Diffusion: Whenever there is hypercapnea, find reason. Do not rely on VO2 = DmO2 x ( PAO2 – PCO2) respiratory rate → request for PaCO2 Dm = Diffusing Capacity oxygenation failure – so many causes (Note: D is directly proportional to Area and Diffusion Coefficient for the gas and inversely proportional to diffusion Distance ~ D = [A x Inspired Air Dc]/T) *No need to memorize or apply equation → what is important is that Inspired Air: dry alveolar membrane should be in tip-top shape for the respiratory gases O2 160 mmHg (21%) to diffuse through Tracheal Air: Diffusion is fast → takes only a quarter of a second for desaturated N2 600 mmHg (79%) Saturated CO2 0 mmHg (0%) gas to be completely oxygenated O2 150 mmHg (20%) H2O 0 mmHg (0%) So even if you exercise → diffusion or the respiratory system is N2 563 mmHg (74%) CO2 0 mmHg (0%) usually not the problem but the cardiovascular system H2O 47 mmHg (6%) Exercise can improve the cardiovascular system improve oxygen delivery from 10-15x, but the reserve capacity of the cardiovascular system is even more (20-25x) in a normal resting physiologic bodies Bottomline: Diffusion is not a usual cause of hypoxemia 2
- 3. Ventilation-Perfusion Matching - The usual cause of hypoxemia Effect of Hypoventilation on Hypoxemia ↓Va → ↓PAO2 → ↓PaO2 ↓Va → ↑PaCO2 → ↓PaO2 1mmHg ~ 1.25mmHg Fixed Variable PB = PN2 + PH2O + PCO2 + PO2 760 573 47 40 100 mmHg Example: Dead space High V/Q Low V/Q Shunt Ventilation Ventilation Ventilation PaCO2 = 55 mmHg (change = 55 – 40 = 15) Expected PaO2 = 80 mmHg (80 – 15 x 1.25) = 61.25 If actual < expected → hypoventilation (plus other) Normal V/Q ratio = 0.8 Actual PaO2 = 60 mmHg Hypoventilation VQ matching or mismatching comes in a spectrum of physiologic Ventilation-Perfusion Mismatching events - Causes: A → complete ventilation but no perfusion; physiologic dead - Airway disorders space - Lung parenchymal disorders B → ideal VQ; ventilation is matched by perfusion. Most common cause of V/Q mismatch: Obstructive airway Normal VQ → slightly more perfusion than ventilation; some of disease blood flow goes back to heart unoxygenated. D→ no ventialtion but complete perfusion; shunt Shunt Defect Hard to determine A and D from one another; often lumped together Shunt Equation: Qs = CcO2 – CaO2 = 5-8% Alveolar-Arterial Oxygen Gradient QT CcO2 – CvO2 Causes: - Intracardiac PAO2 = 100 – 115 mmHg - Right to left shunt e.g. Fallot's tetralogy, Eisenmenger's syndrome P(A-a)O2 = 15=20 mmHg - Pulmonary - Pneumonia PaO2 = 80 – 100 mmHg - Pulmonary edema - Atelectasis Mechanisms of Hypoxemia - Pulmonary haemorrhage - Decreased inspired oxygen tension (FiO2) - Pulmonary contusion - Hypoventilation* - Ventilation – Perfusion (V/Q) mismatching* Dead Space Ventilation - Shunt defect* Ventilation - Diffusion defect - Causes *The more common causes of hypoxemia - Pulmonary embolism - Thrombus Normal Gas Exchange Va = 5L/min - Fat Perfusion - Tumor - Air - Septic Q = 0L/min - Pulmonary vasculitis Ventilation Diffusion Defect - Causes: Diffusion - Acute Respiratory Distress Syndrome - Interstitial lung disease - Fibrotic lung disease Tracheobronchial Tree Perfusion Hypoventilation - Hypoventilation can also lead to decrese in arterial oxygen, even if there’s no problem in parenchyma involved in gas exchange. Thus hypoxygenation can lead to hypoxemia. Airways divide dichotomously Airway decreases in size → ↑ surface area 70m2 80-120mL blood in capillaries for gas exchange ↓Va → ↓PAO2 → ↓PaO2 3
- 4. Diffusion Time Factors Affecting O2 Dissociation Curve Carbon Dioxide Dissociation Curve Extended Definition of Respiratory Failure Condition Definition Ventilatory Failure Abnormality of CO2 elimination by the lungs Failure of arterial Abnormality of O2 uptake by the lungs oxygenation Failure of O2 transport Limitation of O2 delivery to peripheral As PCO2 increases, oxygen carrying capacity diminishes. As PO2 tissues so that aerobic metabolism increases (especially in venous blood) there is decrease in CO2 cannot be maintained carrying capacity → Bohr effect Failure of O2 uptake Inability of tissues to extract O2 from and/or utilization blood and use it for aerobic metabolism Oxygen Consumption O2 Consumption (VO2) Oxygen Transport VO2 = Q x (CaO2 – CvO2) = 5 L/min x 5 mL/dL O2 transport (or delivery) (DO2) = 250 ml/min DO2 = Q x CaO2 = 5 L/min x 20 mL/dL x 10 CvO2 → oxygen content (venous) = 1,000 ml/min O2 Extraction ratio Q → cardiac output O2 ER = VO2 / DO2 = 250 mL/min / 1,000 mL/min O2 content (CaO2) = 0.25 (25%) CaO2 = (1.39 x Hb x %Sat) + (0.003 x PaO2) Safety mechanism at subcellular level has good application for = 1.39 x 15 x 0.98 + 0.003 x 98 = 20 ml/dl (vol%) cardiac arrest → must be able to resuscitate within 3-5 min → still be able to avoid brain damage/death/organ failure Oxygenation Dissociation Curve Clinical Manifestations of Respiratory Failure - Apnea → respiratory failure - Cyanosis → 5 mg of desaturated Hb already; only 20% of patients with respiratory failure will present with cyanosis → not a good parameter to measure - Altered level of consciousness - Dyspnea - Signs of respiratory distress - Signs/symptoms of hypoxemia - Signs/symptoms of hypercapnea - Signs/symptoms of underlying pathology Manifestations of Respiratory Distress and Respiratory Failure - Tachypnea and tachycardia - Flaring of ala nasae - Use of accessory muscles of respiration - Supraclavicular fossa excavation Note points - “Pump” handle breathing PO2 = 40 mmHg g Saturation → 75% (PvO2 for a normal - Tracheal tug and decreased tracheal length person at rest) - External jugular venous distension in expiration PO2 = 60 mmHg g Saturation → 90% - Costal paradox PO2 = 100 mmHg g Saturation → 97.5% (PaO2 for a normal - Pulsus paradoxus person at rest and in exercise) - Abdominal paradox and asynchrony Respirator distress; but P50 = 26 mmHg g Saturation → 50% (for normal Hb - Respiratory alternans there is impending In sepsis, may have no hypoxemia, but hypoxia - Cyanosis apnea → ventilation Hypoxemia → <50 mmHg - Altered level of consciousness failure in the next 15min Respiratory failure is not synonymous with respiratory distress. If there’s respiratory distress, investigate if there is RF 4
- 5. Evaluation of Hypoxemia Signs of Respiratory Distress - Normal P(A-a)O2 - Tachypnea and tachycardia - Decreased FiO2 - Flaring of ala nasae - Hypoventilation - Use of accessory muscles of respiration - Increased P(A-a)O2 - Intercostal muscle retraction - Ventilation-Perfusion mismatching - Sternocleidomastoid muscle contraction - Shunt defect - Costal paradox (Hoover’s sign) - Diffusion defect - “Pump” handle breathing Most common cause of hypoxemia: hypoventilation, V/Q - Supraclavicular fossae excavation mismatch & shunt - External jugular venous distension in expiration If with hypoxemia → calculate first P(A-a)O2 gradient - Tracheal tug and decreased tracheal length - Normal gradient → no problem in respiratory membrane & - Abdominal paradox and asynchrony V/Q, it will still go to arterial system - Respiratory alternans Indices of Oxygenation Signs and Symptoms of Hypercapnea - Symptoms Indices Normal Values Headache Pa O 2 80 – 100 mmHg Mild sedation → Drowsiness → Coma Sa O 2 95 – 100 vol% - Signs P(A-a)O2 25 – 65 mmHg Vasodilation → redness of skin, sclera and conjunctiva PaO2/PAO2 0.75 secondary to increased cutaneous blood flow; sweating PaO2/FiO2 350 – 450 Sympathetic response → hypertension tachycardia QS/QT <5% ”Antok” PAO2 = (PB – PH2O) x FiO2 – (PaCO2/RQ) = (760 – 47) x FiO2 – (PaCO2/RQ) Signs and Symptoms of Hypoxia = 713 x FiO2 – (PaCO2/RQ) - Symptoms PaO2/PAO2 = 0.15 → severe respiratory failure Ethanol-like symptoms → confusion, loss of judgment, There are many oxygenation parameters. It is not adequate to look paranoia, restlessness, dizziness at just PaO2. Must look at other oxygenation parameters - Signs Sympathetic response → tachycardia, mild hypertension, Algorithm of Hypoxemia peripheral vasoconstriction Non-sympathetic response → bradycardia, hypotension ”Lasing” P(A-a)O2 - Inhibitions depressed COPD → chronic hypoxemia, irritable Normal Increased Diagnosis of Respiratory Failure - Patient is in respiratory distress - Hypoxemia (PaO2 < 60 mmHg) - Hypercapnia (PaCO2 > 50 mmHg) PaCO2 Challenge with - Arterial pH shows significant acidemia (respiratory acidosis) 100% FiO2 *At least 2 of the 4 criteria should be fulfilled Only way to diagnose RF is to do ABG. It is a laboratory diagnosis, not a clinical diagnosis Increased Normal or Corrected Uncorrected Decreased PaO2 PaO2 Other Diagnostic Modalities - Laboratory Hypo - Decreased V/Q mismatch Shunt - CBC ventialtion FiO2 Shunt <10% >10% - Electrolytes - Imaging studies Diffusion defect - Chest x-ray - CT scan Principles of Treatment - Ventilation-perfusion scan - Maintain adequate oxygenation - Support ventilation with mechanical ventilation when needed Evaluation of Causes of Hypercapnia - Treat underlying illness or pathophysiologic derangements - Maintain fluid and electrolyte balance Minute Ventilation (VE) - Provide adequate nutrition - Avoid complications Transcribed by: Fred Monteverde Increased VE Decreased VE Notes from: Cecile Ong Lecture recorded by: Lala Nieto Increased VCO2 Increased VD & Decreased VA Decreased VA Fred Monteverde Mae Olivarez Emy Onishi Lala Nieto Cecile Ong Chok Porciuncula Airway or Lung Decreased “Pump” Mitzel Mata Section C 2009! parenchyma ventilatory Regina Luz disorders disorders drive Fever COPD, Sedation Neuromuscular Hypermetabolism ARDS, Stroke disorder Asthma, PE Pleural effusion 5
