brief prabowo nsteacs.pptx
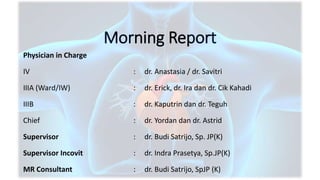
- 1. Morning Report Physician in Charge IV : dr. Anastasia / dr. Savitri IIIA (Ward/IW) : dr. Erick, dr. Ira dan dr. Cik Kahadi IIIB : dr. Kaputrin dan dr. Teguh Chief : dr. Yordan dan dr. Astrid Supervisor : dr. Budi Satrijo, Sp. JP(K) Supervisor Incovit : dr. Indra Prasetya, Sp.JP(K) MR Consultant : dr. Budi Satrijo, SpJP (K)
- 2. SUBJECTIVE Mr. P/60 yo/ID 11536070 CHIEF COMPLAINT : Chest Pain Patient complained about chest pain at 06.00 AM (2 hours before RSSA admission) with VAS score 8/10, when he was lying on bed. It was heavy-like sensation, without radiated to the back, with duration more than 30 minutes, and accompanied with cold sweating. Nausea (-), vomiting (-), SOB (- ). There was no stabbing like sensation and chest pain was not affected with inspiration, positional changes, or food intake. Because the chest pain still persisted, patient directly went to RSSA. In ER RSSA at 00.30 AM, patient said that chest pain still already felt with VAS 8/10 mmHg. GCS was 456, BP 160/112 mmHg, HR 81 bpm, RR 26x/min and Sat 99% on NC 3 lpm NC. He was given drip NTG 40 mcg/min, loading aspilet 4 tab, and CPG 4 tab, and his BP was improved 130 / 90 mmHg, and chest pain improved with VAS 4/10. Previously, he suffered from similar chest pain, with VAS score 6/10 while at rest. It was occured At 05.00 AM (19 hours before RSSA admission). He was taking isosorbide dinitrate 5 mg, with 6 times of repetition, but the chest pain did not Improved.
- 3. SUBJECTIVE Mr. P/60 yo/ID 11536070 PAST MEDICAL HISTORY : • He had suffered from similar chest pain 1 year ago and checked at private hospital in Malang. He was diagnosed with NSTEMI, and was referred to other hospital for further management. Coronary angiography was perform and the result was CAD 3VD + LM disease. Then he planned to be referred to cardiologist outpatient clinic for consideration for elective PCI or CABG. But patient never came to control at RSSA because he refused for operation. After that Patient never controlled to any cardiologist and also didn’t take any medication • History of DOE (+) while doing moderate-heavy activities since 1 month. OE, PND, Leg swelling, palpitation, and syncope was denied
- 4. SUBJECTIVE Mr. P/60 yo/ID 11536070 RISK FACTOR : • He had hypertension since 20 years ago, didn’t routinely consume medication • He is an a passive smoker for the last 1 year • History of diabetes mellitus, CKD, CAD and other disease was denied. FAMILY HISTORY : History of hypertension on her family was denied There was no sudden cardiac death and cardiac disease in her family. He was the 2nd son out of 5 siblings. Screening for covid-19 There was no cough, fever, sore throat, anosmia, dysgeusia in the last 14 days ago. History of traveling to red zone area was denied History of contact with patient confirmed COVID-19 was denied He lives in orange zone area He hasn’t yet vaccinated covid-19
- 5. OBJECTIVES Physical Examination : General appearance moderate ill BW 65 kg Height 160 cm BMI 25.4 kg/m2 (overweight) GCS 456, VAS 8/10 drip GTN 40 mcg/min, VAS 4/10 BP 160/112 mmHg drip GTN 40 mcg/min 130/70 mmHg PR 100 bpm regular, strong pulse RR 20 tpm SpO 99% NC 3 lpm Tax: 36,50C Head and Neck : Anemic conjuctiva +|+; icteric sclera -|- nostril breathing (-), sternocleidomastoid muscle retraction (-) JVP R+1 cmH O OBJECTIVES Thorax : Cor: ictus cordis, palpable at 1 cm lateral MCL V sinistra S1-S2 regular normal, murmur (-), gallop (-) Pulmo: symmetrical movement, intercostal muscle retraction (-) ves/ves Rh -/- wh - / - ves/ves -/- - / - Ves/ves +/+ - / - Abdomen : flat, soefl, bowel sound was normal, liver and spleen unpalpable, shifting dullness (-) Extremities : leg swelling -|- , warm acrals, CRT < 2 seconds Urine output : 350 cc (initial) inj furosemide 40 mg 1750 cc/2 hours
- 6. ECG at RSSA (April 18th 2022) at 00.30 Sinus rhythm, HR 100 bpm, FA LAD, HA N. normal P wave, PR Int 160 ms. narrow QRS 80 ms. Pathological Q waves in lead III. ST segmen depression V2 (3 mm), V3(4 mm), V4(4.5 mm). T wave normal. QTc 337 msec. LVH(-), RVH (-), LAE (-), RAE(-). Conclusion : Sinus tachycardia with ischemia
- 7. ECG at CVCU (March 4th 2022) Sinus rhythm, HR 100 bpm, FA LAD, HA N. normal P wave, PR Int 160 ms. narrow QRS 80 ms. Pathological Q waves in lead III. ST segmen depression V2 (1 mm), V3(1.5 mm), V4(0.5 mm). Biphasic T wave at V2,V3,V4. QTc 397 msec. LVH(-), RVH (-), LAE (-), RAE(-). Conclusion : Sinus tachycardia, with ST-T changes (+) ECG at RSSA (April 18th 2022) at 2.30
- 8. ECG at CVCU (March 4th 2022) Sinus rhythm, HR 98 bpm, FA LAD, HA N. normal P wave, PR Int 160 ms. narrow QRS 80 ms. Pathological Q waves in lead III. ST segmen depression V2 (2 mm), V3(1 mm), V4(1 mm). T wave normal. QTc 486 msec. LVH(-), RVH (-), LAE (-), RAE(-). Conclusion : Sinus tachycardia, ischemia, and prolonged QTc. ECG at Persada Hospital (May 30th 2021)
- 9. CXR at Persada Hospital (May 30th 2021) AP position, symmetrical, enough inspiration, enough KV Soft tissue: Normal Bone: Costae D/S normal ICS D/S normal Trachea: In the middle Cor: Site: N Size: CTR 56% Cardiac waist (+) Aorta dilatation (+) Hemidiaphragm: D: dome shape S: hard to evaluate Vascular apex D increased Costophrenic angles: D: sharp, S: hard to evaluate Pulmo : Infiltrate (-) Conclusion : Cardiomegaly with HHD configuration Aorta dilatation
- 10. CXR at RSSA (April 18th 2022) AP position, symmetrical, less inspiration, enough KV Soft tissue: Normal Bone: Costae D/S normal ICS D/S normal Trachea: In the middle Cor: Site: N Size: CTR 67% Cardiac waist (-) Hemidiaphragm: D: dome shape S: hard to evaluate Bronchovesicular pattern dextra and sinistra increased Costophrenic angles: D: sharp, S: hard to evaluate Pulmo : Infiltrate (-) Conclusion : Cardiomegaly with HHD configuration Susp. Pleural effusion sinistra
- 11. Parameter Result Normal Value Hb 10 g/dL 11.5 – 18.0 g/dL Leukocytes 10,500 /µL 4000 - 11000/µL Hematocrit 31,5 % 35 - 45 % Thrombocytes 302,000 /µL 150000-450000/µL Differential count 1/0.3/61.7/25/12 1-2/0-1/3-5/54-62/25-33/3-7 % NLR 2.48 PPT 10.6 detik 9.4 – 11.3 aPTT 25.2 detik 24.6 – 30.6 INR 1.02 <1.5 Random Blood Sugar 108 mg/dL <200 mg /dl SGOT 83 U/L 0-40 U/L SGPT 24 U/L 0-41 U/L Albumin 4.08 mg/dl 3.5 – 5.5 Parameter Result Normal Value Na 140 mmol/L 136 – 145 K 3.47 mmol/L 3.5 – 5.0 Cl 102 mmol/L 98 - 106 Ureum 23.9 mg/dL 16.6-48.5 Creatinin 1.13 mg/dL <1.2 eGFR 70.256 mL/mnt/1. 73 m2 Procalcitonin 0.06 ng/mL <0.1 Troponin I 2.4 ng/mL <0.1 CKMB 105 mg/dL 7-25 CRP 1.41 mg/dL <0.3 Date: April 18th 2022 Laboratory Finding at RSSA
- 12. Parameter Result Normal Value pH 7,45 7.35 – 7.45 pCO2 29,7 mmHg 35 - 45 pO2 120,1 mmHg 80 - 100 HCO3 20,6 mmol/L 21 - 28 BE -3,7 mmol/L -3 - +3 SaO2 99,9 % >95 Respiratory Alkalosis Fully Compensated Date: April 18th 2022 Blood Gas Analysis at RSSA with NC 4 lpm
- 13. Echocardiography at Prima Medika Hospital (May 8th 2021) Dimensi ruang jantung normal LV concentric hypertrophy (LVMI 118 g/m2, RWT 0.43) Fungsi sistolik LV : EF teach 56%, biplane 66% Fungsi diastolic LV : impaired relaxation (E/A 0.59) Fungsi sistolik RV : normal (TAPSE 1.63 cm) Analisa segmental : hipokinetik anteroseptal setinggi mid, hipokinetik anterior setinggi apex Kesimpulan : Hypertensive heart disease Diastolic dysfunction LV gr I Mild MR Coronary Artery Disease
- 14. LAO-CRA RAO-CRA
- 15. RAO-CAU LAO-CAU
- 16. RAO-CRA LAO-CRA
- 17. Coronary angiography at Persada Hospital LM : stenosis 10% mid-distal LAD : stenosis 95-99% at osteal-proximal. CTO at proximal, got collateral from contralateral Intermediate : stenosis 90% at osteal- proximal LCx : co-dominsasnt. Stenosis 90% at osteal-proximal. Stenosis 60-70% at distal RCA : stenosis 60% at osteal-mid. stenosis 40% at RPL. Stenosis 80% at PDA Conclusion : CAD 3VD Suggest to : CABG/high cost PCI
- 18. Assessment 1. NSTEMI killip II (Very high risk criteria) TIMI 5/7, GRACE 140 CRUSADE 27 2. HF st C fc II dt CAD, HHD 3. Hypertension st II 4. History of smoker
- 19. Planning Diagnosis & Therapy Planning diagnosis Echocardiography ECG/24 hours, FBG/2hPPBG, HbA1c, UA, profil lipid Planning therapy Pro Early Immediate invasive strategy with IABP backup Bedrest O2 NC 2 lpm Total Fluid 2000 ml/24 h IVFD NS 0.9% 1000 ml/24 h Oral Intake 1000 cc/24 hr Equal fluid balance Heart Diet 1800 kkal/day Drip GTN 40 mcg/min Inj. Enoxaparin 2x60mg sc Inj. Lansoprazol 1x30mg Inj. Furosemide 40 mg 3x20mg Peroral ASA 320 mg 0-0-80mg Clopidogrel 300 mg 75mg-0-0 Atorvastatin 0-0-40mg Captopril 3x25mg Bisoprolol postponed Diazepam 0-0-2mg Laxadyn 0-0-CI Planning Monitoring Subjective, Vital Sign, UOP, Bleeding Sign, ECG/24h Admitted to ICVCU
- 20. Condition at the end of the duty • S: chest pain (-) • O: • BP 126/70 mmHg • HR 90x/min • RR 20x/min • Tax 36.5 degrees C • SpO2 99 % NC 4 lpm • Rh --+/--+ Wh -/- • Edema -/- • Urine output 3000 ml/7hours
- 23. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Table 2 Conditions other than acute type 1 myocardial infarction associated with cardiomyocyte injury (= cardiac troponin elevation) (1) Tachyarrhythmias Heart failure Hypertensive emergencies Critical illness (e.g. shock/ sepsis/ burns) Myocarditisa Takotsubo syndrome Valvular heart disease (e.g. aortic stenosis) Aortic dissection Pulmonary embolism, pulmonary hypertension Renal dysfunction and associated cardiac disease Bold = most frequent conditions. aIncludes myocardial extension of endocarditis or pericarditis.
- 24. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Table 2 Conditions other than acute type 1 myocardial infarction associated with cardiomyocyte injury (= cardiac troponin elevation) (2) Acute neurological event (e.g. stroke or subarachnoid haemorrhage) Cardiac contusion or cardiac procedures (CABG, PCI, ablation, pacing, cardioversion, or endomyocardial biopsy) Hypo- and hyperthyroidism Infiltrative diseases (e.g. amyloidosis, haemochromatosis, sarcoidosis, scleroderma) Myocardial drug toxicity or poisoning (e.g. doxorubicin, 5-fluorouracil, herceptin, snake venoms) Extreme endurance efforts Rhabdomyolysis Bold = most frequent conditions. aIncludes myocardial extension of endocarditis or pericarditis.
- 25. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 3 (1) 0 h/1 h rule-out and rule-in algorithm using high-sensitivity cardiac troponin assays in haemodynamically stable patients presenting with suspected non-ST- segment elevation acute coronary syndrome to the emergency department. aOnly applicable if CPO >3 h.
- 26. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Table 4 Differential diagnoses of acute coronary syndromes in the setting of acute chest pain Bold = common and/or important differential diagnoses. aDilated, hypertrophic and restrictive cardiomyopathies may cause angina or chest discomfort.
- 27. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 6 Antithrombotic treatments in non-ST- segment elevation acute coronary syndrome patients: pharmacological targets. Drugs with oral administration are shown in black letters and drugs with preferred parenteral administration in red. Abciximab (in brackets) is not supplied anymore.
- 28. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 9 Selection of non-ST-segment elevation acute coronary syndrome treatment strategy and timing according to initial risk stratification
- 29. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Recommendations for coronary revascularization (1) Recommendations Class Level Timing of invasive strategy An immediate invasive strategy (<2 h) is recommended in patients with at least one of the following very-high-risk criteria: • Haemodynamic instability or CS • Recurrent or refractory chest pain despite medical treatment • Life-threatening arrhythmias • Mechanical complications of MI • Heart failure clearly related to NSTE-ACS • Presence of ST-segment depression >1 mm in ≥6 leads additional to ST-segment elevation in aVR and/or V1. I C
- 30. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Recommendations for coronary revascularization (2) Recommendations Class Level Timing of invasive strategy (continued) An early invasive strategy within 24 h is recommended in patients with any of the following high-risk criteria: • Diagnosis of NSTEMI suggested by the diagnostic algorithm recommended in Section 3 • Dynamic or presumably new contiguous ST/T-segment changes suggesting ongoing ischaemia • Transient ST-segment elevation • GRACE risk score >140. I A
- 31. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Recommendations for coronary revascularization (3) Recommendations Class Level Timing of invasive strategy (continued) A selective invasive strategy after appropriate ischaemia testing or detection of obstructive CAD by CCTA is recommended in patients considered at low risk. I A Delayed as opposed to immediate angiography should be considered among haemodynamically stable patients without ST-segment elevation successfully resuscitated after out-of-hospital cardiac arrest. IIa B
- 32. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 13 (1) Central illustration. Management strategy for non-ST-segment elevation acute coronary syndrome patients.
- 33. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 13 (2) Central illustration. Management strategy for non-ST-segment elevation acute coronary syndrome patients.
- 34. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 13 (3) Central illustration. Management strategy for non-ST-segment elevation acute coronary syndrome patients.
- 35. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Figure 13 (4) Central illustration. Management strategy for non-ST-segment elevation acute coronary syndrome patients.
- 36. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Supplementary Table 8 Lifestyle recommendations Smoking cessation Use pharmacological and behavioural strategies to help patients quit smoking. Avoid passive smoking. Healthy diet Diet high in vegetables, fruit, whole grains; limit saturated fat to <10% of total. Limit alcohol to <100 g/week or 15 g/day. Physical activity 30–60 min moderate physical activity most days, but even irregular activity is beneficial. Healthy weight Obtain and maintain a healthy weight (BMI 18.5–25 kg/m2) or reduce weight through recommended energy intake and increased physical activity. Other Take medication as prescribed. Sexual activity is low risk for stable patients who are not symptomatic at low-to-moderate activity levels. Lifestyle recommendations are based on ESC CCS Guidelines
- 37. www.escardio.org/guidelines 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575) ©ESC Supplementary Table 9 Healthy diet Increase consumption of fruit and vegetables (≥200 g each per day) 35–45 g of fibre per day, preferably from whole grains Moderate nut consumption (30 g unsalted) 1–2 servings of fish per week (one to be oily fish) Limited lean meat, low-fat dairy products, and liquid vegetable oils Saturated fats to account for <10% of total energy intake, replace with polyunsaturated fats Trans unsaturated fats as low as possible, preferably no intake from processed food, and <1% of total energy intake ≤5–6 g of salt per day If alcohol is consumed, limiting intake to ≤100 g/week or <15 g/day is recommended Avoid energy-dense foods such as sugar-sweetened soft drinks Results are based on the results of a systematic review by de Vries et al.
- 38. Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation 42
- 39. Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation 43
- 40. Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation 44
- 41. Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation 45
- 42. Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation 46
- 43. 47 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 44. 48 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 45. 49 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 46. 50 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 47. 51 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 48. 52
- 49. 53 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 50. 54 Jean-Philippe Collet. 2020. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation
- 51. Stent thrombosis
- 52. Intraprocedural stent thrombosis (IPST) INTRODUCTION a rare complication leading to poor outcome including STEMI and sudden cardiac death 47 (0.7%) of 6,591 patients with incident IPST Death within 30 days was higher (12.9% vs 1.4%) Mortality within one year was also higher (19.9% vs. 2.7%) 0.5-2% in the case of elective PCI 6% in the case of PCI with acute coronary syndromes Safety concerns regarding an increased risk of stent thrombosis with drug eluting stent (DES) persist while the incidence, timing, and predictors of stent thrombosis with DES have not been determined Oktaviono YH. Folia Medica Indonesiana Vol. 52. 2016 : 66-73 Iqbal J, et al. EuroIntervention. 2013,9:62-69
- 53. Definition of Intraprocedural Stent Thrombosis (IPST) Intra-procedural stent thrombosis (IPST) is defined as an angiographically confirmed intraluminal filling defect within the stent that results in occlusive or non-occlusive thrombolysis in myocardial infarction (TIMI) grade-0 or 1 anterograde flow, secondary to the development of new or increasing thrombus within or adjacent to a recently implanted stent, occurring during the index procedure or before the percutaneous coronary intervention (PCI) is completed. Oktaviono YH. Folia Medica Indonesiana Vol. 52. 2016 : 66-73 Brener et al. JACC: Cardiovascular Interventions. Vol. 6. 2013: 36-43 IPST has an incidence of 0.7% after drug eluting stent (DES), and <0.01% after bare metal stent (BMS) implantation in patients without acute myocardial infarction (AMI), thrombus-containing lesions and dissections. It occurs in <1% of patients with ST-segment elevation myocardial infarction (STEMI).
- 54. The Academic Research Consortium (ARC) has standardized the definitions of ST by categorizing the specificity of the adjudicated event (definite, probable, or possible) and its timing relative to PCI (acute, subacute, late, and very late). Intra-procedural stent thrombosis (IPST) (i.e., the development of occlusive or non-occlusive new thrombus in or adjacent to a recently implanted stent before the PCI procedure is completed) is excluded from the ARC ST definitions. Brener et al. JACC: Cardiovascular Interventions. Vol. 6. 2013: 36-43 Claessen et al. JACC: Cardiovascular Interventions. Vol. 7. 2014:1081-1092
- 55. End Point Definition of Stent Thrombosis by The Academic Research Consortium (ARC)-2 Garcia et al. Circulation. 2018:137:2635–2650
- 56. The most important aspect for the diagnosis and treatment of IPST is clinical suspicion of early stent thrombosis. Diagnosis of Intraprocedural Stent thrombosis (IPST) The typical clinical presentation of stent thrombosis consists of chest pain and ischemic electrocardiographic changes in the target vessel territory. However, ST can also present as sudden death, or it can be asymptomatic in the setting of collateral vessels. Hyo-Sun Shin, et al. J Lipid Atheroscler. 2014;3(1):43- 48
- 57. Coronary intervention-related MI is arbitrarily defined by an elevation of cTn values more than five times the 99th percentile URL in patients with normal baseline values. In addition, one of the following elements is required: 1. New ischaemic ECG changes 2. Development of new pathological Q waves 3. Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic aetiology; 4. Angiographic findings consistent with a procedural flow-limiting complication such as coronary dissection, occlusion of a major epicardial artery or a side branch occlusion/thrombus, disruption of collateral flow, or distal embolization. Criteria for PCI-related MI 48 h after the index procedure (type 4a MI) Thygesen K, et al. 2018. European Heart Journal 2019, 40: 237–269
- 58. When a filling defect is detected angiographically: Intravascular ultrasound (IVUS) may be used to detect the underlying mechanism of ST (underexpansion, malapposition, edge dissection). Optical coherence tomography (OCT) is very suitable for visualization of the stent surface for its higher resolution (10 mm), and its ability to detect the presence of (sub) clinical thrombus has been experimentally confirmed. In this patient, as soon as the action predilatation with balloon and stent, we found ischaemic ECG changes and thrombus intracatheter in the end of procedure. The ECG monitor back to the baseline soon after we gave loading Ticagrelor 180 mg, Atorvastatin 40 mg and intracoronary heparin 1000 mg. Diagnosis of Intraprocedural Stent thrombosis (IPST) Genereux P, et al. 2014. Journal of the American College of Cardiology Vol. 63, No. 7, 2014: 619-629
- 59. Pathophysiology of Stent Thrombosis Many factors are involved including procedural factors/stent, patient factors and lesion characteristics. Patients with acute coronary syndrome, inflammation and tissue necrosis were exposed to the circulation so as to strengthen the activity of platelets and easily formed thrombus. The material in the form of a polymer stent Cypher (sirolimus) and Taxus (paclitaxel) DES can cause infiltration of eosinophils suspected hypersensitivity reaction that can trigger platelet adhesion and activation cascade coagulant. Brener et al. JACC: Cardiovascular Interventions. Vol. 6. 2013: 36-43 Claessen et al. JACC: Cardiovascular Interventions. Vol. 7. 2014:1081-1092
- 60. There are two kinds of thrombus: White thrombus : a platelet-rich thrombus, usually only lead to partial occlusion Red thrombus : a rich thrombus fibrin and erythrocytes. White thrombi composed approximately one-third of specimens retrieved during PCI in a contemporary sample of patients from a high-volume referral center. Patients with white thrombi had less ischemic time and had smaller vessels when compared with those with red thrombi. THROMBUS Quadros AS, et al. 2012. American Heart Journal Volume 164, Number 4: 554-560
- 61. Torrado, J. et al. J Am Coll Cardiol. 2018;71(15):1676–95 Pathogenic Mechanisms of Stent Thrombosis
- 62. Multiple Risk Factors Involved In The Development Of Stent Thrombosis
- 63. Device-related factors (or stent thrombogenicity), including stent material, surface coating, and the interaction with adjunctive therapy such as intracoronary brachytherapy. Platelet activation was greater during the 30 days after implantation of an open-cell versus a closed-cell stent, which was potentially related to the different scaffolding properties of the stents. The content of the drugs currently on the DES can be prothrombogenic. Rapamycin and Paclitaxel works by blocking the migration and proliferation of smooth muscle cells that plays a role in neointimal formation and restenosis. However, both drugs induce endothelial expression of tissue factor that will bind to the clotting factor so that the formation of fibrin. STENT FACTORS Claessen et al. JACC: Cardiovascular Interventions. Vol. 7. 2014:1081-1092 Oktaviono YH. Folia Medica Indonesiana Vol. 52. 2016 : 66-73
- 64. Patient- or lesion-specific factors, including vessel size, acute coronary syndrome/unstable angina, plaque characteristics, local platelet/coagulation activity, coronary blood flow, and left ventricular ejection fraction. A polymorphism of platelet glycoprotein IIIa gene (PlA2) may also be associated with an increased risk of stent thrombosis. Other patient characteristics that favor the development of stent thrombosis include diabetes mellitus, chronic kidney disease, smoker, cancer, DAPT non-responsive, premature cessation of DAPT, advanced age and hypersensitivity to polymer or drug. PATIENT- OR LESION-SPECIFIC FACTORS Claessen et al. JACC: Cardiovascular Interventions. Vol. 7. 2014:1081-1092
- 65. PREDICTORS OF IPST Over the past several years, many researchers have investigated potential predictors of stent thrombosis especially acute and sub-acute categories and identified a number of angiographic, clinical, procedural and post-procedural risk factors of stent thrombosis A risk score has been proposed to personalize risk assessment for the occurrence of ST and may be used to identify patients who might benefit the most from more aggressive antiplatelet therapy after stent implantation. Iqbal J, et al.. Euro Intervention 2013; 9: 62-69
- 66. Predictors of Early and (Very) Late Stent Thrombosis Claessen et al. JACC: Cardiovascular Interventions. Vol. 7. 2014:1081-1092
- 67. Predictors of IPST Clinical risk score for prediction of stent thrombosis and risk stratification as developed by Baran et al 8 significant predictors, with a stratification of patients in low, medium, and high risk groups, and has been validated using 1-year data from 4,820 patients. PATIENT’S SCORE: 12 Iqbal J, et al.. Euro Intervention 2013; 9: 62-69
- 68. Predictors of IPST Stent Thrombosis Risk Score (STRS) in predicting early stent thrombosis (ST) after primary Percutaneous Coronary Intervention (PCI). A total of 569 patients were included, the median age was 56 years. Early ST was observed in 33 (5.8%) patients. Early ST rate was 3.3% at STRS of 0-2, which raised to 5.0% at STR of 3-4, and 17.2% at STRS of ≥5 PATIENT’S SCORE: 3 Kumar R, et al. Journal Of The Saudi Heart Association 2020;32:256-262
- 69. Predictors of IPST Association of the CHA2DS2VASc Score with Acute Stent Thrombosis 3,460 consecutive patients with STEMI who underwent a PPCI. CHA2DS2VASc scores ≥ 4 were independently associated with acute stent thrombosis. Patients with a CHA2DS2VASc score of 4 had a 4.3 times higher risk of acute stent thrombosis compared to those with a CHA2DS2VASc score of 1. PATIENT’S SCORE: 3 Tanik OZ, et al. 2019. Med Princ Pract 2019;28:115–123
- 70. Predictors of IPST Integer-Based Risk Score for 1-Year Definite/Probable Stent Thrombosis in Patients With Acute Coronary Syndromes 6,139 patients undergoing PCI with stent implantation for ACS. Risk scores 1 to 6 were considered low risk (1.36%), 7 to 9 intermediate risk (3.06%), and ≥10 high risk for ST (9.18%). PATIENT’S SCORE: 6 Brener SJ, et al. 2013. JACC: Cardiovascular Interventions Vol.6, No.1,2013: 36-43
- 71. Stent Thrombosis Management If ST is the case then action targets PTCA for revascularization of blood vessels should be done immediately. Guidewire selected must be soft and floppy to ensure free through the lumen of the stent and not crossing through the strut stent Aspiration trombhectomy intra coronary thrombus is effective for the treatment of ST especially on stents with a diameter of more than 2.5 mm, large blood vessels and large thrombus. Intracoronary thrombus aspiration can prevent distal embolization. The existence of intra coronary thrombus is also an indication of the provision of Glycoprotein IIb-IIIa inhibitors. The success of overcoming the acute thrombosis, characterized by normal blood flow (TIMI 3 flow) with stenosis <50%. Nikesh Jain et al. Cardiology and Cardiovascular Research 2019; 3(2): 31-36 Oktaviono YH. Folia Medica Indonesiana Vol. 52. 2016 : 66-73
- 72. Dual anti-platelet (DAPT) should be given as early as possible, especially in all patients with acute coronary syndrome patients. Acetylsalicylic acid (ASA) and the P2Y12 receptor antagonists such as clopidogrel, prasugrel and ticagrelor served to increase the effectiveness of treatment and prevention of stent thrombosis. PLATO Trial The effectiveness of Ticagrelor vs Clopidogrel in preventing stent thrombosis The incidence of stent thrombosis could still occur at 0.5-2% in the case of elective PCI and more than 6% in the case of PCI with acute coronary syndromes despite using dual antiplatelet Stent Thrombosis Management ANTI-PLATELET Nikesh Jain et al. Cardiology and Cardiovascular Research 2019; 3(2): 31-36 Oktaviono YH. Folia Medica Indonesiana Vol. 52. 2016 : 66-73
- 73. Selection of anticoagulation during PCI procedures is also important Unfractionated heparin (UFH) is the main option while undergoing PCI. From the research HORIZON-AMI, comparing UFH-Glycoprotein IIa/IIIb with direct thrombin inhibitors bivalirubin as monotherapy, showed a 0.3 vs 1.4%, P <0.001 in the incidence of Acute ST. It is important choose the right size stents and perform high-pressure post-dilation effectively (> 14 atm) To further optimize the prevention ST, lesions calsified, can be handled with the use of rotational atherectomy so that expansion and better positioning stent. The use of intracoronary imaging modalities such as Intra Vascular Ultra Sound (IVUS) and Optical Coherence Tomography (OCT) is very helpful as guiding the expansion and apposition of the stent to be more adequate Stent Thrombosis Management ANTICOAGULANT PROCEDURE OPTIMIZATION Nikesh Jain et al. Cardiology and Cardiovascular Research 2019; 3(2): 31-36 Oktaviono YH. Folia Medica Indonesiana Vol. 52. 2016 : 66-73
- 74. INTEGRATED STRATEGY OF IPST IN THIS PATIENT Patient Characteristic Lession Characteristic Stent Characteristic Male, 49 y.o Insulin treated DM Type II Smoker History of ACS 1 month prior admission CAD 3VD with Left Main Disease Lession length > 20 mm with calcification Multiple stenting Length 38mm Moderate Risk of Early Stent Thrombosis Evidence IPST: Ischemic ECG Changes Thrombus Intracatheter DAPT with Asetyl Salycilic + Ticagrelor High Intensity Statin TIMI Flow 3, residual stenosis 0% ECG returned to baseline No chest discomfort during and post procedure 2nd Generation DES (Everolimus-eluting platinum chromium stent)
- 75. Conclusions Intraprocedural Stent Thrombosis was a strong predictor of mortality in patients undergoing PCI. This case showed that the present widespread use of DES instead of BMS for coronary implantation although decreased the future risk of repeat revascularization, increased the risk of thrombosis. Prior risk stratification, selection of 2nd generation DES, early potent antiplatelet treatment and anticoagulant of choice with UFH might be used to reduce the risk of IPST in patients undergoing stent implantation.
- 76. ISR
- 112. ESC guidelines 2017
- 113. ESC guidelines 2017
- 114. ESC guidelines 2017