Recording of arterial blood pressure and Special circulation
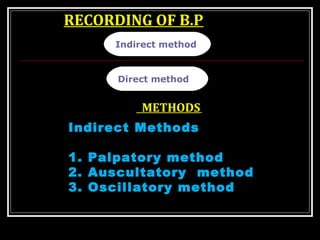
- 1. RECORDING OF B.P Direct method Indirect method METHODS Indirect Methods 1. Palpatory method 2. Auscultatory method 3. Oscillatory method
- 3. 3 RECOMMENDED BLOOD PRESSURERECOMMENDED BLOOD PRESSURE MEASUREMENT TECHNIQUEMEASUREMENT TECHNIQUE 2. • The cuff must be level with heart. • If arm circumference exceeds 33 cm, a large cuff must be used. • Place stethoscope diaphragm over brachial artery. 2.2. •• The cuff must be level with heart.The cuff must be level with heart. •• If arm circumference exceeds 33 cm,If arm circumference exceeds 33 cm, a large cuff must be used.a large cuff must be used. •• Place stethoscope diaphragm overPlace stethoscope diaphragm over brachial artery.brachial artery. 1. • The patient should be relaxed and the arm must be supported. • Ensure no tight clothing constricts the arm. 1.1. •• The patient shouldThe patient should be relaxed and thebe relaxed and the arm must bearm must be supported.supported. •• Ensure no tightEnsure no tight clothing constrictsclothing constricts the arm.the arm. 3. • The column of mercury must be vertical. • Inflate to occlude the pulse. Deflate at 2 to 3 mm/s. Measure systolic (first sound) and diastolic (disappearance) to nearest 2 mm Hg. 3.3. •• The column ofThe column of mercury must bemercury must be vertical.vertical. •• Inflate to occlude theInflate to occlude the pulse. Deflate at 2 topulse. Deflate at 2 to 3 mm/s. Measure3 mm/s. Measure systolic (first sound)systolic (first sound) and diastolicand diastolic (disappearance) to(disappearance) to nearest 2 mm Hg.nearest 2 mm Hg. StethoscopeStethoscope MercuryMercury machinemachine
- 4. Palpatory methodPalpatory method The radial pulse (the pulse at the radial artery in the wrist) is palpated with the fingers of the left hand.
- 5. Auscultatory methodAuscultatory method • The brachial pulse is palpated just above the angle of the elbow (the "antecubital fossa"). • The diaphragm of stethoscope is placed over the brachial artery in the space between the bottom of the cuff and the crease of the elbow. At this point no sounds should be heard
- 7. PRINCIPLE INVOLVED IN RECORDING BLOOD PRESSURE
- 8. • At some point the personnel listening with the stethoscope will begin to hear sounds with each heartbeat. This point marks the systolic pressure. • The sounds are called “Korotkoff” sounds.
- 10. Tapping sound 1SBP 110 mm Hg Banging sound 3 Muffing sound 4 DBP- 95 mm Hg 85 mm Hg 120 mm Hg Murmurish 2 80 mm Hg No sound 5 AUSCULTATORY METHOD (Korotkov sounds) This method was introduced by a Russian physician Korotkov
- 11. BASIS OF KOROTKOFF’SBASIS OF KOROTKOFF’S SOUNDSOUND Sounds are heard due to turbulenceSounds are heard due to turbulence Cuff pressure > Systolic. P Lumen isCuff pressure > Systolic. P Lumen is occluded No sounds are heard.occluded No sounds are heard. Cuff pressure <just below> systolic .PCuff pressure <just below> systolic .P Blood flow at height of systoleBlood flow at height of systole Tapping soundTapping sound Cuff pressure < diastolic.PCuff pressure < diastolic.P Streamline flow No sounds.Streamline flow No sounds.
- 12. AUSCULTATORY GAPAUSCULTATORY GAP A gap present afterA gap present after tapping soundtapping sound Seen in hypertensive patientsSeen in hypertensive patients..
- 15. PATHOLOGICAL VARIATION IN BP 1.Hypertension 2. Hypotension Persistent increase in systemic arterial B.P is known as hypertension. Normal - 120/80 mmHg. Pre hypertension – 120-139/80-89mmHg Stage I Hypertension- 140-159/90-99 mmHg Stage II Hypertension- >/160/100mmHg Fall in B.P below normal range is known as hypotension. Clinically, when the systolic blood pressure is less than 90 mm Hg, it is considered hypotension.
- 16. 04/15/1804/15/18 ↑ BP is called Hypertension (Above 140/90 mm of Hg ) Primary (Essential 90%) Secondary (10%)
- 17. Hypertension Defined as an elevation of systolic blood pressure Persistent hypertension very common 30% of people over 50 are hypertensive Never diagnosed on one reading Indication of cardiovascular disease Trauma Side effect of medication
- 18. Benign Primary Hypertension Malignant Secondary -Atherosclerosis -Pheochromocytoma -Cushing syndrome -Glomerulonephritis -Gestational -Drug induced White coat hypertension
- 19. Diseases Attributable to Hypertension Hypertension Heart failure Stroke Coronary heart disease Myocardial infarction Left ventricular hypertrophy Aortic aneurysm Retinopathy Peripheral vascular disease Hypertensive encephalopathy Chronic kidney failure Cerebral hemorrhage Adapted from: Arch Intern Med 1996; 156:1926-1935. All Vascular
- 20. 04/15/1804/15/18 Hypertension Predisposing factors: Obesity Hereditary Alchoholism Stress Smoking Sedentary life
- 21. 04/15/1804/15/18 Secondary Hypertension Causes: 1.Renal-Acute & Chronic Glomerulonephritis,Nephrotic syndrome 2.Endocrine- Cushings,Conns,Thyrotoxicosis, Pheochromacytoma 3.Vascular-Atherosclerosis Arteriosclerosis
- 22. 04/15/1804/15/18 Secondary Hypertension Causes: 1.Renal-Acute & Chronic Glomerulonephritis,Nephrotic syndrome 2.Endocrine- Cushings,Conns,Thyrotoxicosis, Pheochromacytoma 3.Vascular-Atherosclerosis Arteriosclerosis
- 23. COMPLICATIONS OFCOMPLICATIONS OF HYPERTENSIONHYPERTENSION Renal failure LVH MI Cerebral haemorrhage Retinal haemorrhage
- 24. 04/15/1804/15/18 Treatment of Hypertension Modification of lifestyle: Cessation of smoking. Moderation in alcohol intake. Weight reduction. Programmed exercise. Reduction in Na+ intake. Diet high in K+ . Relaxation technique – Yoga, TM
- 25. 04/15/1804/15/18 Treatment of Hypertension Medications: Diuretics: Increase urine volume. Beta-blockers: Decrease HR. Calcium antagonists: Block Ca2+ channels. ACE inhibitors: Inhibit conversion to angiotensin II. Angiotension II-receptor antagonists: Block receptors.
- 26. MANAGEMENT OFMANAGEMENT OF HYPERTENSIONHYPERTENSION Non drug therapy Stop smoking Control obesity Regular exercise Decrease salt intake Drug therapy Beta blockers Calcium channel blockers Vasodialators Diuretics ACE inhibitors VMC depressors
- 27. HYPOTENSIONHYPOTENSION Fall in B.P below normal range is known as hypotension. TYPES Primary/Essential hypotension. Secondary hypotension. -MI -Hypoactivity of pituitary gland -Hypoactivity of adrenal gland -Tuberculosis Orthostatic hypotension
- 28. Hypotension Defined in adults as a systolic pressure below 100mm Hg Rarely treated in this country
- 29. 04/15/1804/15/18 ↓ BP is called Hypotension (Below 90/60 mm of Hg) 1. Hemorrhage 2. Dehydration 3. Vomiting 4. Diarrhea 5. Excessive sweating 6.Adissons disease 7.Hypothyroidism
- 30. Prevention Reduce the risk of developing High Blood Pressure by making lifestyle changes….. Eat a healthy , well balanced diet Reduce salt and fat intake Exercise regularly Stop smoking Reduce alcohol and caffeine consumption to recommended levels Reduce weight
- 31. TREATMENT OFTREATMENT OF HYPOTENSIONHYPOTENSION Correct the underlying etiology. Orthostatic hypotension Change to supine position with head below the heart level & leg raised.
- 32. 04/15/1804/15/18 Treatment of Hypotension Treat the cause Blood transfusion I.V. Fluids Vasoconstrictors
- 33. 04/15/1804/15/18 RECAP At the end of this class, you should able to recall. 1. Definition of Blood Pressure 2. Its variations. 3. Measurement - Korotkov sound 4. Factors contributing to B.P 5. Peripheral resistance 6. Regulation of BP 7. Immediate regulation 8. Short term regulation 9. Long term regulation. 10. Applied - Hypertension - Hypotension
- 35. The blood flow to individual organs must vary to meet the needs of the particular organ as well as of the whole body
- 36. Neural, myogenic, metabolic, and endothelial mechanisms control regional blood flow Local or regional circulation of tissue blood flow is controlled in two phases Acute and chronic 1. Vasodilator theory- special role of adenosine 2. Oxygen lack theory/ nutrient lack theory 1. Autoregulation 2. Endothelial derived relaxing (NO)and constricting factors(endothelin) 1. Change in tissue vascularity 2. role of oxygen 3. endothelial derived vascular growth factors
- 43. RCA → post. Interventricular branch → marginal br.. .LCA → Ant. Interventricular branch → circumflex
- 44. Two coronary arteries(Rt & Lt) Arises from the root of aorta Supply blood to myocardium.
- 52. Phasic changes in coronary blood flow Myocardial blood flow depends upon - pressure head i.e. aortic pressure - resistance offered to blood flow during various phases of cardiac cycle.
- 53. Characteristics of coronary Circulation O2 consumption of myocardium • Very high - @ 8 ml / 100 gm / mt at rest • Other tissues extract 25% O2/ unit of blood • But myocardium extract 70-80% O2/ unit of blood • During exercise O2extraction reaches to 100 % & B. flow also increases.
- 55. Two coronary arteries(Rt & Lt) Arises from the root of aorta Supply blood to myocardium.
- 58. Perfusion of cardiac muscle from epicardium –endocardium
- 65. Heart utilize varieties of substances for metabolism Free fatty acid, pyruvates, glucose, lactate, ketone bodies and amino acids. More than 60% of myocardial O2 consumption in the fasting state is due to the oxidation of fatty acids. When the O2 supply is adequate, the heart takes up and oxidizes both lactate and pyruvate, as do red (i.e., oxidative) skeletal muscle fibers, although the arterial concentration of pyruvate is usually low.
- 66. Characteristics of coronary Circulation 1-Blood flow variations in coronaries - In 50% individuals RCA has greater flow - In 20% LCA, & - In 30% flow is equal in both LCA &RCA • Normal blood flow at rest – 250 ml ( 70ml / 100 gm / mt ) – @ 5% of CO • During exercise – 3-6 fold increase in flow • LV blood flow – 80 ml / 100 gm / mt • RV blood flow – 40 ml / 100 gm / mt • LA blood flow – 20 ml / 100 gm / mt • RA blood flow – 10 ml / 100 gm / mt
- 68. Comparison of oxygen supply & consumption by myocardium and other body tissues Oxygen content Other tissues Myocardium - Arterial 19 ml % 19 ml % - Venous 14 ml % 06 ml % AV Difference 05 ml % 13 ml % Coefficient of O2 utilization 5/19 x100 13/19 x 100 = 26 % = 69% O2 saturation of venous blood 14/19 x100 06/19 x 100 = 74 % = 31 % pO2 40 mm Hg < 20 mm Hg
- 69. 2- Phasic Changes in coronary blood flow
- 70. 2-Phasic changes in coronary blood flow Myocardial blood flow depends upon - pressure head i.e. aortic pressure - resistance offered to blood flow during various phases of cardiac cycle.
- 73. Systolic compression has more effect on BF in the endocardial layer CBF is 10-30% of that during Cardiac diastole
- 74. Blood flow to LV during systole • Like sk. Muscle myocardium compresses coronary vessels during systole. • LV pressure (121) > aortic pr. (120). • So LV blood flow practically ceases to LV (max during isovolumetric contraction phase) especially in subendocardial portion. So this part is prone to ISCHEMIC changes. • Epicardial parts do receive some B. flow during systole.
- 75. Blood flow to LV during diastole • Myocardial muscles relax during diastole & B.flow rises(max during isovolumetric relaxation phase) • Aortic pr. > LV pr. so blood flow rises
- 76. Right coronary blood flow Left coronary blood flow * The peak left coronary flow occurs at the end of isovolumetric relaxation *
- 78. Blood flow to RV, RA & LA • Rt. coronary blood flow shows similar phasic changes as in Lt. coronary A. • Pressure in aorta > RV & in aorta > RA during systole so coronary flow in these three parts is not appreciably reduced. • Thus blood flow to RV, RA & LA occurs both during systole & diastole.
- 86. Applied aspects • Subendocardial parts are more prone to ischemic changes as during systole blood flow ceases to LV • In AS (aortic stenosis) LV pressure > aorta causing severe compression of coronaries.during systole leading to ischemic changes. • In CHF, venous pr. > aortic pr. In diastole causing decreased coronary perfusion pr. & low coronary blood flow.
- 89. Regulation of coronary blood flow Three mechanisms . Local control mechanism 2.Nervous control mechanism 3. Neuro - hormonal control ANS control CBF
- 90. 1. Local control mechanism a. Autoregulation b. Role of local metabolites c. Role of endothelial cells
- 92. a. Autoregulation It is the ability of tissues/organ to maintain a relatively constant blood flow over a wide range of arterial blood pressure. By Adjusting vascular resistance according to changes in arterial pressure.
- 93. Autoregulation Autoregulation is well developed in – - Kidney - Heart - Brain - Sk. Muscles & mesentary
- 95. a. Autoregulation Two mechanisms – (i) Metabolic theory ↓ BP → ↓ B. flow → ↑ local accumulation of vasodilator subs. e.g.CO2, B.flow comes H+, adenosine, NO, PG, to normal K+, PO4--, ↑ O2 ↓ resistance art. dilatation
- 96. a. Autoregulation (ii) Myogenic theory Vascular smooth muscles respond to wall tension depends on art. Pressure & radius. ↑ BP → ↑ stretching of wall → VSM contracts ↓ ↓ BP ← ↓ B. flow ← narrowing of lumen
- 97. Reactive hyperemia Defined as increased blood flow to the organ/tissues after the removal of blockage in a previously blocked artery. Magnitude of reactive hyperemia depends on – duration of occlusion Cause of R. hyperemia – adenosine release
- 98. b. Role of local metabolites At rest myocardium extracts 60 - 70 % O2 from Hb. So not much additional O2 can be provided to myocardium unless blood flow increase due to vasodilation. Cause of vasodilation – Adenosine release in hypoxic states. Most imp. factor B. flow ↑ ― myocardial O2 consumption ↑(linear relation)
- 99. b. Role of local metabolites Direct effect of ↓ pO2 on arterioles vasodilation Role of other metabolites - H+ , NO, PG, adenosine, CO2 etc. are vasodilators.
- 101. c.Role of endothelial cells Endo. Cells release several vasodilators e.g. EDRF, prostacyclin (PGI2) & EDHF Endo. Cells also release several vasoconstrictors e.g. endothelin-1(ET-1), Angiotensin II, EDCF.
- 102. 2. Nervous control ANS control CBF – a. Directly b. Indirectly a. Direct nervous control is exerted via symp. & parasymp effects on coronary vessels. b. Indirect nervous control is exerted via symp. & parasymp effects on heart.
- 103. Direct nervous control Parasymp.nerves to coronaries are too less there fore have a negligible effect. Symp. Nerves extensively innervates coronary vessels. Receptors – α- present mainly on epicardial vessels β- present mainly on intramuscular vessels NT - NE reacts with α → vasoconstriction - E reacts with β → vasodilation Net effect is vasodilatation
- 104. Indirect Nervous control Through action on heart Symp. Stimulation → ↑ HR & force of contr ↓ ↑B. flow ← ADP cause ← ADP ← ATP vasodilation conversion Parasymp. Stimulation produce opp. effect
- 105. 3. Neuro – hormonal control ATP → vasoconstriction (P1 receptors) → vasodilation (P2 receptors) NPY (neuropeptide Y) → vasoconstriction CGRP (calcitonin gene related peptide) & Substance P → vasodilation
- 109. Special Features of coronary Circulation 1. Receive -5 % of C.O i.e. 225ml/min. 2. Distribution of coronary arteries blood flow varies 3. Heart receives major blood supply during diastole 4. the coronary arteries are end arteries i.e. phasic blood flow 5. Metabolic regulation is well developed and show autoregulation 6. There is adequate coronary blood flow reserve 7. Major source of energy is free fatty acids (1/3) 8. Heart muscles extract about 80 % of oxygen from arterial blood, AV difference is high even at rest.
- 111. Coronary Artery Disease blood flow Myocardial ischemia (“angina pectoris” means chest pain) Accumulation of ‘P’ factor If myocardial ischemia prolong and severe, results in myocardial infarction (Heart Attack) main factors coronary atherosclerosis Fatty deposits build up in blood vessel walls and narrow the passageway for the movement of blood. The resulting condition, called atherosclerosis often leads to eventual blockage of the coronary arteries and a “heart attack”.
- 113. Risk factors for CAD include: Coronary artery disease is one of the most common - Serious effects of aging, Gender, Haemostatic factors, Diabetes, Alcohol intake, Hypertension , Family history, Hypercholesterolemia, Stress Homocysteine etc.
- 116. Myocardial Infarction (Heart Attack) Blockage more then 75% Results in Cell death or infarction occurs Fig:- Acute Myocardial Infarction (AMI )
- 117. Acute Myocardial Infarction (AMI ) Severe Chest pain That radiates along the ulnar border of the upper arm, arm and hand With excessive sweating
- 118. 15/04/18 118 Diagnosis Acute Myocardial Infarction (AMI ) ECG- Elevated ST segment Plasma enzymes- elevated levels of enzymes – Creatine kinase (CK-MB) and Lactate dehydrogenase (fraction 1 of LDH) Typical clinical presentation – Severe Chest pain With excessive sweating
- 119. Treatment- Vasodilators -Nitrates (Nitroglycerine) Streptokinase, TPA Coronary angioplasty Calcium channel blockers (Verapamil) Antiplatelet aggregating agents- Low dose of aspirin Folic acid and Vitamin B12- inhibits homocysteine and convert it methionine a non toxic agent surgical by coronary artery bypass graft (Aortic CABG)
- 121. Important notes of Cerebral blood flow and metabolism Brain tissue is highly sensitive to hypoxia- Brain need continuous blood flow. Interruption of blood flow only for 5-20 seconds causes a loss of consciousness. Circulatory arrest for only 3-4 minutes results in irreversible brain damage. utilizes glucose as main fuel which is independent of insulin (except ventro-medial hypothalamus)
- 122. SPECIAL FEATURES OF CEREBRAL BLOOD FLOW: Brain has a very rich blood supply. Normal blood flow to brain (less than 2% of the body weight) 15% of the CO (750 mL/min) or 50–55 mL blood/100 g tissue/min. When cerebral blood flow falls below 18 mL/100 g tissue/ min (critical flow level), there occurs unconsciousness.
- 123. Total O2 consumption of the brain is 40-50 mL/min (3.3 mL/100 g tissue/min), i.e. 20% of the whole body at rest. O2 consumption of grey matter (GM) is much more than the white matter, possible because of high density of capillary network. SPECIAL FEATURES conti…
- 124. Cerebral arteries are end arteries and Brain present in rigid cage so intracranial content is incompressible therefore increase cerebral blood flow associated with comparable increase in venous outflow Volume of fluid and ECF remains constant Monrokellie Doctrine At any given time total blood volume, CSF voume and brain tissue in the cranial cavity remains constant SPECIAL FEATURES conti…
- 125. Capillaries are non - fenestrated and surrounded by end feet process of astrocytes forming BBB. Very tight junction between endothelial cells of capillaries. SPECIAL FEATURES conti…
- 126. Cerebral blood vessels and circulations
- 127. Arterial supply - 3 Pairs of cerebral arteries
- 128. Circle Of Willis
- 129. Arteries to the Brain “Putting it all Together” Arteries to the Brain “Putting it all Together” CEREBRAL BLOOD VESSELS Arterial supply -3 Pairs of cerebral arteries CAROTID SYSTEM Two internal carotid a. CAROTID SYSTEM Two internal carotid a. VERTEBROBASILAR SYSTEM 2 vertebral a. VERTEBROBASILAR SYSTEM 2 vertebral a.
- 130. Overview of arterial cerebral circulationOverview of arterial cerebral circulation CAROTID SYSTEM 70% CAROTID SYSTEM 70% VERTEBROBASILAR SYSTEM 30% VERTEBROBASILAR SYSTEM 30%
- 131. Overview of cerebral circulation
- 132. Each artery give rise to two set of branches Cortical branches Ramify on the surface of the Cerebral hemisphere and Supply the cortex. Central or perforating branches Pass deep into the substance of the cerebral hemisphere to supply the structure within it. Consist of six main groups.
- 133. Deep brain structures Arteries of cerebral haemorrhage
- 135. Cerebral VeinsCerebral Veins • Drain the cortex and subcortical white matter. • Drain the substance of the brain including basal ganglia,and diencephalon. Both superficial and deep veins communicate by anastomotic veins. Both superficial and deep veins communicate by anastomotic veins. Superficial veins : (sinuses) Superficial veins : (sinuses) Deep veins:Deep veins:
- 136. Venous drainage at a glanceVenous drainage at a glance
- 137. Innervation of cerebral blood vessels • arteries & arterioles supplied with • Sympathetic fibers . (superior Cervical Ganglia) NT is NE,NeuropeptideY. • Para sympathetic fibres- (Sphenoplantine ganglia) Cholinergic neurons. NT is Ach,VIP,PHM27. • Sensory fibers (trigeminal ganglia) are also present in distal arteries • Touch & pull of these vessels cause pain (no pain fibers) • arteries & arterioles supplied with • Sympathetic fibers . (superior Cervical Ganglia) NT is NE,NeuropeptideY. • Para sympathetic fibres- (Sphenoplantine ganglia) Cholinergic neurons. NT is Ach,VIP,PHM27. • Sensory fibers (trigeminal ganglia) are also present in distal arteries • Touch & pull of these vessels cause pain (no pain fibers)
- 139. Cerebral blood flow depends on REGULATION OF CEREBRAL BLOOD FLOW The perfusion pressure which determines cerebral blood flow is the difference between the mean arterial pressure at the head level and the internal jugular pressure (cerebral venous pressure).
- 140. Phenomenon of Auto regulation • Between MAP 65-140mm Hg blood flow of brain remain constant
- 141. • If BP<60mmHg cerebral blood flow is extremely compromised syncope. • If BP>140mm Hg disruption of blood brain barrier, cerebral edema or Hemorrhage may result • Both Metabolic theory & Myogenic theory of autoregulation are considered. • In metabolic theory main regulating substance of cerebral blood flow is pco2 • If BP<60mmHg cerebral blood flow is extremely compromised syncope. • If BP>140mm Hg disruption of blood brain barrier, cerebral edema or Hemorrhage may result • Both Metabolic theory & Myogenic theory of autoregulation are considered. • In metabolic theory main regulating substance of cerebral blood flow is pco2
- 142. Intrinsic Regulation of Blood Flow (Autoregulation) Intrinsic Regulation of Blood Flow (Autoregulation) • Maintains fairly constant blood flow despite BP variation • Myogenic control mechanisms occur in some tissues because vascular smooth muscle contracts when stretched & relaxes when not stretched – E.g. decreased arterial pressure causes cerebral vessels to dilate & vice versa • Maintains fairly constant blood flow despite BP variation • Myogenic control mechanisms occur in some tissues because vascular smooth muscle contracts when stretched & relaxes when not stretched – E.g. decreased arterial pressure causes cerebral vessels to dilate & vice versa
- 143. Intrinsic Regulation of Blood Flow (Autoregulation) continued • Metabolic control mechanism matches blood flow to local tissue needs • Low O2 or pH or high CO2, adenosine, or K+ from high metabolism cause vasodilation which increases blood flow • Metabolic control mechanism matches blood flow to local tissue needs • Low O2 or pH or high CO2, adenosine, or K+ from high metabolism cause vasodilation which increases blood flow 14-40
- 144. The auto regulation of cerebral blood flow is seen only when the arterial pco2 & po2 are maintained at their normal values The auto regulation of cerebral blood flow is seen only when the arterial pco2 & po2 are maintained at their normal values
- 145. Effect of Pco2 Effect of Pco2 • Physiologically partial pressure of co2 is most potent vasodilator of cerebral blood vessels. • With in arterial Pco2there occurs a linear in cerebral blood flow. • However when Pco2 increases above 80mmHg no further in cerebral blood flow (due to max. dilatation) • When Pco2 is below 20mmHg no further in cerebral blood flow (due to vasoconstriction) • Physiologically partial pressure of co2 is most potent vasodilator of cerebral blood vessels. • With in arterial Pco2there occurs a linear in cerebral blood flow. • However when Pco2 increases above 80mmHg no further in cerebral blood flow (due to max. dilatation) • When Pco2 is below 20mmHg no further in cerebral blood flow (due to vasoconstriction)
- 146. Effect of Pco2 Effect of Pco2 • A rise of Pco2 of 1mmHg above normal range, increases cerebral blood flow by 3ml/100gm/min • A fall of Pco2 of 1mmHg below normal range decreases cerebral blood flow by 1.5ml/100gm/min • Effect of Co2 is mediated via change in Ph. • A rise of Pco2 of 1mmHg above normal range, increases cerebral blood flow by 3ml/100gm/min • A fall of Pco2 of 1mmHg below normal range decreases cerebral blood flow by 1.5ml/100gm/min • Effect of Co2 is mediated via change in Ph.
- 147. Maintaining cerebral blood flow CBF regulated by levels of CO2 and H+ in arterial blood Increase in CO2 / H+ / decrease O2 : - vasodilation occurs - increases blood flow Normally CBF constant More active regions of brain receive increased blood flow E.g. during exercise motor areas receive increased blood flow at expense of other areas Why? Because of increase in levels of CO2 / H+ and decrease in O2 in those areas. Maintaining cerebral blood flow CBF regulated by levels of CO2 and H+ in arterial blood Increase in CO2 / H+ / decrease O2 : - vasodilation occurs - increases blood flow Normally CBF constant More active regions of brain receive increased blood flow E.g. during exercise motor areas receive increased blood flow at expense of other areas Why? Because of increase in levels of CO2 / H+ and decrease in O2 in those areas.
- 150. Increased Intracranial Pressure The effects of an increase in ICP can be more serious than condition causing it. An increase in ICP can: - disrupt blood supply - distort shape of brain Causes of increased ICP: - Expanding lesions, e.g haematoma, tumour -Hydrocephalus, -i.e. accumulation of excess CSF Increased Intracranial Pressure The effects of an increase in ICP can be more serious than condition causing it. An increase in ICP can: - disrupt blood supply - distort shape of brain Causes of increased ICP: - Expanding lesions, e.g haematoma, tumour -Hydrocephalus, -i.e. accumulation of excess CSF Role of Intracranial Pressure
- 151. Effect of intracranial pressure changesEffect of intracranial pressure changes ICP – Intracranial pressure CPP- effective cerebral perfusion pressure • Any change in ICP causes change in venous pressure
- 154. Clinical importance Stroke - Two types Ischemic Hemorrhagic Blockage Rupture mainly branch of Thromboembolism middle Cerebral a. Treatment- Fibrinolytic drugs - Antiexitotoxic drugs Decrease glutamate conc. locally
- 155. Cause- arteriosclerotic plaques in arteries in brain Clotting mechanism Clot formation Block artery Acute loss of brain function in a localized area
- 157. Effect of negative gEffect of negative g • If the body is accelerated downwards, force acting towards the head increases arterial pressure at head level • ICP also rises, so the vessels are supported and do not rupture • If the body is accelerated downwards, force acting towards the head increases arterial pressure at head level • ICP also rises, so the vessels are supported and do not rupture
- 158. CSF occupies @ 10% of the intracranial volume with a pressure between 0 to 7mmHg .when CSF volume CSF occupies @ 10% of the intracranial volume with a pressure between 0 to 7mmHg .when CSF volume • CSF gets displaced into the spinal canal. This mechanism provides @ 65% of compensatory capacity of the rigid skull. • Beyond this even small increase in CSF volume causes marked in ICP • CSF gets displaced into the spinal canal. This mechanism provides @ 65% of compensatory capacity of the rigid skull. • Beyond this even small increase in CSF volume causes marked in ICP
Notas del editor
- When blood pressure rises the blood travelling along the arteries roughens the lining of the arteries. To understand why this happens, picture what occurs when you turn a tap on. At normal pressure the water travels in a straight line, but when you turn the tap on full blast the water spurts out in all directions. Before it comes out it has been pushing in all directions against the sides of the pipes. This is what happens to the blood in the arteries if you have high blood pressure and puts an extra strain on the heart.
- When blood pressure rises the blood travelling along the arteries roughens the lining of the arteries. To understand why this happens, picture what occurs when you turn a tap on. At normal pressure the water travels in a straight line, but when you turn the tap on full blast the water spurts out in all directions. Before it comes out it has been pushing in all directions against the sides of the pipes. This is what happens to the blood in the arteries if you have high blood pressure and puts an extra strain on the heart.
- Slide 5 Studies show that a multitude of diseases are attributable to hypertension. They include: • Heart failure • Coronary heart disease • Myocardial infarction • Left ventricular hypertrophy and failure • Aortic aneurysm • Peripheral vascular disease • Retinopathy • Hypertensive encephalopathy • Chronic kidney failure • Cerebral hemorrhage • Stroke With so many diseases linked to hypertension, prompt and effective treatments have the potential to reduce many complications. Dustan HP, et al. Arch Intern Med 1996; 156:1926-1935.
- Postural Hypertension: is a fall in blood pressure that occurs when changing position from lying to sitting or from sitting to standing Postural=change in position Hypotension=fall in blood pressure to a low level A fall in blood pressure leads to a reduced blood supply to organs and muscles; this can cause a variety of symptoms: E.G Feeling dizzy Changes in vision such as blurring Feeling vague or muddled You may be asked to take a patients blood pressure lying down Some diabetic patients may suffer the symptoms of postural hypotension
- After discussing the ‘dynamics of circulation’ and ‘cardiovascular regulation mechanisms’, it will be worthwhile to know how these basic principles apply to circulation in various regions of the body.
- Because each organ in the body has its own unique set of requirements, special circulations within each organ have evolved with their own particular features and regulatory mechanisms. Especially for times of great stress to the body, each organ possesses circulatory adaptations that allow it to make the changes appropriate for causing minimal harm to the overall organism. Here, we focus on the circulations of the brain, heart, skeletal muscle, abdominal viscera, and skin. The blood fl ow to each tissue must meet the nutritional needs of that tissue’s parenchymal cells while at the same time allowing those cells to play their role in the homeostasis of the whole individual. The way in which the circulatory system distributes blood fl ow must be fl exible so that changing demands can be met. In the process of meeting these demands, the body makes compromises. Consider the circulatory changes that accompany exercise. Blood fl ow to active skeletal muscle increases tremendously through both an increase and a redistribution of cardiac output. Blood fl ow to the coronary circulation must also rise to meet the demands of exercise. Furthermore, to dispose of the heat generated during exercise, the vessels in the skin dilate, thereby promoting heat transfer to the environment. As cardiac output is increasingly directed to active muscle and skin, circulation to the splanchnic and renal circulations decreases while blood fl ow to the brain is preserved. This chapter focuses on the perfusion of select systemic vascular beds, but keep in mind that the lungs receiv
- There are four cerebral arteries. The largest are the two internal carotid arteries, the left and right branches of the common carotid arteries in the neck which enter the skull, as opposed to the external carotid branches which supply the facial tissues. The two smaller arteries are the vertebral arteries, which branch from the subclavian arteries which primarily supply the shoulders, lateral chest and arms. Within the cranium, which houses the brain, the two vertebral arteries fuse into the basilar artery, which is located underneath, and primarily supplies, the brainstem. Both internal carotid arteries, within and along the floor of the cerebral vault, are interconnected via the anterior communicating artery. Additionally, both internal carotid arteries are interconnected with the basilar artery via bilateral posterior communicating arteries. The Circle of Willis, long considered to be an important anatomic vascular formation, provides backup circulation to the brain. In case one of the supply arteries is occluded, the Circle of Willis provides interconnections between the internal carotid arteries and basilar artery along the floor of the cerebral vault, providing blood to tissues that would otherwise become ischemic.