Managing Sudden Onset Eye Pain in Elderly Post-Cataract Surgery Patient
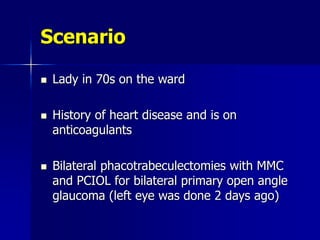
- 1. Scenario Lady in 70s on the ward History of heart disease and is on anticoagulants Bilateral phacotrabeculectomies with MMC and PCIOL for bilateral primary open angle glaucoma (left eye was done 2 days ago)
- 2. Called in the middle of the night because she has develped sudden onset of pain in left eye What possible diagnoses run through your mind? Are you going to examine her?
- 3. My differential diagnosis would include: Endophthalmitis/blebitis Uveitis Corneal surface problem Malignant glaucoma Iris bombe (pupil block) Raised IOP from other causes Delayed suprachoroidal haemorrhage Migraine Others
- 4. What diagnosis would you think if you saw this? What does the picture show?
- 6. The most feared intraoperative complication? Every surgeon needs to be prepared for it, to recognise it, and know what to do the instant it happens.
- 7. a.k.a and abbreviations Suprachoroidal haemorrhage (SCH) Massive suprachoroidal haemorrhage (MSCH) Expulsive choroidal haemorrhage (ECH)
- 8. WHAT IS IT? Large bleed into the suprachoroidal space which results in the extrusion of intraocular contents from the eye or apposition of retinal surfaces
- 9. Enucleated eye showing suprachoroidal and vitreous haemorrhage following ocular perforation SCH
- 10. HISTOPATHOLOGY of MASSIVE SCH Totally detached choroid and neural retina Gaping wound May see a ruptured ciliary artery
- 11. Retina in the AC and cornealscleral incision Hyphaema AN EYE WITH THAT HAD INTRAOPERATIVE EXPULSIVE SCH
- 12. Histopathology of same eye. Neuroretina is seen in the corneal wound. Optic nerve Surgical incision Blood clot Detached retina Detached retina Blood clot
- 13. Specimen of an eye that got SCH following rupture of a corneal ulcer SCH Prolapsed lens through cornea Detached retina
- 14. CLASSIFICATION
- 15. SOME HAVE ATTEMPTED TO PROVIDE A CLASSIFICATION Type 1 ECH : massive haemorrhage with expulsion of retinal tissue Type 2 ECH : vitreous loss and an abolished vitreous cavity Type 3 ECH : less extensive SCH with a partially preserved vitreous cavity
- 16. What was the classification again?
- 17. MORE SIMPLE CLASSIFICATION 1) EXPULSIVE : spontaneous nucleus expression with extrusion of ocular contents 2) NON-EXPULSIVE : SCH without loss of ocular contents
- 18. INCIDENCE OF SCH (old studies) 0.2% in cataract Sx 0.3% in PK Sx 0.7% with filtration surgery
- 19. PATHOGENESIS
- 20. Exact cause of spontaneous SCH is not known. Can get SCH after surgical instruments impact on the choroid. Although suprachoroidal effusion and SCH may precede the development of expulsive haemorrhage, the relationship remains unclear.
- 21. Source of bleeding seems to be ruptured long or short, posterior ciliary arteries. Thought to occur at the sight where the arteries make a right-angled turn crossing the suprachoroidal space from its scleral canal.
- 22. One theory is that sudden hypotony straightens the sclerotic vessel and causes the rupture.
- 23. Experiments on rabbits using anticoagulants to precipitate SCH have given another possible sequence of events:
- 24. Engorgement of the choriocapillaris Suprachoroidal effusion occurring mainly near the posterior pole Stretching and tearing of choroidal vessels and vessels at the ciliary body base Massive extravasation of blood, primarily from the torn vessels at the ciliary body base Expulsion of blood and intraocular contents through incision
- 26. SYSTEMIC Generalised arteriosclerosis Hypertension Diabetes mellitus Blood dyscrasias: – Polycythaemia – Haemophilia – thrombocytopenia Anticoagulants Advanced age
- 27. MANAGEMENT OF PATIENTS UNDERGOING CATARACT SURGERY ON ORAL ANTICOAGULANTS (N.Sargent, T.Keenan, 2008) Expected to be uncomplicated phaco LA/GA On admission: •Full consent by resident with documentation in notes •Check for phacodonesis and pupil dilates to >4mm •Resident to check INR is in therapeutic range: DVT prophylaxis 2.0 to 2.5 DVT or PE Rx 2.0 to 3 AF 2.0 to 3.0 Recurrent DVT or PE 3.0 to 4.0 Low risk prosthetic heart valves 2.0 to 3.0 High risk prosthetic heart valves 3.0 to 4.0 On listing for surgery: consultant or resident to give blood form for INR to be performed within 48 hours of Sx INR within therapeutic range?Yes No Inform surgeon straight away by phone: •Consider discharging and referring to treating doctors •Consider keeping in ward if INR too high whilst reducing warfarin (e.g. if from Gaza) •Consider surgery if INR below therapeutic range and if LA Proceed to surgery: •Subtenon/topical LA •Clear corneal incision
- 28. MANAGEMENT OF PATIENTS UNDERGOING CATARACT SURGERY ON ORAL ANTICOAGULANTS (N.Sargent, T.Keenan, 2008) ECCE or Phaco with high risk of needing to convert to ECCE (e.g. phacodonesis with small pupil and hard lens), trabeculectomy •Inform consultant surgeon straight away by phone. •Consider keeping in ward if INR too high whilst reducing warfarin (e.g. if from Gaza) Proceed to surgery: •Subtenon/topical LA •Clear corneal incision if possible Footnote *If therapeutic range for INR 3-4.0 (generally this is the case if fitted with an old- fashioned Starr-Edwards ‘ball-and-cage’ prosthetic mitral valve) •liase with anaesthetist. •Consider stopping warfarin and as soon INR below 3.0 commence heparin IV infusion. •Stop IV heparin 2-3 hours before surgery. On admission resident to check INR INR less than 3.0 ? (see footnote) Yes No
- 29. OCULAR I Glaucoma (including high preop IOP and history of 5-fluorouracil injections) Severe axial myopia Aphakia Previous vitrectomy
- 30. OCULAR II Previous multiple scleral buckling operations Dense brunescent nuclear sclerosis and ECCE Large incision used with nucleus expression extracapsular cataract extraction PK
- 32. OCULAR INTRAOPERATIVE FACTORS I Retrobulbar anaesthesia (increased resistance to venous outflow) Retrobulbar anaesthesia without adrenaline Sudden decrease in intraocular pressure
- 33. OCULAR INTRAOPERATIVE FACTORS II Vitreous loss Combining extracapsular extraction with a trabeculectomy Capsular bag phaco versus iris plane phaco (increased intraocular pressure swings)
- 34. SYSTEMIC Valsalva manoeuvre Coughing Sudden rise in systemic BP Elevated intraoperative pulse >85 bpm General anaesthesia
- 35. POSTOPERATIVE FACTORS - Wound leak - Ocular trauma - Valsalva manoeuvre
- 37. In an ECCE, typically occurs after lens delivery Progressive AC shallowing Loss of red reflex Red mound appearing in vitreous Increased IOP Gaping of wound Iris prolapse that will not reposit
- 38. This is followed by Vitreous extrusion Loss of red reflex Appearance of a dark mound behind the pupil Severe cases all intraocular contents maybe extruded through the incision
- 39. Suprachoroidal haemorrhage during PK Sx After expulsion of lens, retina and choroid in front of a bright red haemorrhage BEFORE: corneal button removed
- 40. MANAGEMENT
- 41. When you think about MANAGEMENT in exams, think about dividing into: 1) Preventative (pre- and intraoperative) measures 2) Intraoperative management 3) Post-operative management
- 42. PREVENTATIVE MEASURES Can divide again into: 1) Pre-op 2) Intra-op 3) Post-op
- 43. Checking INR levels if on anticoagulants. Avoid aspirin and other anticoagulants where possible, except routine phacos. Check BP, control systemic hypertension Cancel coughing patients or give cough suppressants Control excessively high IOP (consider diamox and mannitol on day of surgery) PREOPERATIVE MEASURES
- 44. Use minimal pre-op G.Phenylephrine to avoid systemic hypertension Do not give large volumes of anaesthesia behind the globe Use adrenaline in lid blocks PREOPERATIVE MEASURES
- 45. Do not stop NSAIDs for cataract surgery Royal College of Surgeons guidelines
- 46. BP and heart rate monitoring Avoid rapid decompression of globe Gentle manipulation, particularly with nuclear expression Careful with stay sutures Consider use of preplaced ‘safety sutures’ before aspiration and irrigation during all extracapsular extractions INTRAOPERATIVE
- 47. POST-OPERATIVE Avoid eye trauma or eye pressure Avoid hypotony Avoid valsalva manoeuvres
- 49. RAPID CLOSURE OF WOUND Even if vitreous and iris become squeezed into the wound. Use multiple 8/0 or heavier sutures, even silk. Intermittent repositing of the uvea with an iris spatula whilst waiting for suture to be loaded, close wound with anything (clamp, forceps, finger)
- 50. DIRECT PRESSURE ON GLOBE Tamponades the effusion or haemorrhage, which allows coagulation
- 51. If an expulsive event is the cause of protrusion of vitreous, vitrectomy is wrong because this lowers IOP
- 52. IOP LOWERING AGENTS GIVEN STAT ON THE TABLE IV mannitol Carbonic anhydrase inhibitors Topical beta-blockers
- 53. POSTERIOR SCLEROTOMY Indications: – if wound can’t be closed. – Intraocular tissue extrudes in spite of wound closure – IOP remains extremely elevated after 15 to 20 minutes The decision is delayed if the wound is successfully closed without extrusion of tissue May, however, exacerbate bleeding and extrusion
- 54. POSTERIOR SCLEROTOMY: METHOD Use either a blade or Elliot trephine 5-7mm posterior to the limbus in the same quadrant as the major hemorrhagic bulge 1.5mm in diameter
- 55. POSTERIOR SCLEROTOMY: METHOD Haemorrhagic fluid is drained whilst maintaining an elevated IOP (i.e. press on globe) that serves to both stop the bleeding and to extravasate suprachoroidal blood May wish to leave sclerotomies open to allow further post-op drainage
- 56. IMMEDIATE POSTOPERATIVE MANAGEMENT Intensive topical steroids Topical antibiotics Systemic steroids
- 58. 1 day post-op following expulsive haemorrhage
- 59. MANAGEMENT OPTIONS FOR SUPRACHOROIDAL HAEMORRHAGE Observation Delayed secondary management: – Drainage sclerotomy alone (to remove SCH and re-establish normal IOP) – Drainage sclerotomy combined with PPV with or without scleral buckling
- 60. EVALUATION AND TIMING OF SURGERY Between 7 and 14 days post-op, the blood undergoes liquefaction allowing better drainage of the haemorrhage as well as allowing time for intraocular inflammation to settle down. B-scan USS can help ascertain whether complete clot lysis has occurred.
- 61. EVALUATION AND TIMING OF SURGERY Wait 1-2 weeks before draining. Attempts to drain a SCH before some degree of clot lysis has occurred are usually unsuccessful Perform earlier if: – Very high IOP – Corneal lenticular touch – Intractable ocular pain
- 62. MSCH with central retinal and choroidal apposition. Dome shaped appearance. Blood
- 63. MSCH with central retinal and choroidal apposition. Dome shaped appearance. Steeply rising , double peaked , wide spike Lower reflective spikes representing haemorrhage in suprachoroidal space
- 64. 2 days post SCH in another patient. Clot seen as low-medium, irregular internal reflectivity) Blood clot Blood clot
- 65. PROGRESSION OF A CLOT TO LYSIS 24 hours. Central retinal apposition. Arrows point to large blood clot (irregular reflectivity) 5 days . Blood clot is more homogenous (echolucent) 2 weeks. Suprachoroidal space filled with fine diffuse opacities (mobile during dynamic examination) indicative of clot lysis. Low reflective reflectivity of the liquified blood
- 66. Progression of another SCH 24 hours. Central retinal apposition. Arrows point to large blood clot (irregular reflectivity) 2 weeks. Decreased elevation of the choroidal haemorrhage 5 weeks. Resorption of the SCH. Small peripheral SCH.
- 67. VITRECTOMY: indications Indications for vitrectomy include: Vitreous or retinal incarcerated in the wound Vitreous haemorrhage Rhegmatogenous and/or tractional RD (also require scleral buckling) Central choroidal incarceration Persistent flat AC
- 68. VITRECTOMY: Aims of Sx Remove vitreous haemorrhage Remove retained lens material Relieve vitreoretinal traction Reestablish the normal anatomic configuration of the posterior segment
- 69. RECOMMENDED SURGICAL TECHNIQUE (1) 1-3 sclerotomies placed either: – 3-4mm posterior to the limbus – At the equator into the suprachoroidal space Eye initially inflated 1st through a limbal wound, then through a pars plana wound with either: – Saline – Sterile air – PCFL (Perfluorocarbon liquids) which have the advantage compressing suprachoroidal blood anteriorly, thereby facilitating anterior drainage An iris spatula is used to release blood clots through the scleroomy sites
- 70. Insufflation of phakic or aphakic) eye with choroidal haemorrhage An infusion light pipe connected to an air pump, BSS syringe, or perflurocarbon liquid. Use constant infusion pressure. An iris spatula opens the sclerostomy wound and facilitates clot removal
- 71. After the SCH has been drained, the normal anatomic relationship can be reestablished. A 3 port PPV can be made Residual anterior vitreous can be removed with vitrectomy Vitreous strands causing vitreoretinal traction can be cut RECOMMENDED SURGICAL TECHNIQUE (2)
- 72. If a rhegmatogenous RD is present, the retinal break can be treated with retinopexy. If perfluorocarbon liquid used, then perform either: – fluid-fluid exchange with BSS – Liquid-air exchange RECOMMENDED SURGICAL TECHNIQUE (3)
- 73. In most cases a scleral buckle is performed to: – Help relieve residual vitreoretinal traction – Support areas of retinal breaks May need a long-term internal tamponade agent (gas or oil) RECOMMENDED SURGICAL TECHNIQUE (3)
- 74. SECONDARY IOL Can be considered
- 75. There are studies that have suggested that not all cases probably require surgical drainage in order to obtain comparable visual improvement Chu TG, et al. Massive suprachoroidal haemorrhage with central retinal vein apposition. A clinical and echographic study. Archives of Ophth.109 (11): 1575- 81, 1991 Nov.
- 76. PROGNOSIS
- 77. Visual outcome is often bad and can result in total loss of sight. Useful vision can be salvaged in some cases: 20% will attain a post-operative vision of 6/12 or better
- 78. Better prognosis with small incision phaco compared with standard incision ECCE Worse prognosis if vision is PL or worse on 1st post-op day Possible additional sequelae: – 2ry RD complicated by PVR – Phthisis bulbi
- 79. CLINICAL FEATURES ASSOCIATED WITH A POORER VISUAL OUT|COME INCLUDE Initial or indeterminate RD 360 degrees SCH Breakthrough bleeding into the vitreous Subretinal haemorrhage
- 80. OUTCOME AFTER SURGICAL DRAINAGE WITH VITRECTOMY Up to 50% reattachment rate of RD for eyes with retinal incarceration (W. Wirostko, et al, USA) Half of eyes achieve 6/60 vision or better Phthisis bulbi develops in 28% of eyes (might be due to haemorrhagic necrosis of the CB in some cases)
- 81. LIMITED INTRAOPERATIVE CHOROIDAL HAEMORRHAGE Choroidal haemorrhage limited to an ocular quadrant
- 82. Incidence: – 2-5% in ICCE or ECCE – Higher in filtration surgery Presents as positive posterior vitreous pressure with bulging of the iris or vitreous loss at the time of surgery LIMITED INTRAOPERATIVE CHOROIDAL HAEMORRHAGE
- 83. See a dull reddish-brown elevation of the retina The haemorrhage usually remains self- limited, requiring no therapy, and the prognosis for vision is good LIMITED INTRAOPERATIVE CHOROIDAL HAEMORRHAGE
- 84. Possible to get delayed massive SCH
- 85. Occurs more commonly than an intraoperative haemorrhage (~2%) When cataract combined with trabeculectomy. These cases may present with sudden severe ocular pain 1-4 days post-op. Delayed (postoperative) SCH
- 86. Usually preceded by a serous choroidal detachment One possible source of pain: traction on the long posterior ciliary nerves Delayed (postoperative) SCH
- 87. Delayed SCH Retina in AC
- 88. 89 year old female who had complicated cataract extraction+ACIOL+trabeculectomy. 2 days post-op, she awakened with severe eye pain Forward displacement of vitreous and retina Flat AC
- 89. Large , darkly coloured dome-shaped elevations arising from the peripheral retina extending towards the optic nerve
- 90. IOP may be raised from blockage of the filtration sclerostomy or angle closure from forward rotation of the lens-iris diaphragm Ocular contents are not expulsed from the eye unless wound rupture occurs Delayed (postoperative) SCH
- 91. Drainage indicated when: – Very high IOP – Flat AC – In some cases when the vitreous cavity by haemorrhage Surgery for Delayed (postoperative) SCH
- 92. The suprachoroidal space is entered via an equatorial sclerotomy, and the AC is simultaneously filled with air or a viscoelastic during drainage If the haemorrhage occurs after filtration surgery, the sclerotomy may have to be sutured to facilitated drainage Surgery for Delayed (postoperative) SCH
- 93. Between 50-75% of eyes maintain a VA similar to that present prior to the filtration surgery If vitreous is incarcerated in the sclerotomy site, it should be removed to reduce the risk of a post- drainage RD Presence of breakthrough bleeding most often requires: – vitrectomy – Scleral buckle – Air/fluid exchange Surgery for Delayed (postoperative) SCH
- 94. INFUSION MISDIRECTION SYNDROME (IMS) seen in Phaco Sx This can mimic SCH intraoperatively
- 95. INFUSION MISDIRECTION SYNDROME This happens when zonular defects, common in pseudoexfoliation, permit infusion fluid to pass into the retrocapsular space It can also occur in situations where there is a peripheral opening in the posterior capsule
- 96. INFUSION MISDIRECTION SYNDROME This is a common cause of AC shallowing It results in the anterior displacement of the posterior capsule
- 97. INFUSION MISDIRECTION SYNDROME RESEMBLING SCH When confronted with AC shallowing, the surgeon must stop and think what the cause is If the media is clear, ophthalmoscopy will permit visualisation of SCH If the media is not clear or if ophthalmoscopy is not conclusive: – stop the procedure and put patient in recovery room – re-examine in 1 hour – if AC depth remains shallow, SCH is likely and a B- scan will confirm the diagnosis. The procedure must then be cancelled
- 98. INFUSION MISDIRECTION SYNDROME RESEMBLING SCH If the AC depth has returned to normal, the problem was IMS in which case can : – The procedure can be completed by phaco using low flow, low vacuum and low infusion bottle height – Or convert to ECCE – Use a ‘dry’ cortex removal technique utilizing infusion Instead of waiting an hour, you could consider performing a limited pars plana vitrectomy with simultaneous reformation of the AC by viscoelastic injection
- 99. INFUSION MISDIRECTION SYNDROME RESEMBLING SCH Also consider using a dispersive viscoelastic (‘Viscoat’) into the entire periphery of the AC prior to resuming phaco to: – Push the peripheral iris posteriorly – Reduce the possibility of recurrence of IMS by impeding access of fusion to the zonular region IMS is probably much more common than a SCH
- 100. CONCLUSIONS
- 101. CONCLUSIONS Much feared and is often a devastating and blinding condition Think about preventative measures Need quick recognition and quick closure of the wound Vitreoretinal options available post-op Conditions such as IMS can mimic SCH
- 102. THE END
