Unit 2. ANC (2).pptx
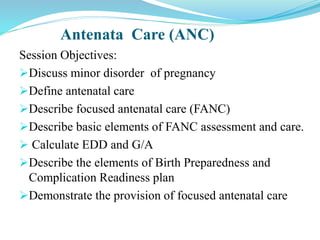
- 1. Antenata Care (ANC) Session Objectives: Discuss minor disorder of pregnancy Define antenatal care Describe focused antenatal care (FANC) Describe basic elements of FANC assessment and care. Calculate EDD and G/A Describe the elements of Birth Preparedness and Complication Readiness plan Demonstrate the provision of focused antenatal care
- 2. Minor Disorders Of Pregnancy Minor disorders are only disorders that occur during pregnancy and are not life threatening. 1.Nausea and vomiting: This presents between 4 and 12 weeks gestation. Hormonal influences are listed as the most likely causes. It is usually occurs in the morning but can occur any time during the day, aggravated by smelling of food. Management: - Reassure the mother - Small, frequent meals, dry meals - Reduce fatty and fried containing foods. - Rest If severe, follow the management of hyperemesis gravidarum ( in hospital set up) 2
- 3. 2. Heart burn: - is a burning sensation in the mid chest region. Progesterone relaxes the cardiac sphincter of the stomach and allows reflex of gastric contents into esophagus. Heart burn is most troublesome at 30-40 weeks gestation because at this stage is under pressure from the growing uterus. Management: - Small and frequent meal, -sleeping with more pillows than usual. -eat less fat more protein - For persistence/sever case/ prescribe antacids 3
- 4. 3. Pica: • This is the term used when mother craves certain foods of unnatural substances such as coal, soil...etc. • The cause is unknown but hormones and changes in metabolism are blamed. • Reduce level of serum iron and zinc also suspected reason. Management: help the women , to avoid eating of harmful substances if the food harmless, give for the women Seek medical advice if the substance craved is potentially harmful to the unborn baby. 4
- 5. 4. Constipation: - Progesterone causes relaxation and decreased peristaltic activity of the gut, which is also displaced by the growing uterus. Management: Increase the intake of water, fresh fruit, vegetables and roughages in the diet. Exercise is helpful, especially walking 5. Backache: Progesterone relax joints and ligaments The enlarged uterus altered the posture, curved backward Management: Advice the mother to sleep on firm bed. Advice support mechanisms of the back, support by straight wall. 5
- 6. 6. Fainting: In early pregnancy fainting may be due to the vasodilatation occurring under the influence of progesterone before there has been a compensatory increase in blood volume. In late pregnancy the pressure of uterus on the inferior vena cava, slows the return of blood to the heart. Management: o Avoid long period of standing o Sit or lie down when she feels slight dizziness o She would be wise not to lie on her back except during abdominal examination 6
- 7. 7. Varicosities Progesterone relaxes the smooth muscles of the veins and result in sluggish circulation. Cause swelling and clot on veins It occurs in legs, vulva and anus (hemorrhoids) Management: • Exercising the calf muscles by rising on the toes • Elevate the leg and rest on the table • Support thighs and legs • Avoid constipation and advise adequate fluid intake. • Sanitary pad give support for vulva varicosities Most minor disorders can be advanced into a more serious complication of pregnancy (Danger signals of pregnancy) 7
- 8. Antenatal Care(ANC) Definition: Antenatal care is a comprehensive primary health care provided for a pregnant women to improve maternal and perinatal outcomes. Objectives of ANC: To 1.Screening, diagnosis and management of pre-existing maternal disorders (DM, CVD, infections. etc). 2.Diagnosis and management of Obstetric and other maternal complications during pregnancy including minor disorders of pregnancy.
- 9. 3. Detection and management or preferable prevention of fetal complications including structural anomalies, infections and growth retardations. 4. Planning for labor and delivery, care of the newborn and future reproductive performance. 5. Ensure the welfare of the mother and the fetus during pregnancy and labour. 6. Ensure that the baby is born with its optimal intellectual and physical abilities
- 10. Sites of ANC: - Home - Private sectors - Public Health facilities Personnel: -Midwives -Nurses -Health officers -Physician -Obstetrician/Gynecologists
- 11. ANC Service should be: - Available - Affordable(cost) - Accessible(any time) - Acceptable(standard) Insufficient antenatal care may be due to: -Ignorance -Poor skill -Poor Incentive for personnel -Ill-trained and supervised staff -Lack of supply -Cost of treatment
- 12. Rights of the Pregnant Woman Health care providers should be aware of the client’s rights when offering antenatal care services. The pregnant woman has the right to: Get information about her health Discuss her concerns, thoughts, and worries Know in advance about any planned procedure to be performed Privacy Confidentiality Express her views about the services she receives Select the health institutions
- 13. Approaches on the number of visits: 1.Traditional Methods 2. Focused ANC Care 1.Traditional approach: Non comprehensive, old, time consuming Follow – up Visits Ideally: -every 4wks up to 28 wks -every 2wks up to 36wks -every 1wk till delivery Alternatively patients can be grouped into low, medium and high risk!!
- 14. The traditional visit is:- not used currently Risk approach Time consuming Tedious for the mother & professionals Quality of care is poor Not woman friendly Poor communication
- 15. 2. Focused ANC: It is comprehensive, coordinated, short and with few number of visits. FANC emphasizes:- Individualized care Client centered Fewer but comprehensive visits Disease detection not risk classification Care by a skilled provider
- 16. In focused ANC system:- Privacy/Confidentiality is assured Continuous care provided by same provider Promotes partner/ support person involvement Adheres to national protocols Referral Facilitated: catchment, ambulance, phone.no ANC, Labour & delivery, PNC And Family Planning Services are linked and housed within the same location if possible.
- 17. Objectives of Focused ANC 1. Health Promotion and Disease Prevention: Counsel the woman and provide the services as necessary: • Immunization against tetanus(TT1-TT5) • Iron and folate supplementation. • How to recognize danger signs, what to do, and where to get help (health education) • Voluntary counseling and testing for HIV • The benefit of skilled attendance at birth • Breastfeeding 17
- 18. • Establish access to family planning • Protection against malaria with insecticide-treated bed nets. • Good nutrition and the importance of rest • Protection against iodine deficiency • Risks of using tobacco, alcohol, local stimulants, and traditional remedies • Hygiene and infection prevention practices • Avoid use of any drug-b/c of Teratogenicity effect. 18
- 19. 2. Early detection and treatment of complications and existing Diseases: Detect pre-existing diseases as early as possible Skilled treatment of complications Do intensive level of monitoring and follow-up care over the course of pregnancy. 19
- 20. 3. Birth Preparedness and Complication Readiness Plan: Approximately 15% of women will develop a life-threatening complication. So, every woman and her family should have a plan for the following: A skilled attendant at birth How to get the place of birth and How to access emergency transportation if needed Items needed for the birth Money saved to pay for transportation, the skilled provider and for any needed mediations and supplies that may not been provided for free Support during and after the birth (e.g., family, friends) Potential blood donors in case of emergency. 20
- 21. In focused ANC WHO recommended 4visits in normal condition: First visit: before 16 wk( conception -16 wk) Second visit: 24-28wk Third visit: at 32 wk Fourth visit: at 36 wk ANC visit must started as early as possible . Good clinical decisions must be made at each visit. 21
- 22. Terminology Gravidity: number of pregnancy Primigravida -a woman pregnant for the first time Multigravida -a woman who has had two or more pregnancies Parity- refers to delivery after point of viability(>28week) Nullipara -a woman who has never produce a viable offspring. Multipara -a woman who has given birth to more than one child. Grandmultipara -woman who has given birth to six or more children
- 23. Lie: is the relationship of the long axis (spine) of the fetus to the long axis of the mother’s uterus. can be: • longitudinal –normal lie • Transverse- abnormal & horizontal • Oblique- abnormal & inclined Attitude: is the relationship of the fetal parts to one another. It can be: • flexion- normal attitude • extension and deflection-are abnormal -Presenting part: is the part of the fetus felt at the lower pole of the uterus and felt on abdominal examination and on vaginal examination.
- 24. Presentation: is the part of the fetus in the lower pole of the uterus. • the normal presentation is vertex and • abnormal are: breech, face, brow and shoulder. Position: is the relationship of the denominator to the six areas of the mother’s pelvis. • Normal position is anterior or lateral and • abnormal position is Occipito-posterior position. Crowned: When the Bi-parietals pass the ischial spines and the head no longer recedes between contraction (the head distends the vulva). Viability= able to survive outside the womb (28+ weeks of gestation.
- 25. Denominator: The part of the fetus which determines the position. (Vertex- occipute, breach -sacrum. Face- mentum, & acromium processes -shoulder). Engagement: when the Bi-parietal diameters of the fetal head passes through the pelvic brim. Stillbirth-birth of baby with no signs of life at or after 28 week of G.A. Abortion-termination of pregnancy before 28 wk of GA. IUFD-fetal death inside the utres after 28 wk of GA. Initially un known by the mother & may not have labour. Neonatal death-death of neonate (birth-28 day)
- 26. Examining a pregnant woman Examination of pregnant woman starts when she enters to the ward(room).e.g. gait, well/sick looking, The examination begin by history taking History taking History taking: Is a means of assessing the health of the woman to find out any condition which may affect child bearing. Social history: name, age ,address, occupation, marital status…etc. Family history: hereditary disease :DM, HPN, twins, psychiatry, heart, allergies ..etc.
- 27. Medical Hx: Past &present: polio, TB, rickets, v. veins, HPN, renal problem, allergy, epilepsy, psychiatry, infection Surgical Hx: Any operation / blood transfusion Past obs and Gyne Hx: History on previous pregnancies and deliveries(complication, fetal condition, fetal Kg -Problems during pregnancy, labour, PPH…. -Gravidity, parity, stillbirth, neonatal death, abortion. -congenital anomaly, Reproductive tumor, History of present pregnancy: -Menstrual history - LNMP, EDD, G/Age -any problem during this pregnancy: malaria, infection, vaginal bleeding, edema. Etc.
- 29. EDD & G/A Calculation: EDD= Expected date of delivery -EDD=LNMP+9month+1oday LNMP=Last normal menstrual period -first day of last menstruation period G/A = Gestational age, age of fetus in intrauterine life -time length from LNMP to the actual visit -commonly express in week/month NB: 5 or 6 day, the 13th month called pagume in Ethiopian calader. So, pleas consider it in EDD & G/A calculation.
- 30. Examples 1. Calculate EDD and G/A of a woman with LNMP of 10/01/2012 EC. EDD= G/A= 2. Calculate EDD and G/A if a woman with LNMP of 20/12/2011 comes for ANC visit by the date of 21/05/2012 EDD= G/A=
- 32. Physical examination Objective: To diagnose pregnancy To identify high risk pregnancy To give advice for pregnant mother
- 33. General examination: -weight, BP, fundal height, FHB, V/S -appearance –sick looking, dehydrated, weak -Abdomen – big ,small , pendulous, flat - Measure height—less than 150 cms ??? - weight-total Wt increment in average is 12kg -in 1st half 20wk- has 2kg increment -In 2nd half 20 wk- has 10kg ’’ ” - Blood pressure –to ascertain the baseline for follow up through out pregnancy. Ultrasound examination- if necessary 16-18wk and 36week is best time.
- 34. Investigations: U/A – Protein, glucose, ketone at 1st visit & as necessary Blood for: - Hemoglobin - VDRL-for syphilis -Blood group, Rh -FBS HIV-test: PMTCT Hgb at 1st visit and 36 weeks At 1st visit (booking visit )only: blood group & RH, PMTCT, (VDRL-may indicate if).
- 35. Physical Examination: Head – clean, scalp– oily, dry, Face –clear, puffy, edema ,jaundice Ear /nose –discharge Neck –gland enlargement Breast –mass , symmetry…. nipple– everted, erect, flat, depressed, inverted, engorgement, colostrum.
- 36. Abdominal Examination AIMS - To observe signs of pregnancy- if not early - To assess fetal growth - To detect any deviation from normal. Steps for Abdominal Examination 1. Inspection 2. Palpation 3. Auscultation
- 37. Inspection a. Shape:-Note contour -is it round, oval, irregular or pendulous? - Longitudinal, ovoid -in primigravida - Round -in multiparaus. - Broad- in transverse lie b) Size:- Should correspond with the estimated GA. c) Skin: - linea-nigra -the dark midline pigmentation -Stare gravid arum –discoloration due to abdominal distattntion e) Scar - Any operation scar(c/s)
- 38. On Palpation: 1. Fundal height and fundal palpation (1st Leopold Maneuver) 1.1 Fundal Height: At 12 wk - the uterus is palpated at sympahysis pubis At 20 week –uterus reaches at umbilicus At 36 weeks -xyphoid process At 40 weeks-returns to about 4 cm below the xyphiod due to “lightening.” Method: Measure distance of funds with points on abdomen
- 39. Assessing the fundal height: 1.tape measurement: by centimeter from sympahysis pubis to xyphoid process. 1cm corresponds with 1 week +/- 2week error 2.fundal palpation: o finger method o above umblicus-1 finger =2week o below umblicus-1 finger =1week Purpose- To know lie, presentation and fundal height(GA).
- 40. Method: - Use palms of 2 hands palpate on with fingers held close together, palpate the upper pole of the fundus. Soft, irregular, bulky, non-ballotable mass(breech). Hard, round ,ballotable mass(head). 40
- 41. 2. Lateral Palpation: (2nd Leopold maneuver) Purpose-To know lie & position Always facing towards the mother and palpate gently by supporting in opposite hands. Irregular, bulky- (Extremities-front side) Linear, rigide,and smooth -(back) Check FHR : -rate and rhythm, -count for one minute(100-180 beat/minute) Use fethoscope: - hand should not touch it while listening, - ear must be in close from contact with fethoscope
- 43. 3. Deep pelvic Palpation(3rd Leo poled Maneuver): Always facing in opposite to the mother and palpate deeply. Purpose -To Know Presentation ,Attitude & descent Presentation: breech/cephalic Attitude: Flexed –cephalic prominence is in opposite side of back. Extended-grove in neck Descent: down warad movement of fetal head -by using rule of 5th : 5/5th- floating, 2/5th -engaged
- 44. 3rd maneuver 44
- 45. Estimation of descent by rule of 5th 45
- 46. 4.Pawlick's Grip: (4th Leopard Maneuver):The lower pole of the uterus is grasped with the right thump &2/3 fingers. Purpose: To know engagement & presentation =fixed head - engaged and floating head is -not engaged 46
- 47. Auscultation: FHR is must auscultated at the back side of the fetus Fetal heart rate is first heard: -at 16-18 week’s -in multipara and -at 18-20 weeks -in primigravida. In breech the fetal heart is heard above the umbilicus. In cephalic presentation it is heard below the umbilicus 47
- 48. Genito-Urinary System: - Frequency of micturition - Check for abnormal discharging Circulatory System: Varicosities: - Varicose veins may occur in the legs, anus (hemorrhoids) and vulva. -Vulval varicosities are rare and very painful. 48
- 49. The Vulva - Vulval warts -irritating discharge The Lower Limbs -Examine for bones alignment and deformities. -Check pitting edema in the lower limbs by applying fingertip pressure for 10 seconds over the tibial bone. -Check DVT-by extension of lower legs.
- 50. Screening High – risk groups: 1. Previous IUFD 2. Previous neonatal death 3. IUGR 4. Polyhydramnios, oligohydramios 5. Unsatisfactory maternal weight gain or weight loss 6. Hypertension 7. Sustained proteinuria of 2+ or > 8. APH 9. Multiple pregnancy
- 51. 10. Recurrent premature labour 11. Medical Conditions 12. Rh- isoimmunization 13. Post-maturity Know decide for: -can we follow -refer immediately or -stay until term & referred
- 52. Health education: Nutrition: Diet – balanced (Protein, CHO, fat. Vitamins) fruits , Iron; calcium, folic acid, increase cal/day, Weight gain – favorable range of 10 – 12Kg Recommended weight gain during pregnancy 1st half 20wk =2 kgs 2nd half 20wk=10—11kgs NB: 0.5kg/week after 2nd half
- 53. Bad habit: avoid use of any drug Alcohol – is best avoided -Fetal Alcohol Syndrome (80 gm/d) -IUGR -Mental retardation Smoking: -IUGR; abruption - in prenatal mortality Exercise– not necessary to limit -but not be vigorous and exhaustive
- 54. Avoid use of raw meat & milk Have adequate rest Avoid any exposure to d/t chemical/radations Start TT vaccination starting from 1st visit. Hygiene : personal/enviromental Use of ITN/bed net-to prevent malaria HIV test & PMTCT Health education about minor disorders
- 55. Clothing – Comfortable, non-constrictive Nipple stimulation -after 36 weeks of pregnancy The Birth plan & Complication Readiness(BP/CR) -Skilled provider -Transportation -Funds(money) -Support person -Blood donor
- 56. ` Provide Iron: take as soon as after gestation starts Every women must take Fe during pregnancy. Iron for 6 month/180 tablet & 1-3 month after birth. Take 1 tap/day in normal condition Iron Folate: 60 mg Ferrous sulphate(Fe) + 400mcg/0.4mg Folic Acid/Vitamin B9 Folic Acid: -formation of RBC & DNA -prevent neural tube defect/spinal cord -helps the body to produce & maintain new cells -prevention & treatment of anemia Source of FA: avocado, beans, peas, nuts, lentils, dark green vegetables & citrus fruit and juice
- 57. Fe used for: -formation of hemoglobin; prevent anemia -transport of oxygen -formation of fetal & maternal RBC. -Source: meat, liver, egg, poultry, brade, cereals, beans, peas, lentils, fruits, & vegetables SE: epigastric pain, constipation/diarrhea, dark feces. Best time to take: empty stomach (1hr before/2hr after meal but to reduce its SE usually taken with meal. CI: milk, antiacid-Mts, oral contraceptive,& drugs like quinolone, ciprofloxacine…… In history of recurrent abortion, spina bifida, hydrocephalus & other conditions Fe folate may start before pregnancy.
- 58. Advice on danger sign: must report??? Vaginal bleeding Blurred vision Reduced fetal movements Sever headache Sudden swelling Rupture of the membrane Premature onset of contractions Maternal anxiety for whatever reason……..???
- 59. Ante partum Fetal Surveillance Definition: Ante partum Fetal Surveillance is method used for assessment of fetal wellbeing and used to identify the fetuses at risk of intrauterine hypoxia or even death in uterus Aims : To identify fetuses at risk of intrauterine hypoxia so that a permanent injury like death should be prevented by timely intervention. To identify healthy fetuses among those suspected to be in problem on clinical evaluation so that an unnecessary intervention may be avoided.
- 60. INDICATATIONS All pregnancies require fetal wellbeing assessment, however it focuses to high risk groups like; 1. Primigravida aged 35 or more. 2. Multipara aged 40 or more. 3. Small for date fetus. 4. Bad obstetrics history. 5. Pre-existing medical conditions. > Diabetes mellitus. > Renal disease. > Hypertension.
- 61. 6. Pregnancy related Diseases: > PIH , rhesus incompatibility. 7. Post date pregnancy. 8. APH.Decreased fetal movements. Timing of prenatal Assessment : -1st trimester – diagnosis of pregnancy and gestational age.-2nd trimester – diagnosis of congenial malformations -3rd trimester – assessment of fetal wellbeing
- 62. Ante partum Fetal Surveillance techniques: 1.Biophysical profile (BPP) 2.Nonstress test (NST) 3.Contraction Stress Test 4.Fetal movement assessment (“kick counts”) =are common ,but many in number
- 63. 1.Biophysical profile (BPP): BPP is consists of 5 components: -Amniotic fluid index (determination of the amniotic fluid volume) -Fetal breathing movements -Fetal movement -Fetal tone -Non-stress test
- 64. Fetal Biophysical Scoring System Parameters score 2 score 0 1.Breathing movements FBM for at least 30 i.Absent secs in 30 mins ii.FBM>30 se 2.Gross body movements 3 movements of 2 or less fetal limbs in30 min movements in 30 mins. 3.Fetal Tone 1 extention with flection i.no ii.slow flextion 4.AFV > =2cm <2cm 5.NST Reactive Non reactivity
- 65. -Score of 8 to 10 - is normal -Score of less 6- is abnormal -Score of 6 &7- is borderline 2.Non-Stress Test =FHB & fetal movement The NST is based on the premise that the heart rate of a fetus that is not neurologically depressed will temporarily accelerate with fetal movement. Heart rate reactivity is thought to be a good indicator of normal fetal autonomic function. Loss of reactivity is associated most commonly with the fetal sleep cycle but may result from any cause of central nervous system depression, including fetal acidosis and some medications.
- 66. To perform NST, the mother is asked to denote when the fetus moves. The fetal heart rate tracing is then evaluated for accelerations of the fetal heart rate corresponding with fetal movement. A reactive (normal)- >2 fetal heart rate accelerations ,15beat/m from base line lasting 15 seconds within a 20- minute period. A nonreactive - lacks sufficient fetal heart rate accelerations over a 40-minute period. The NST of the normal preterm fetus is frequently nonreactive:
- 67. 3.Contraction Stress Test=FHB & Contruction The CST measures the response of the fetal heart rate to uterine contractions. It relies on the premise that fetal oxygenation will be transiently worsened by uterine contractions. To perform CST, the fetal heart rate and uterine contractions are simultaneously recorded with in Doppler US(FHB)&Toco-Daynamometr(contruction). =Negative(normal)-no late deceleration in all contruction. =Positive-has late FHB deceleration with in contruction.
- 68. Repetitive variable decelerations (at least 3 in 20 minutes), even if mild, are associated with an increased risk of cesarean delivery. Decelerations that persist for >1 minute (prolonged decelerations) are associated with a markedly increased risk of both cesarean delivery for a non reassuring fetal heart rate pattern .
- 69. 4.Fetal movement assessment (“kick counts”) This observation provides the rationale for fetal movement assessment by the mother ("kick counts") as a means of ante partum fetal surveillance. There should be minimum of 10 movement within 12hr . - > 12hr for 10 movement is abnormal. - >= 10 movement in 1hr is also abnormal.
- 70. HIV/AIDS By the end of this session, students will be able to discuss: -The difference between HIV and AIDS. -Body Fluids that Transmit HIV and prevention - Stage of HIV/AIDS -Counseling process and advantage of PMTCT -Difference b/n PICT, VCT & PMTCT
- 71. HIV - Human ImmunoVirus; is the virus that attack our immunity and causes AIDS. Specific type of virus (a retrovirus) The CD4 cells are our soldiers and HIV attacks them. Strong CD4 cells are able to fight off infection But, HIV damages the CD4 cell, eventually killing it. So, HIV damages the system that usually protects the body from infection.
- 73. • AIDS- stands for aquired Immuno deficiency Syndrome • Disease limits the body’s ability to fight infection • A person with AIDS has a very weak immune system • No Cure. According to the Centers for Disease Control and Prevention (CDC), a person with HIV infection has AIDS when he or she: has a CD4 cell count (a way to measure the strength of the immune system) that falls below 200. A normal CD4 cell count is 500 or higher. OR develops any of the specific, serious conditions - also called AIDS-defining illnesses - that are linked with HIV infection(OI).
- 74. Potential Bodily Fluids contains HIV Blood products-mainly Semen Vaginal fluids Breast Milk What about tears, sweat, saliva, urine or feces? Reading assignment :?????? -Transmition & Prevention? -WHO 4-stage of HIV?
- 75. HIV and Pregnancy Pregnancy does not accelerate the progression of HIV disease to AIDS. but Patients with AIDS are more likely to suffer from pregnancy related complications.
- 76. Effect of Advanced HIV on pregnancy: Spontaneous abortion Infections (opportunistic, GU, postpartum, post- surgical) Preterm labor Premature rupture of membranes Low birth weight babies Stillbirths
- 77. Current Status of Mother to Child Transmission: During pregnancy: 5-10% During labour &delivery: 1o-20% During breast feeding: 5-10% Maternal factors increase the risk: Severe immune deficiency. Advanced clinical and immunological state Maternal malnutrition. ..etc
- 78. Fetal factors increasing risk: Prematurity Low birth weight multiple pregnancy Viral factors-viral load Obstetric factors: -mode of delivery -PROM- -Routine infant airway suctioning..etc
- 79. National Strategies for PMTCT There are 4 strategies: 1st .Primary prevention of HIV in childbearing women. 2nd .Prevention of unintended pregnancy in HIV positive women. 3rd .Prevention of transmission from HIV + women to their infants. 4th .Treatment, care and support of women infected with HIV, their infants and their families.
- 80. All HIV+ pregnant woman must start ART regardless of there cd4 number. Preferred regiment is:(option B+) =TDF+3TC+EVZ TDF-Tenofovir- has risk of nephrotoxicity 3TC-lamivudine EVZ-Efavirenz
- 81. Nevirapine suspension –to the neonate for 6wk. Wt 2-2.5kg=10mg(1ml)daily Wt >2.5kg=15mg(1.5ml)daily &W<2kg=2mg/kg Feeding option-exclusive breast feeding-best - formula feeding-risk of infection Avoid blood contact b/n mother-baby Skill birth attendant Admit the mother as early as possible Immediately after birth initiate NVP-for neonate as prophylaxis.
- 82. Definition of counseling: Counseling: is a two-way communication process that helps individual to : Examine personal issues Make decisions Make plans for taking action In HIV counseling and testing the focus of the sessions is helping clients to make decision based on their HIV status.
- 83. HIV counseling involves: Listening Respect for the client Confidentiality Asking questions Allowing clients to make their own decisions
- 84. Counseling is not: -Telling clients what to do -Criticizing clients -Forcing ideas or values on clients -Taking responsibility for clients’ actions or decisions.
- 85. Patients Rights during counseling: Confidentiality Privacy Refuse testing Be treated with respect Information Ask questions
- 86. HIV counseling and testing (HCT) Approaches: Client – voluntary counseling and testing (VCT) Provider initiated testing and counseling (PICT) Mandatory and compulsory HIV testing Testing for medical research and surveillance
- 87. Voluntary Counseling & Testing (VCT) is an HIV-prevention intervention initiated by the client at his or her free will. VCT provides the opportunity for the client to confidentially explore and understand his/her HIV risks and to learn his/her HIV infection status with the support of a counselor.
- 88. Components of a VCT Program Type of counseling session Individual Couple Pre-test counseling: Introduction and orientation Risk assessment Option for risk reduction Preparation for the test result
- 89. Post-test counseling: HIV negative test result: Negotiate risk reduction plan Support for risk reduction plan Negotiate disclosure & partner referral HIV positive test result: Identify source of support Negotiate disclosure and partner referral Risk reduction issues Referral
- 90. PICTH-Routine testing of all patients who need an HIV test in addition to other medical checkups. Test is usually offered by a health care worker as part of regular medical care. Increase individuals’ access to HIV testing, and therefore increase the number of people who know their status. Increase uptake of ARVs . Many people prefer to be tested by a health care provider during a regular visit to the clinic. PIHCT takes less time.
- 91. Take Aways Definition & objectives of ANC Approaches of ANC: Traditional Methods & Focused ANC Component of the 4 FANC-Visits: -History taking -EDD & G/A Calculation -Physical examination -4 abdominal Palpation(Leopold maneuver) -Complete health education -Health education about danger signs -Iron folate supplying & TT vaccination -The Birth plan & Complication Readiness -National Strategies for PMTCT
- 92. Thank You