tmj
- 2. • INTRODUCTION • DEVELOPMENT • GROWTH • PARTS OF TMJ • BLOOD SUPPLY • INNERVATION • LYMPHATICS • TMJ IN FUNCTION • TMJ IMAGING • DEVELOPMENTAL ANOMALIES • TMJ DISORDERS AND MANAGEMENT • CLINICAL IMPLICATIONS • REFERENCES
- 3. INTRODUCTION • The TMJ is one of the most complex joints in the body. It is the area where the mandible articulates with the cranium. • It is considered to be a GINGLYMOARTHRODIAL JOINT. Ginglymoid- hinging Arthrodial- gliding. COMPOUND JOINT- 3 bones SYNOVIAL JOINT. • Growth center present within the joint capsule.
- 4. DEVELOPMENT • Meckel’s cartilage provides the skeletal support for development of the lower jaw. • Extends from the midline - backwards and dorsally; terminates as the malleus.(Articulare) • It articulates with the incal cartilage; thus early jaw movement occurs between these 2 cartilages. • This primary jaw joint exists for 4 months until ossification.
- 5. • The first evidence of joint development is seen at 3 months. • Here the 2 condensations TEMPORAL CONDYLAR • The temporal blastema - 1st to appear - separated from condylar blastema by some distance. • The condylar blastema’s rapid growth, in the dorsolateral direction - reduces the gap - band of uncondensed mesenchyme persists. (Form in the mesenchyme lateral to the primary joint.)
- 6. • Membranous ossification center appears in the middle of the temporal blastema. appearance of a cleft immediately above the condylar condensation cartilage appears in the condylar blastema to form the condylar growth cartilage. • Second cleft appears below the bone forming in the temporal blastema- creating upper joint cavity.
- 7. GROWTH OF TMJ • Neonatal tmj. • Tmj adopts it’s general postnasal form and composition around 12th week in utero. • At birth, the entire masticatory complex - skeletal structures and musculature - diminutive relative to craniofacial complex. • Condyle – immature small in size and essentially rounded.
- 8. • Temporal component- essentially flat- with very small manidibular fossa. • Articular disk is prominent – uniform thickness- conforms to flat temporal joint. • Mandibular condyle is highly vascular throughout the cartilage layers- Active proliferation and maturation.
- 9. • Changes in the temporal component of tmj – (birth to end of mixed dentition) • By 8 months - articular surface shows enlargement of the eminence and post-glenoid region. • 2.5 years - increase in size of articular eminence from 2mm to 5mm. • Temporal component achieves a s-shape; para sagittal. Contributed by articular eminence, fossa, post - glenoid process. • Early mixed dentition 6-7yrs - condyle thickens and cartilage thins
- 10. • Articular disk- highly vascularised- rich in fibroblasts- first few years of life. • After which- central part becomes avascular - less cellular.
- 11. • Adult Tmj - complete replacement of cartilage by bone- by 4th decade. • 5th decade - deeper articular fossa - growing eminence. • There is flattening of eminence in partial or complete edentulous states.
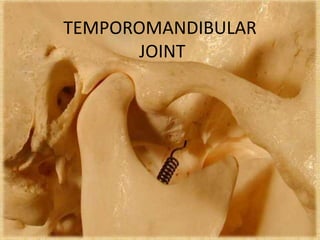
- 12. Parts of tmj bony GLENOID FOSSA CONDYLE ARTICULAR EMINENCE Soft tissue ARTICULAR DISC CAPSULE LIGAMENTS
- 13. Articular fossa /glenoid fossa Articular eminence ; An anterior protuberance continuous with the fossa The condylar process - rests within the fossa Articular Disc: divides articular compartment into upper and lower spaces The articular capsule envelopes the above structures. The lateral and accessory ligaments protect the joint.
- 14. • Laterally-root of zygomatic process. • Medially -spine of sphenoid- anteriorly foms the articular eminence. • Posteriorly-separated by sqaumo tympanic and petrotympanic fissures, from tympanic plate. • Superiorly -separated form middle cranial fossa by a thin plate of bone at apex. Glenoid fossa
- 15. • Glenoid fossa posterior margin- defined by lateral post glenoid process-continues medially as a post glenoid ridge in the tympanic plate. • The median glenoid plane defines the medial and the anteromedial boundary of the articular area. • Between the zygomatic root and median glenoid plane there is an extension of the articular surface, anterior to the crest of the articular slope- the pre-glenoid plane.
- 16. Articular eminence • A transversely elliptical region, sinuously curved in the sagittal plane- tilted forwards at 25 degrees to the occlusal plane. • Forms most of the articular surface of the fossa. • Variable steepness ; flatter in edentulous. • Anterior limit is the summit of the articular eminence which is a transverse ridge that extends as far as articular tubercle.
- 17. Condyle • Articular surface of the mandible represented by the mandibular condyle. • 15-20mm long; 8-120mm thick • Articulating surface strongly convex; anteroposterior and mediolateral(elongated): thus has 2 poles • Lateral pole: more pointed and does not extend far beyond the lateral surface of mandible. • Medial pole: projects further medially; thicker smoother more rounded.
- 18. Articular disc • Transversely oval-predominantly dense fibrous connective tissue. • Divides the joint cavity into 2 compartments. • Thick margin forming peripheral annulus; central depression holds articular surface of condyle. • Lower surface convex; concavo- convex upper surface. • Upper surface: thickened posteriorly and anteriorly, delimits a central thinner component.
- 19. In the sagittal section • Disc appears to posses a thin intermediate zone – thickened anterior & posterior bands. • Upper surface concavo- convex- fits against convex articular eminence and concave articular fossa. Posteriorly disc attached to loose vascular and nervous tissue- splits into 2 laminae. UPPER & LOWER
- 20. • Upper lamina - fibroelastic tissue - attached to squamotympanic fissure • Lower lamina - fibrous non elastic tissue - attached to back of condyle. • The bilaminar region consists of venous plexus - central part avascular. • Space between the two – filled with loose highly vascular connective tissue Upper lamina- Lower lamina
- 21. • Type I collagen comprise the disk – loosely arranged and poorly oriented- central region tightly bound, more organized. • Crimped nature of collagen – serves to absorb energy when sudden tensile force is applied. • Protects the disc from potential rupture.
- 22. Cells in the disc secrete chondroitin sulphate- heavily concentrated in central portion. Gives the disc resilience and compressive strength.
- 23. Functions of articular disc. • Helps stabilize tmj. • Acts as a shock absorber. • Shape and thickness - governed by muscle forces controlling position of mandible and condyle • It reduces wear. Frictional wear is halved by separating sliding and rotating movements .
- 24. Synovial membrane • Lines the inner surface of the capsule - relatively delicate. • Finger like projections – villi - anterior and posterior limits of the joint • Consists of 2 layers: cellular intima which rests on vascular subintimal layer.
- 25. • Subintimal layer – loose connective tissue – blood vessels, scattered fibroblasts, macrophages, mast and fat cells & elastic fibers. • Intimal layer - 2 types of cells – type A(macrophage like) & type B(fibroblast like). Type A : phagocytic, have filopodia Type B : Adds protein to fluid & synthesize hyaluronate
- 26. Synovial fluid • Filtrate of plasma- contains protein and sodium hyaluronate- • Total volume- 1ml • A non-newtonian fluid i.e decreased viscosity with increased shear rate’. • May also fulfill metabolic needs of avascular fibrous tissue of joint.
- 28. Capsule • Fibrous- surrounds the joint- extends from margin of glenoid fossa, including articular eminence (anteriorly), envelopes head of the condyle • Fuses inferiorly with the periosteum of the condylar process. • It encloses- a joint cavity- divided into 2 compartments by a fibrous disk.
- 29. • Origin – temporal - petrosquamosal and squamotympanic fisure; • Posteriorly - medial and lateral margins of the glenoid fossa • Anteriorly - periosteum of the anterior slope of the articular eminence. Here the capsule is lax up to the margins of the disk. From here it moves downwards (taut) - fuses with periosteum of condylar process.
- 30. Temporomandibular ligament • Also called lateral ligament • broad fan shaped – reinforcement of lateral wall of capsule. • Has two parts outer and inner surface • Outer surface-oblique arises from articular eminence- extends downwards and backwards attaches to outer surface of neck of condyle. • Inner horizontal portion (same origin)- inserts into lateral pole of the condyle and lateral margin of disk
- 31. • Prevents lateral dislocation thus also prevents medial dislocation of the opposite side. • Oblique portion limits inferior displacement and horizontal portion limits posterior displacement of condyle.
- 32. Sphenomandibular ligament •Medial to and separate from the capsule. •A flat thin band descends from the spine of sphenoid-widens reaching lingula. Fibers attach to the anterior malleolar process. •Lateral : Lateral pterygoid and Auriculotemporal nerve. • Upper end: Chorda tympani • Inferomedial: Medial pterygoid
- 33. Stylomandibular ligament • Thickened band of deep cervical fascia -stretches from the apex ,adjacent to the anterior aspect of styloid process-to the angle & posterior border of mandible. • Cannot mechanically constrain any normal mandibular movements.
- 34. Blood supply • Superficial temporal artery laterally and anterior tympanic branch of maxillary artery medially( terminal brch of ECA). • Venous drainage – retromandibular vein- anterior aspect -plexus around lateral pterygoid • Posteriorly – vascular region that separates 2 laminae of the retrodiscal tissue.
- 35. • Auriculotemporal and massetric nerves; mandibular division of trigeminal nerve. • Postganglionic sympathetic nerves- tissue associated with the capsular ligament & bilaminar disc
- 36. Lymphatic drainage • Drain into the upper deep cervical lymph nodes around IJV.
- 37. Tmj in Function Functional elements Glenoid fossa;Posterior surface of articular eminence. Entire superior surface of Condylar head. Capsule and ligament. Articular disc. Non functional element Glenoid fossa; posterior half, attachment to superior layer of lamina.
- 38. Jaw movements During mouth opening- incisors separated upto 50-60mm- 35˚ rotation. Adult range of movements- 10y (F) 15y(M).
- 39. Protruders Retractors Elevators Depressors Lateral movers Lateral & medial pterygoids Temporalis,digastric geniohyoid Temporalis,masseter medial pterygoid Lateral pteygoid, digastric, geniohyoid, mylohoid Medial & lateral pterygoids
- 40. Movements of condyle • Major function of mandible- exerts force to break down food. • Pure vertical movements - ineffective in breaking tough fibrous food. • Lateral movements - create a shear component- enhances power stroke of mastication. • Extensive lateral movements - jaw rotated about one condyle-other condyle slide backward and forward. • Sliding movement - capsular ligament around upper joint is loose- tight around lower compartment.
- 41. • 3 phases in symmetrical opening: • Early phase- controlled by temporomandibular ligament and articular eminence • Short middle phase- constriction of movements by Temperomandibular ligament & Sphenomandibular ligament. • Late phase: controlled by sphenomandibular ligament and articular eminence.
- 42. Imaging • Hard Tissue • Panoramic projection • Lateral tanscranial view • Transpharyngeal view • Antero-posterior projection • Tomography. • Soft Tissue. • Arthrography. • CT scan. • MRI.
- 45. • Various terms have been used to describe disturbances of the masticatory system. • 1934 James costen described group of symptoms centering around ear and TMJ- Costen syndrome. • 1959 Shore introduced TMJ Dysfunction • Ash & Ramfjord- functional TMJ disturbances Terminology
- 46. • Limited nature of these terms lead to a broader term- Craniomandibular disorders. • Bell coined the term Temporomandibular disorders. • Describes both problems associated with the joint & disturbances associated with function of masticatory system.
- 47. Activities of system/ function • Chewing, clenching • Speaking, grinding • Swallowing • Influenced by peripheral input - inhibitory • Influenced by CNS • excitatory Functional Parafunctional
- 48. Etiologic considerations for TMD. • 5 major factors associated with TMD 1. Occlusal condition: 2. Trauma 3. Emotional stress 4. Deep pain input 5. Para-functional activities.
- 49. Occlusal condition • Excessive load on the system due to orthopedic instability may lead to intracapsular disorders. • 2 factors that determine it are: degree of instability and amount of loading. • Changes can be acute/ sudden or chronic.
- 50. • Chronic interference affects functional activity by altering muscle; • avoids potentially damaging contact and gets on with task of function
- 51. Trauma • Macro and micro • Macro: sudden force that can result in structural alterations. Eg blow to face. • Micro : small force applied repeatedly to structures over a long periods. Bruxism/ clenching.
- 52. Deep pain input. • Centrally excites a brainstem – produces muscle response- protective co-contraction. (body’s response to injury or threat of it.) • Functional disorders of masticatory system • 2 symptoms: Pain and dysfunction.
- 54. I. Masticatory muscle disorders a. Protective co-contraction b. Local muscle soreness c. Myofacial pain d. Myospasm e. Centrally mediated myalgia
- 55. II. Temporomandibular joint disorders 1. Derangement of condyle - disc complex a. Disc displacements b. Disc dislocations with reduction c. Disc dislocations without reduction 2. Structural incompatibility of articular disc a. Deviation in form - Disc - Condyle - Fossa b. Adhesions i. Disc to condyle ii. Disc to fossa c. Subluxation d. Spontaneous dislocation 3. Inflammatory disorders of TMJ a. Synovitis/ Capsulitis b. Retrodiscitis c. Arthritides i. Osteoarthritis ii. Osteoarthrosis iii. Polyarthritides d. Inflammatory disorders of associated structures i. Temporal tendonitis ii. Stylomandibular ligament inflammation.
- 56. III. Chronic mandibular hypomobility 1. Ankylosis a. Fibrous b. Bony 2. Muscle contracture a. Mystatic b. Myofibrotic 3. Coronoid impedance IV. Growth disorders 1. Congenital and develpmental bone disoredrs a. Agenesis b. Hypoplasia c. Hyperplasia d. Neoplasia 2. Congenital and develpmental bone disoredrs a. hypothrophy b. Hypertrpohy c. Neoplasis
- 57. • Conservative reversible therapy. • Counsel • Exercise • Physical therapy • Medications • Appliances • Selective Grinding • Bio-feed Back • TENS • Non conservative irreversible therapy. • High Condylectomy • Meniscectomy • Disectomy • Orthodontic surgery • High Condylotomy • Hyaluronic acid • Reconstruction • Arthrocentisis Long term studies for TMD treatment have given 2 kinds of approaches ;
- 58. • All treatment methods can be categorized generally into ; • Definitive treatment / supportive treatment.
- 59. Definitive treatment • Occlusal conditions- occlusal therapy- • Reversible-stabilization appliance • Irreversible – selective grinding, restorative procedures. • Emotional Stress: Restrictive use, Voluntary avoidance, Relaxation therapy. • Trauma- microtrauma- curtail it.
- 60. Supportive therapy • Directed toward the reduction of pain and dysfunction. • Pharmacologic or Physical therapy. • Pharmacologic: 1. Analgesics 2. NSAIDs 3. Corticosteroids 4. Anxiolytics 5. Muscle relaxants 6. Antidepressants.
- 61. • Physical therapy. Group of supportive actions, usually instituted as an adjunct to definitive treatment. 2 types- Modalities & Manual techniques • Modalities: Thermotherapy, Coolant, ultrasound, phonophoresis, iontophoresis, TENS, laser • Manual techniques: provided by physical therapist; 3 types- soft tissue & joint mobilization, muscle conditioning.
- 62. Local muscle soreness • Or non-inflammatory myalgia- myogenos pain disorder. • First response of muscle tissue to continued protective co-contraction. • Cause • Protracted protective co-contraction • Local tissue trauma • Increased emotional stress.
- 63. • History • Pain began several hours or days after event - associated with tissue injury. • Clinical characteristics 1.Marked decrease in the velocity and ROM 2.Minimum pain at rest. 3.Pain increased with function. 4.Local tenderness when palpated.
- 64. • Definitive treatment • As it produces deep pain; primary goal is to decrease sensory input to CNS. • Supportive therapy • Pain reduction; NSAIDS etc • Relaxation techniques • Muscle stretching and massage
- 65. Myospasm • Cause: 1. Continued deep pain input 2. Local metabolic factors- leads to fatigue. 3. Idiopathic History: sudden onset; restricted movement ; rigidity
- 66. • Clinical characteristics 1.Marked decrease in the velocity and ROM 2.Minimum pain at rest. 3.Pain increased with function. 4.Local tenderness when palpated.
- 67. Treatment 1. Reducing the pain- passive strecthing of muscle. 2. Manual massage, vapocolant spray, ice etc. 3. In case of remission: botulinum toxin A- neurotoxin – irreversible presynaptic blockade of Ach at motor end plates.
- 68. Disc displacements and disc dislocations with reduction • Cause: • Result from elongation of the capsular and discal ligaments, coupled with thinning of articular disc. • Due to macro or micro trauma. • Micro trauma e.g. Bruxism, class II div 2 ,prolonged excessive loading- breakdown
- 69. • Clinical features. 1.Relatively normal ROM, restricted with pain. 2.Discal movements felt on palpation of joints • Treatment 1. To re-establish normal condyle – disc displacement. 2. Done using anterior positioning appliance- provides occlusal relationship that maintains mandible in a forward position- least protruded position.(farrar 1970).
- 70. Dislocation without reduction • Disc dislocated anteromedially from condyle does not return to normal position with condylar movement. • Macro/ microtrauma most common causes • Features: limited ROM (25-30mm)- normal eccentric movement to ipsilateral side & restricted ecccentric movement to contralateral side .
- 71. • Treatment: 1.Anterior positioning appliance contraindicated 2.Manual manipulation for disc recapture.
- 72. Subluxation • Also called hypermobility • Clinical description of condyle as it moves anterior to crest of articular eminence. • Cause: result of anatomic form of fossa; steep short poterior slope of eminence- longer flat anterior slope. • Results when disc is maximally rotated on condyle before full translation.
- 73. • History- patient reports a locking sensation when ever mouth is opened too widely. Sudden jump of condyle forward with a ‘thud’ sensation. • Treatment – Eminectomy- reducing steepness of eminence.
- 75. Spontaneous Dislocation • Also referred to as open lock; occurs after wide opening; spontaneous dislocation of both the condyle and disc. • History: patient arrives at office with mouth open unable to close- following yawn or wide opening; • Features: patient remains in a wide open position
- 76. Condyle in normal position Condyle after dislocation
- 77. • Treatment: directed towards increasing the disc space, allows retrodiscal lamina to retract disc. • Also applying slight posterior pressure to chin while the patient is opening wide; reduces dislocation
- 78. Ankylosis • Abnormal immobility of the joint. • Two types fibrous and bony • Fibrous - occurs between condyle and disc disc and fossa • Bony - condyle and fossa.
- 80. • Cause: most commonly- hemarthrosis secondary to trauma. • Fibrous ankylosis- continued progression of joint adhesions- also chronic inflammation aggravates the condition.
- 81. • Features: condyle can still rotate- some degree of restriction on inferior surface of disc. • Patient unable to open 25mm interincisally; lateral movements restricted. Path of opening toward ipsilateral side • Treatment: surgery only definitive treatment in case of loss of function.
- 82. Clinical criteria for Temporomandibular disorders: • Motion: • Limitation • Deviation • Tenderness • Joint noise: • Examination : Listening Palpation (over the TMJ or inside the auditory canal) or asking the patient. • Additional means - chewing a wax or gum. Noise: Clicking (Popping) Crepitus
- 87. • Range of motion • 1- Active Range Of Motion (AROM): It’s the opening under voluntary effort , it is measured by the distance between upper central incisors and lower central incisors. • Normal…………………>40 mm • Restricted……………. Male if less than 35 mm. Female if less than 30 mm. • Excessive……… it should be considered normal except when there is a history of locking or there is a pain or discomfort during opening that interfere with normal function • 2-Passive Range Of Motion (PROM) : +(2-3mm)
- 88. • Deviation • As the both sides are not affected to the same extend usually deviation occurs toward the affected side.
- 89. • Clicking (popping) • Reproducible: reproducible opening or reproducible closing • Reciprocal: In both opening and closing • Repetitive: At exact same position • Clicking suggests disc disorder • Crepitus • Fine crepitus: weak grating sound suggests mild bone to bone contact • Coarse crepitus: strong grating sound suggests gross bone on bone contact. • Crepitus suggests degenerative joint disease
- 90. Developmental anomalies • ANOMALIES OF THE MANDIBLE AND THE TMJ; • Hypoplasia • Hyperplasia • Dysplasia / dysmorphia • Deformation • Postembryonic anomalies
- 91. • Micrognathia- describes an abnormally small mandible. • Many anomalies have this as one of their features. • Cause: occurs due to deficiency in the amount of available mesenchyme during the formation; due to earlier destruction or absence of undifferentiated cells. Deficiency is always bilateral and symmetrical. • Many craniofacial anomalies include hypoplasia; normal but small mandible; often with an abnormality of TMJ.
- 92. • Hallerman strieff syndrome, Pierre Robin syndrome, and Treacher Collins syndrome. • Hallermann Strieff Syndrome: includes a number of facial defects involving the eyes, nose, maxilla and mandible giving a distinct facial appearance. • Features: Small mandible particularly the condyles, and forward positioning of the condyle out of a poorly formed fossa is characteristic. • Positioning partly postural to improve airway; regularity and symmetry of the condition suggests a reduction in mesenchyme at an early embryonic stage.
- 93. • Pierre robin syndrome; recently referred to as Robin sequence; Small mandible an essential feature; also one of the causes of associated cleft palate; more generalised hypoplasia involving facial and masticatory muscles, maxilla, mandible and palate; thus wide spread deficiency of mesenchyme. • Treacher collins syndrome: dysplastic anomalies of eye, zygomatic arch, temporal bone, ear and mandible; produces a distinct facial appearance. • Small mandible including condyle; unusual TMJ relations; condyle positioned posteriorly and inferiorly in close relation with the external auditory canal . • This may be related to the abnormal muscle balance in this condition; or anomaly of the capsule as an unusual discomalleolar ligament. Treacher collins
- 94. • Excessive size of the mandible is termed mandibular prognathism. • Usual criteria for estimating prognathism is the amount of anterior protrusion of the chin; length of the mandible from condyle to symphysis. • Unilateral hyperplasia is limited to the condyle, larger than the unaffected side. • Another form of unilateral hypertrophy is part of a generalized hemihypertrophy involving many facial structures and the entire mandible. Tmj on the affected side is positioned far anterior to the external auditory canal accounting for midline deviation.
- 95. • Dysmorphia- group of anomalies characterized by partial or complete agenesis or malformation of parts of the TMJ. • Agnathia, complete or nearly complete absence of the mandible and hyoid bone with other branchial arch defects . Due to failure of neural crest cells to enter face. • Orofacial digital syndrome( Type II)- includes absence of the symphysis(cleft mandible), cleft of lower lip and macroglosssia, ODS(type I) less sever form. • Dyspalsias of the TMJ belong to the group of anomalies most commonly termed hemifacial microsomia(also termed Lateral facial Dysplasias). • Features: Complete agenesis of the TMJ, also affects ramus, condyle, muscle of mastication etc.
- 96. • Biomechanics of the movement of mandible takes place with the changes associated with in the TMJ. • Usual function never exceeds the integrity or adaptive limits of the masticatory system. • Any function which exceeds this limit causes acute or chronic trauma on the masticatory system. Clinical implications
- 97. • Acute – Subluxation – Dislocation – Trauma – Displacement of the articular disk • Chronic – Bruxism – Occlusal disharmony – Intercapsular disorders
- 98. • Even and simultaneous contacts on all teeth during centric closure – distributes forces on all teeth equally. • During centric closure canine or anterior guidance is desirable – reduces the ability of elevator muscles to contract – transfers the movement onto the anterior teeth – class III lever system – resulting in anterior teeth receiving only 1/9th the force.
- 99. • Anterior guidance needs to be in harmony with the patient’s neuromuscular envelope of function. • The occlusion should have a definite vertical dimension. Alteration lengthens the pterygomassetric sling beyond its ability to adapt causing muscular spasms • Force management should be considered while treating mobile teeth.
- 100. REFERENCES • Management of temporomandibular disorders and occlusion: 5th edition; Jeffrey P. Okeson • Oral Radiology; Principles & interpretation; White & Pharaoh; 4th Edition. • Clinical periodontology 10th edition Carranza • Gray’s anatomy: anatomical basis of clinical practice: 39th edition. • The anatomical basis of dentistry: Bernard Liebott: 2nd edition • Oral histology: Development, structure and function: Tencate; 5th edition
- 101. THANK YOU