function.pptx
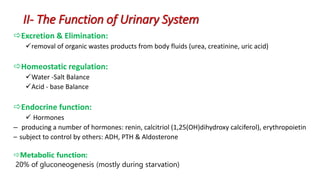
- 1. II- The Function of Urinary System Excretion & Elimination: removal of organic wastes products from body fluids (urea, creatinine, uric acid) Homeostatic regulation: Water -Salt Balance Acid - base Balance Endocrine function: Hormones – producing a number of hormones: renin, calcitriol (1,25(OH)dihydroxy calciferol), erythropoietin – subject to control by others: ADH, PTH & Aldosterone Metabolic function: 20% of gluconeogenesis (mostly during starvation)
- 2. Excretion of excess electrolytes, nitrogenous wastes and organic acids The maximal excretory rate is limited or established by their plasma concentrations and the rate of their filtration through the glomeruli The maximal amount of substance excreted in urine does not exceed the amount transferred through the glomeruli by ultrafiltration except in the case of those substances capable of being secreted by the tubular cells. A - The excretory function II- The Function of Urinary System
- 3. B- Homeostatic Functions Regulate blood volume and blood pressure: by adjusting volume of water lost in urine (action of ADH) releasing renin from the juxtraglomerular apparatus Regulate plasma ion concentrations: sodium, potassium, and chloride ions (by controlling quantities lost in urine) calcium ion levels 1) Water -Salt Balance Blood volume is associated with Salt volume: the greater the blood volume the greater the blood pressure. Removing water (dehydration) lowers blood pressure II- The Function of Urinary System
- 4. The kidneys control this by excreting H+ ions and reabsorbing HCO3 (bicarbonate). 2) Acid-Base Balance (Help stabilize blood pH) If plasma pH is low (acidic). H+ secretion in the urine and HCO3¯ reabsorption back to the plasma increases thus urine becomes more acidic, and the plasma more alkaline. If plasma pH is high (alkaline). H+ secretion in the urine and HCO3¯ reabsorption back to the plasma decreases thus urine becomes more alkaline, and the plasma more acidic. B- Homeostatic Functions II- The Function of Urinary System
- 5. Kidneys have primary endocrine function since they produce hormones (erythropoietin, renin and prostaglandin). Erythropoietin is secreted in response to a lowered oxygen content in the blood. It acts on bone marrow, stimulating the production of red blood cells. Renin the primary stimuli for renin release include reduction of renal perfusion pressure and hyponatremia. Renin release is also influenced by angiotensin II and ADH. The kidneys are primarily responsible for producing vitamin D3 In addition, the kidneys are site of degradation for hormones such as insulin, PTH and aldosterone, C- The endocrine function II- The Function of Urinary System
- 6. Urine formation requires : III. Urine Formation A) Glomerular Filtration Due to differences in pressure water, small molecules move from the glomerulus capillaries into the glomerular capsule B) Tubular reabsorption Many molecules are reabsorbed from the nephron into the capillary (diffusion, facilitated diffusion, osmosis, and active transport) i.e. Glucose is actively reabsorbed with transport carriers. If the carriers are overwhelmed glucose appears in the urine indicating diabetes C) Tubular secretion Substances are actively removed from blood and added to tubular fluid (active transport) ie. H+, creatinine, and some drugs are moved by active transport from the blood into the distal convoluted tubule
- 7. Urine Formation Due to differences in pressure water, small molecules move from the glomerulus capillaries into the glomerular capsule A- Glomerular Filtration What gets filtered in the glomerulus ? • Freely filtered (filtered = passed) • H2O • Elements : (Na+, K+, Cl-, Mg2+ , PO4) • Glucose • Urea • Creatinine • Insulin • Not filtred (not passed) • Protein • Blood cells
- 8. B- System of tubules • Reabsorption from glomerular filtrate: % reabsorbed Water 99.2 Sodium 99.6 Potassium 92.9 Chloride 99.5 Bicarbonate 99.9 Glucose 100 Albumin 95 – 99 Urea 50 – 60 creatinine 0 • Reabsorption can be active or passive and occurs in virtually all segments of the nephron • Reabsorption of water and important particles occurs on these tubules
- 9. Urine Formation Proximal Convoluted Tubule The most metabolically active part of the nephron • 60-80% of reabsorption Driving force is active transport of Na+ • Water follows Na+ Filtrate volume decreases Ultra filtrate Blood
- 10. Urine Formation Loop of Henle • Descending limb - Permeable to water - Impermeable to solutes (Na+, Cl-) • Ascending limb - Impermeable to water - Permeable to solutes (Na+, Cl-)
- 11. Distal Convoluted Tubule Reabsorption of Na+ - Active transport aldosterone dependent - Cl- follows Na+ - Water follows Na+ Excretion of K+ • Reabsorption of Ca++ PTH action
- 12. Urine Formation Collecting Duct • Determines final urine concentration. • Dependent on ADH secretion + ADH No ADH
- 13. IV- Biochemical Tests of Renal Function Measurement of GFR Clearance tests Plasma creatinine Urea, uric acid Cystatin Albuminuria Renal tubular function tests Osmolality measurements Specific proteinuria Glycosuria Aminoaciduria Urinalysis Appearance Specific gravity and osmolality pH osmolality Glucose Protein Urinary sediments
- 14. A. Measurement of GFR Clearance tests Plasma creatinine Urea and uric acid Cystatin Microalbumineria IV- Biochemical Tests of Renal Function
- 15. GFR can be estimated by measuring the urinary excretion of a substance that is completely filtered from the blood by the glomeruli and it is not secreted, reabsorbed or metabolized by the renal tubules. Clearance is defined as the (hypothetical) quantity of blood or plasma completely cleared of a substance per unit of time. Clearance of substances (like Inulin) that are filtered exclusively or predominantly by the glomeruli but neither reabsorbed nor secreted by other regions of the nephron can be used to measure GFR. Inulin The Volume of blood from which inulin is cleared or completely removed in one minute is known as the inulin clearance and is equal to the GFR. Measurement of inulin clearance requires the infusion of inulin into the blood and is not suitable for routine clinical use A1. Measurement of glomerular filtration rate GFR = (U V) P inulin inulin (V is not urine volume, it is urine flow rate)
- 16. 1 to 2% of muscle creatine spontaneously converts to creatinine daily and released into body fluids at a constant rate. Endogenous creatinine produced is proportional to muscle mass, it is a function of total muscle mass the production varies with age and sex Dietary fluctuations of creatinine intake cause only minor variation in daily creatinine excretion of the same person. Creatinine released into body fluids at a constant rate and its plasma levels maintained within narrow limits Creatinine clearance may be measured as an indicator of GFR. A2. Plasma creatinine
- 17. The most frequently used clearance test is based on the measurement of creatinine. Small quantity of creatinine is reabsorbed by the tubules and other quantities are actively secreted by the renal tubules So creatinine clearance is approximately 7% greater than inulin clearance. The difference is not significant when GFR is normal but when the GFR is low (less 10 ml/min), tubular secretion makes the major contribution to creatinine excretion and the creatinine clearance significantly overestimates the GFR. A3. Creatinine clearance and clinical utility
- 18. An estimate of the GFR can be calculated from the creatinine content of a 24-hour urine collection, and the plasma concentration within this period. The volume of urine is measured, urine flow rate is calculated (ml/min) and the assay for creatinine is performed on plasma and urine to obtain the concentration in mg per dl or per ml. Creatinine clearance in adults is normally about of 120 ml/min, The accurate measurement of creatinine clearance is difficult, especially in outpatients, since it is necessary to obtain a complete and accurately timed sample of urine A3. Creatinine clearance clinical utility
- 19. Use of Formulae to Predict Clearance • Formulae have been derived to predict Creatinine Clearance (CC) from Plasma creatinine. • Plasma creatinine derived from muscle mass which is related to body mass, age, sex. • Cockcroft & Gault Formula CC = k[(140-Age) x weight(Kg))] / serum Creatinine (µmol/L) k = 1.224 for males & 1.04 for females • Modifications required for children & obese subjects • Can be modified to use Surface area
- 20. Catabolism of proteins and nucleic acids results in formation of so called nonprotein nitrogenous compounds. Protein Amino acids Ammonia Urea A4. Measurement of nonprotein nitrogen-containing compounds
- 21. Urea is the major nitrogen-containing metabolic product of protein catabolism in humans, Its elimination in the urine represents the major route for nitrogen excretion. More than 90% of urea is excreted through the kidneys, Urea is filtered freely by the glomeruli Plasma urea concentration is often used as an index of renal glomerular function There are many factors, other then renal dysfunction, that affect urea level like: Mild dehydration, high protein diet, increased protein catabolism, muscle wasting as in starvation, reabsorption of blood proteins after a GIT hemorrhage, treatment with cortisol or its synthetic analogous Blood Urea
- 22. Clinical significance of blood urea • States associated with elevated levels of urea in blood are referred to as uremia or azotemia. • Causes of urea plasma elevations: Prerenal: renal hypoperfusion Renal: acute tubular necrosis Postrenal: obstruction of urinary flow Blood Urea The reference interval for serum urea of healthy adults is 5-39 mg/dl. Plasma concentrations also tend to be slightly higher in males than females Azotemia is defined by plasma or serum concentration more than 50 mg/dL
- 23. In human, uric acid is the major product of the catabolism of the purine nucleosides; adenosine and guanosine. Purines are derived from catabolism of dietary nucleic acid (nucleated cells, like meat) and from degradation of endogenous nucleic acids. Overproduction of uric acid may result from increased synthesis of purine precursors. In humans, approximately 75% of uric acid excreted is lost in the urine; the must of the reminder is secreted into the GIT Uric acid
- 24. Renal handling of uric acid is complex and involves four sequential steps: Glomerular filtration of virtually all the uric acid in capillary plasma entering the glomerulus. Reabsorption in the proximal convoluted tubule of about 98 to 100% of filtered uric acid. Subsequent secretion of uric acid into the lumen of the distal portion of the proximal tubule. Further reabsorption in the distal tubule. Hyperuricemia is defined by serum or plasma uric acid concentrations higher than 7.0 mg/dl (0.42mmol/L) in men or greater than 6.0 mg/dl (0.36mmol/L) in women Uric acid
- 25. • Cystatin C is a small polypeptide (13 kDa) produced by all nucleated cells at a constant rate with a stable concentration in blood. Its biological function is an inhibition of cysteine proteases. • The renal handling of cystatin C differs from creatinine. Although both are freely filtered by glomeruli, cystatin C, unlike creatinine, is reabsorbed and metabolized by the proximal renal ducts. Thus, under normal conditions, cystatin C does not enter the final excreted urine to any significant degree. • The serum concentration of cystatin C is not affected by body mass, diet, or drugs. • When GFR decreases, the serum cystatin C concentration increases as a consequence of decreased renal elimination. • Cystatin C is considered to be the more sensitive and earlier marker of GFR in comparison to creatinine. As creatinine has a much smaller molecule than cystatin C, a small decrease in GFR does not affect its elimination and its serum concentration increases later than that of cystatin C. Estimation of GFR from cystatin C
- 26. The glomerular basement membrane does not usually allow passage of albumin and large proteins. A small amount of albumin, usually less than 25 mg/24 hours, is found in urine. Urinary protein excretion in the normal adult should be less than 150 mg/day. When larger amounts, in excess of 250 mg/24 hours, are detected, significant damage to the glomerular membrane has occurred. Quantitative urine protein measurements should always be made on complete 24-hour urine collections. Albumin excretion in the range 25-300 mg/24 hours is termed microalbuminuria. (if examination done on urinary spot it must be reported at 1g of creatinine). Proteinuria
- 27. Proteinuria may be due to: 1. An abnormality of the glomerular basement membrane. 2. Decreased tubular reabsorption of normal amounts of filtered proteins. 3. Increased plasma concentrations of free filtered proteins. 4. Decreased reabsorption and entry of protein into the tubules consequent to tubular epithelial cell damage. With severe glomerular damage, red blood cells are detectable in the urine (hematuria), the red cells often have an abnormal morphology in glomerular disease. Hematuria can occur as a result of lesions anywhere in the urinary tract, Proteinuria
- 28. • Normal < 150 mg/24h. • TYPES OF PROTEINURIA • Glomerular proteinuria • Tubular proteinuria • Overflow proteinuria Proteinuria
- 29. Glomerular proteinuria: • due to increased filtration of macromolecules (such as albumin) across the glomerular capillary wall. • The proteinuria associated with diabetic nephropathy and other glomerular diseases, as well as more benign causes such as orthostatic or exercise-induced proteinuria fall into this category. • Most patients with benign causes of isolated proteinuria excrete less than 1 to 2 g/day Proteinuria
- 30. Tubular proteinuria Low molecular weight proteins — such as ß2-microglobulin, immunoglobulin light chains, retinol-binding protein, and amino acids — have a molecular weight that is generally under 25,000 in comparison to the 69,000 molecular weight of albumin. These smaller proteins can be filtered across the glomerulus and are then almost completely reabsorbed in the proximal tubule. Interference with proximal tubular reabsorption, due to a variety of tubulointerstitial diseases or even some primary glomerular diseases, can lead to increased excretion of these smaller proteins Proteinuria
- 31. Overflow proteinuria • Increased excretion of low molecular weight proteins can occur with marked overproduction of a particular protein, leading to increased glomerular filtration and excretion. • This is almost always due to • immunoglobulin light chains in multiple myeloma, • 2 microglobulin (in acute lymphoproliferative syndrome), • myoglobin (in rhabdomyolysis), • hemoglobin (in intravascular hemolysis) Proteinuria
- 32. •Compared with the GFR as an assessment of glomerular function, there are no easily performed tests which measure tubular function in quantitative manner • Investigation of tubular function: • Osmolality measurements in plasma and urine • Specific proteinuria • Glycosuria • Aminoaciduria B – Renal tubular function test
- 33. B1- Urine and plasma Osmolality • Urinary osmolality is a general marker of tubular function. This is because of all the renal tubule functions, the most commonly affected by the disease is the ability to concentrate the urine. • Water reabsorption requires the integrity of the tubules and collecting canaliculus and the presence of ADH. • The measurement of the renal capacity to concentrate the urine is done by comparison of the urinary osmolality to the plasma osmolality. • Urine osmolality ≥ 600 mosm / kg, tubular function is normal. • Urine osmolality ~ plasma osmolality (urinary / plasma osmolality ratio ~ 1) abnormal tubular function
- 34. Different causes of polyuria Causes U-Osmolality mosm/kg P-Osmolalité mosm/kg Increased osmotic load. (p. ex. glucose) ~ 500 ~ 310 Increased water ingestion < 200 ~ 200 Central diabetes insipidus < 200 ~ 300 Nephrogenic diabetes insipidus < 200 ~ 300
- 35. B2. Water deprivation test Principle: Deprivation of water ADH secretion tubular water reabsorption decreased blood osmolality increased urinary osmolality. Protocol: • Stop any ingestion of water during the night (20h in the evening to 10h in the morning) • measurement of the osmolality of the urine eliminated in the morning. • If urinary osmolality does not increase in response to water deprivation, desmopressin (DDAVP) (a synthetic analogue of ADH) is administered. • The response of the resulting urine osmolality allows to differentiate central diabetes insipidus from nephrogenic diabetes insipidus. • In central diabetes insipidus , the renal tubules normally respond to DDAVP and urinary osmolality increases. • In nephrogenic diabetes insipidus, the renal tubules do not respond: the urinary osmolality remains flat.
- 36. Results after a water deprivation test U Osm mOsm/kg P Osm mOsm/kg ADH ng/l U V ml/min U Osm P Osm P Na mmol/l Normal N 3 à 6 < 0.6 > 2.9 N Central diabetes insipidus (total) ~ 0.5 > 1.5 < 1 Central diabetes insipidus (partial) 3 > 1 < 1.5 Nephrogenic diabetes insipidus ~ 12 > 1 < 1 Potomania N 4 < 1 > 2.9 N
- 37. Renal tubular acidosis (RTA) can be characterized as follows: • Type I: defect in secretion of hydrogen ions by the distal tubule which may be innate or acquired. • Type II: The reabsorption capacity of bicarbonates in the proximal tubule is reduced. • Type III: the reabsorption of bicarbonates by the renal tubule is impaired due to an aldosterone deficiency. • The diagnosis can be confirmed by the acidic load test. • This test involves administering ammonium chloride (which makes the blood more acidic) • and measuring the urinary pH in a series of samples collected every hour for the next 8 hours. (normally urine became more acid) B3. urinary pH and acid load test
- 38. • 2-microglobulin is a small proteins filtered by glomeruli and reabsorbed by tubular cells. • An increase in its urine concentration without increase in serum concentration is a sensitive indicator of tubular reabsorption defect. B4. Specific proteinuria (2-microglobulin)
- 39. • The presence of glucose in the urine when the blood glucose is normal usually reflects the inability of the tubules to reabsorb glucose due to a specific tubular injury (decreased tubular reabsorption threshold of glucose). This is known as renal glycosuria, which is a benign condition. • Glycosuria may also be seen in association with other tubular function disorders, such as renal tubular acidosis, aminoaciduria, and tubular proteinuria. It's Fanconi syndrome. This syndrome can result from heavy metal intoxication, or the effects of toxins and congenital metabolic disorders such as cystinosis. B5. Glycosuria
- 40. • Normally the amino acids present in the glomerular filtrate are reabsorbed in the proximal tubules. • Causes of increased urine amino-acid concentration: • plasma concentration exceeds the renal threshold, • there is a specific failure of normal tubular reabsorption mechanisms, as in cystinuria (a congenital metabolic disorder), or more commonly as a result of acquired tubular lesions. B6. Aminoaciduria
- 41. V- Pathophysiology Acute renal disease (AKD) • Acute renal failure is a sudden deterioration of renal function, indicated by a rapid increase in serum urea and creatinine levels. • The AKD can be corrected, unlike chronic renal failure, which is irreversible. • In general, • If diuresis drops to less than 400 ml / 24h, = oliguria. • If the patient can not urinate at all = anuria. • Occasionally, urinary excretion remains high, especially when tubular dysfunction predominates.
- 42. Biochemical characteristics that distinguish pre-renal uremia from intrinsic kidney damage Characteristics pre-renal kidney failure Intrinsic kidney damage U- Na U- Urea S-Urea U-Osmolality S-Osmolality < 20 mmol/l >20 >1.5 > 40 mmol/l < 10 < 1.1
- 43. V- Pathophysiology • Chronic Kidney Disease (CKD) • A progressive decline in kidney function • Decreased filtration • Progresses to end stage renal disease • Dialysis or kidney transplant
- 44. Consequences of the CKD Metabolism of water and sodium • The reabsorption capacity of Na+ ions is most often conserved; however, the ability to reabsorb water can be lost. • Polyuria, although present, is not excessive because of the weakness of GF. Because of their inability to regulate the water balance, patients with CKD are very frequently in overload or fluid depletion. • In the early stages of CKD, the normal reduction in urine formation when the patient is asleep is lost. Patients who do not have polyuria in the day may still have nocturia as a call symptom. V- Pathophysiology
- 45. Consequences of the CKD • Potassium metabolism • Hyperkalemia .The ability to eliminate K decrease • Acid-base balance • As it develops, CKD reduces the kidney's ability to regenerate bicarbonates and eliminate H+ ions. The retention of hydrogen ions causes metabolic acidosis. • Synthesis of erythropoietin • Chronic nephropathies are often accompanied by normochromic normocytic anemia, mainly due to a lack of erythropoietin production. . V- Pathophysiology
- 46. Drop in the formation of 1,25- 2(OH) D3 Progressive distraction of the nephron Increased phosphate retention Decreased serum Ca++ Decreased intestinal absorption of Ca++ Increased serum phosphate Increased PTH biosynthesis and secretion Calcium and phosphates metabolism Consequences of the CKD Increased osteoclast activity Renal osteodystrophy
Notas del editor
- Creatinine is not reabsorbed by tubule after filtration. The quantities if final urine = to the quantities in primary urine
- In descending limb we have reabsorption of water without solutes this lead to the increase in urine density In ascending limb we have reabsorption of solutes without water this lead to the decrease in urine density
- In this part of nephron, there is a final adjustment of the level of Na and K by action of Aldosterone (water follow Na) and the reabsorption of Ca by action of PTH.
- After water deprivation: Normally there is a decrease in blood volume which will cause a secretion of ADH which increases the absorption of water at the level of the distal and collecting tubule. the result is a decrease in urine volume and an increase in urine osmolarity. Urine Osm / Plasma Osm ratio is greater than 2.9 In the case of total diabetes insipidus (total absence of ADH secretion) the urine osmolarity remains low and the blood osmolarity increases even more with increase in blood sodium. Urine volume remains high and the urine osmolarity / blood osmolarity ratio is less than 1. In the case of partial diabetes insipidus (decrease in the secretion of ADH) the urinary osmolarity as well as the osmolarity and the plasma sodium remain slightly high. the urine osmolarity / blood osmolarity ratio is less than 1.5 In case of nephrogenic diabetes insipidus (insensitivity of tubular receptors to the action of ADH) same result as diabetes insipidus but here the rate of ADH is high. In the event of potomania (heavy drinker of water) the plasma osmolarity, the sodium plasma and the level of ADH are normal. There is only the urine volume which is a little higher than normal with lowered osmolarity
- In prerenal failure the quantities of blood that reaches the glomerulus is reduced but the mechanism of filtration and reabsorption still proportional. In case of intrinsic kidney damage, there is no filtration so the quantities in plasma raise and in urine fall.