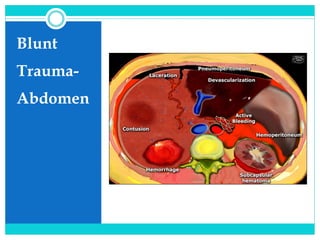
Blunt trauma abdomen
- 3. DR ISHA DESHMUKH ASSISTANT PROFESSOR PEDIATRIC DEPARTMENT BJGMC MUMBAI APPROACH TO BLUNT TRAUMA ABDOMEN
- 4. Introduction Following the head and extremities, the abdomen is the third most commonly injured anatomic region in children. Abdominal trauma can be associated with significant morbidity & may have a mortality rate as high as 8.5%. The abdomen is the most common site of initially unrecognized fatal injury in traumatized children. Children can lose up to 45% of their total blood volume before showing any changes in blood pressure.
- 5. Anatomical Considerations: Solid Organs: proportionally larger & more anterior Kidneys: larger, more mobile +/- foetal lobulations Subcutaneous Fat: ↓ Abdominal Musculature: ↓ AP Diameter: ↓ Flexible Cartilaginous Ribcage The intestine is not fully attached within the peritoneal cavity (especially the sigmoid and right colon) more vulnerable to injury due to sudden deceleration and/or abdominal compression. The bladder extends to the level of the umbilicus at birth and therefore is more exposed to a direct impact to the lower abdomen.
- 6. Key points…… Liver/spleen more anterior and less protected by ribs/muscles Kidney more mobile and less protected by ribs/muscles Solid organ bleeding tends to stop because kids have excellent vasoconstrictive response Pitfall of hypotension: kids can lose 30-40% of circulating blood volume and still maintain normal blood pressure so don’t wait for hypotension to diagnose shock. CRT>2-3 seconds; cool skin Low urine output Altered mental status Elevated heart rate/narrowed pulse pressure Lactate>3-4
- 7. Common injury patterns Solid organ injury Laceration to liver, spleen, or kidney Injury to one of these three + hemodynamic instability: considered indication for urgent laparotomy Isolated solid organ injury in hemodynamically stable patient: can often be managed nonoperatively. Pelvic fractures: Suggest major force applied to patient. Usually MVA Significant association with intraperitoneal and retroperitoneal organs and vascular structures.
- 8. Physical Examination Observation of external signs Palpation for tenderness, distension or guarding Swallowing of air pain & crying NGT decompression UQ ecchymosis , tenderness, and associated rib fractures suggest liver / splenic injuries Mid-abdominal ecchymosis from a seat belt small bowel injury Localized suprapubic tenderness extraperitoneal bladder rupture Generalized abdominal distension intraperitoneal bladder rupture.
- 9. Assessment Inspection, auscultation, percussion, palpation Inspection: abrasions, contusions, lacerations, deformity Auscultation: careful exam advised by ATLS. (Controversial utility in trauma setting.) Percussion: subtle signs of peritonitis; tympany in gastric dilatation or free air; dullness with hemoperitoneum Palpation: elicit superficial, deep, or rebound tenderness; involuntary muscle guarding
- 10. Physical Exam: Eponyms Grey-Turner sign: Bluish discoloration of lower flanks, lower back; associated with retroperitoneal bleeding of pancreas, kidney, or pelvic fracture. Cullen sign: Bluish discoloration around umbilicus, indicates peritoneal bleeding, often pancreatic hemorrhage. Kehr sign: L shoulder pain while supine; caused by diaphragmatic irritation (splenic injury, free air, intra-abd bleeding) Balance sign: Dull percussion in LUQ. Sign of splenic injury; blood accumulating in subcapsular or extracapsular spleen.
- 11. Laboratory Tests CBC – Hb Serum biochemistry Serum amylase levels / lipase levels – Pancreatic / bowel trauma Liver transaminases - Liver injury Coagulation profile Urine analysis – hematuria Base deficit > 6 meq/L intra-abdominal injury
- 12. Investigations FAST X-Ray Chest & Abdomen USG CT Scan Paracentasis Diagnostic Peritoneal Lavage Diagnostic Laparoscopy
- 13. Radiographic Assessment Radiology survey – Chest, abdomen, pelvis, cervical spine CT – procedure of choice If patient is unstable management CT – most accurate to grade the extent of injury Ultrasonography (US) is rapid, noninvasive, and relatively inexpensive.
- 14. Plain X-Ray Chest & Abdomen Pneumotharax, Haemothorax Free air under diaphragm Bowel loops in the chest Elevation of the both /Single diaphragm Lower Ribs # -Liver /Spleen Injury Ground Glass Appearance – Massive Hemoperitoneum Obliteration of Psoas Shadow –Retroperitoneal Bleeding #vertebra
- 15. Focused Assessment with Sonography in Trauma (FAST) First used in 1996 Rapid , Accurate Sensitivity 86- 99% Can detect 100 mL of blood Cost effective Four different views- Pericardiac Perihepatic Perisplenic Peripelvic space Eliminates unnecessary CT scans Helps in management plan
- 16. FAST: Accuracy For identifying hemoperitoneum in blunt abdominal trauma: Sensitivity 76 - 90% Specificity 95 - 100% The larger the hemoperitoneum, the higher the sensitivity. So sensitivity increases for clinically significant hemoperitoneum. How much fluid can FAST detect? 250 cc total 100 cc in Morison’s pouch
- 17. FAST: Strengths and Limitations Strengths Rapid (~2 mins) Portable Inexpensive Technically simple, easy to train (studies show competence can be achieved after ~30 studies) Can be performed serially Useful for guiding triage decisions in trauma patients Limitations Does not typically identify source of bleeding, or detect injuries that do not cause hemoperitoneum Requires extensive training to assess parenchyma reliably Limited in detecting <250 cc intraperitoneal fluid Particularly poor at detecting bowel and mesentery damage (44% sensitivity) Difficult to assess retroperitoneum Limited by habitus in obese patients
- 18. USG Advantage Easy & Early to Diagnose Noninvasive No Radiation Exposure Resuscitation/Emergency room Used in initial Evaluation Low cost Disadvantage Examiner Dependent Obesity Gas interposition Low Sensitivity for free fluid less 500 mL False –Negative retroperitoneal & Hallow viscus injury
- 19. CT EAST level I recommendations (2001): CT is recommended for evaluation of hemodynamically stable patients with equivocal findings on physical examination, associated neurologic injury, or multiple extra-abdominal injuries. CT is the diagnostic modality of choice for nonoperative management of solid visceral injuries.
- 21. DPL - Diagnostic Peritoneal Lavage Diagnostic peritoneal lavage is sensitive for the detection of intra-abdominal injury that results in hemoperitoneum , but it is rarely performed in pediatric patients. In one series, the cell count, amylase activity and particulate matter in DPL specimen were able to identify small bowel perforation with a sensitivity of 100%. Difficult to perform – small abdomen
- 23. Diagnostic Peritoneal Lavage 98% sensitive for intraperitoneal bleeding (ATLS) Open or closed (Seldinger); usually infraumbilical . Free aspiration of blood, GI contents, or bile in hemodynamically abnormal pt: indication for laparotomy If gross blood (> 10 mL) or GI contents not aspirated, perform lavage with 1000 mL warmed RL. + test: >100,000 RBC/mm3, >500 WBC/mm3, Gram stain with bacteria. Alters subsequent examination of patient
- 24. Diagnostic Laparoscopy Diagnostic video-assisted laparoscopic evaluation – safe and effective modality for evaluating the abdomen. Diaphragmatic injuries – diagnosed & repaired laparascopically Alternative – thoracoscopy for thoracic & abdomen injury in penetrating trauma.
- 25. Prehospital Care The goal of prehospital is to deliver the pt to hospital for definitive care as rapidly as possible. ‘Scoop and Run’ Maintain airway & start I V line Care of spinal cord Communicate to medical control Rapid transport of patient to trauma centre
- 26. Initial Assessment and Resuscitation Primary survey Identification & treatment of life threatening conditions Airway , with cervical spine precautions Breathing Circulation Disability Exposure
- 29. ATLS
- 32. EAST Algorithm: Unstable Eastern Association for the Surgery of Trauma, 2001
- 33. EAST Algorithm: Stable Eastern Association for the Surgery of Trauma, 2001
- 36. Solid Organ Injuries Grading of injured solid organs such as Spleen, Liver & Kidneys are on the basis of subcapsular hematoma ,capsular tear, parenchymal lacerations & avulsion of vascular pedicle Bleeds significantly & cause rapid blood loss Difficult to identify injury by physical exam Repeated assessment is required to make the diagnosis Slowly oozing blood into peritoneal cavity
- 38. Splenic Injury Most common intra- abdominal organ to injured (40-55%) 20% of splenic injuries due to left lower rib fractures Commonly arterial hemorrhage Conservative management : -Hemodynamic stability -Preserved vasculature - Absence of other indication of Laprotomy -Grade 1to 3 (Subcapsular Hematoma ,Laceration <3 cm) Monitoring Serial abdo. Examinations & Haematocrit are essential Success rate of conservative m/m is >80%
- 40. Splenic Injuries Capsular tears (I)- Compression & topical haemostatic agent Deep Laceration (II)- Horizontal mattress suture or Splenorrhaphy Major Laceration not involving hilum (IV)- Partial Splenectomy Hillar injury (V)–Total Splenectomy Grade IV-V: almost invariably require operative intervention Success rate of Splenic salvage procedure is 40-60%
- 41. Liver Injury Second most commonly injured organ Highest mortality Clinical course of patient determines treatment Late complications – bile peritonitis, abscess formation, hemorrhage Operative treatment – hepatic vein trauma Damage control surgery – packing, stabilization, followed by repeat laparatomy Embolization of hepatic vessels – ongoing blood loss
- 42. Lacerations (most common in posterior segment of right lobe at ligament attachment), hematoma, vascular injury Hemoperitoneum 2/3 of the time Grading systems not useful for operative decision-making. Management based on patient’s clinical status not CT. CT helps with level of care, duration of stay, duration of activity restriction at discharge 1-3% operative management Active extravasation (contrast blush on CT) NOT an absolute indication
- 43. Renal Injury Clinically not suspected & frequently overlooked Mechanism: Blunt , Penetrating # lower ribs or spinous process, Crush abdominal Pelvic injury Direct blow to flank or back Fall MVA
- 44. Renal Injury Diagnosis 1.History ,Clinical examination 2. Presentation :Shock, hematuria & pain 3. Urine: gross or microscopic hematuria 5.X-ray KUB, IVP 6.USG 7.CT Scan abdomen 8.Radionuclide Scan The degree of hematuria may not predict the severity of renal injury
- 45. Kidney Injury… Rarely isolated injury Mechanism: Direct blow: parenchymal contusion or hematoma; see delayed contrast enhancement on CT; mostly NOM Rapid deceleration: collecting system injury; mostly NOM if leakage confined to peri-renal space on delayed (10-15 min later) images Renal artery injury: urgent operative repair because loss of kidney function occurs within 2 hours.
- 46. Renal Injury . Classification of Injury Grade I : Contusion or Subcapsular Hematoma Grade II: Non Expanding Hematoma, <1 cm deep ,no extravasation Grade III: Laceration >1cm with urinary Extravasation Grade IV: Parenchymal Laceration deep to CM Junction Grade V: Renovascular injury
- 48. Management of Renal Injury About 85% of blunt renal trauma can be managed conservatively Renal Contusion : Conservatively Renal exploration : Indication Deep cortico-medullary Laceration with extravasation Large perinephric Hematoma Renovascular injury Uncontrolled bleeding Before Nephrectomy ,Contralateral Kidney should be assessed
- 49. Bladder Injury Commonly in BTA 70% of bladder Injury are associated with pelvic fracture . Hematuria Type 1.Extraperitoneal Rupture-by bony fragment 2. Intraperitoneal Rupture- at dome when blow in distended bladder Diagnosis -1. Clinical 2. Cystography T/t 1. Intraperitoneal –trans-peritoneal - closure +SPC 2:Extraperitoneal Rupture : Foley’s catheter -10 -14 days
- 50. Pancreatic Injury Uncommon injury Mechanism: compression against vertebra-->body injury; blow to flank-->tail injury CT: CT not great for evaluation; peri-pancreatic fluid, stranding, pancreatic enlargement Management controversial: small studies with increased rate of complications with NOM Mattix, J Pediatr Surg 2007: 26% failure rate of NOM; more pseudocyst formation if NOM with pancreatic ductal injury Higher failure risk: Multiple organ injury Greater injury severity Pancreatic injury-18% failure rate
- 51. Bowel Injury Jejunum most commonly injured CT findings: unexplained free fluid, wall thickening, dilated bowel loops, mesenteric fat stranding; free air or oral contrast extravasation (if given) infrequently seen with rupture Partial thickness tearhematoma Treatment: NOM, bowel rest; SBO can occur if large hematoma Full thickness tear/rupture repair Unexplained free fluid with normal PE: FF not as predictive of bowel injury in kids as in adults; consider serial exams