Alain Toledano : Small Breast Cancers Radiotherapy : Locoregional Treatments particularities ?
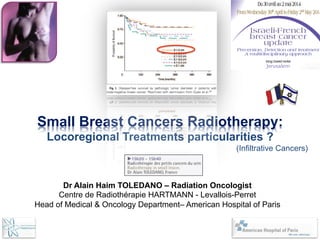
- 1. Small Breast Cancers Radiotherapy: Locoregional Treatments particularities ? (Infiltrative Cancers) Dr Alain Haim TOLEDANO – Radiation Oncologist Centre de Radiothérapie HARTMANN - Levallois-Perret Head of Medical & Oncology Department– American Hospital of Paris
- 2. William HALSTEAD First mastectomy in 1882 . Spread of tumor cells in a contiguous manner . lymph. spreading / extensionà « En bloc » dissection . Ly. diffusion : precursor, instigator of metastases . Node : barrier for tumor cells dissemination . Importance of Nodes Anatomy . Little importance of « bloodstream » in diffusion . Tumor is autonomous, independant of its host . Breast Cancer = Locoregional Desease . Locoregional Treatment : determinant for prognosis . No consideration to tumor multicentricity Hypothesis William HALSTEAD (1894)
- 3. Bernard FISHER NSABP Leader . No orderly pattern of tumor cell dissemination . lymph. spreading/ embolisat°: no « en bloc » dissect° . Ly. diffusion : indicator rather than instigator of mets . Node : Ineffective barrier to tumor cell spread . Regional Lymph Nodes are of Biologic Importance . Importance of « bloodstream » in dissemination . Complexe Host-Tumor: interrelationships, affect disease . Operable Breast Cancer = Systemic Disease . Locoregional Treatment : No impact on Overall Survival . Multicentricity : not necessaryprecursor of cancer dev. Hypothèses Bernard FISHER (1968)
- 4. T = 8 mm SIMPLE MODEL = 1 tumor < 1cm, early diagnosis, did not have time to spread, Therapeutic deflation
- 5. T = 18 mm 1 N+ SIMPLE MODEL = 1 tumor < 1cm, early diagnosis, did not have time to spread, Therapeutic deflation
- 6. T = 38 mm x N+ / M+ Good Theory the more often: so, screening, curative TT without sequellae… SIMPLE MODEL = 1 tumor < 1cm, early diagnosis, did not have time to spread, Therapeutic deflation
- 7. T = 8 mm REALITY = 1 tumor < 1cm, early diagnosis, may have already metastased… x N+ / M+
- 8. T T × . Why 20-30% of Node Negative breast Cancers = Mestastases at 10 ans ? HALSTEAD vs FISHER Which reality small of T ? A third hypothesis « the spectrum thesis » (1994) considers breast cancer to be a heterogeneous disease that can be thought of as a spectrum of proclivities (tendencies) extending from a disease that remains local throughout its course to one that is systemic when first detectable
- 10. Can we decrease aggressivness of small tumors locoregional treatments ? Can we identify sub-groups candidates to Therapeutic deflation ?
- 11. R Radiotherapy + Tamoxifen (n=386) Tamoxifen (n=383) . Phase III trial, randomised, inclusions 1992 – 2000 . 769 patients, 5.6 years median follow-up . Age > 50 years. T < 5 cm (T1, T2). Free Exerese Margins. N- . Stratification : Size (<,>2 cm) . ER . Node Statut . Center . 1572 eligibles patients , 899 refused the study = 57,2% . 159 patients (/769) did not received the 5 years TAM (75/383p arm TAM) NEJM 2004
- 12. RT + Tam Tam Valeur p 5 years Local recurrence Rate - 611 pts T1 0,4% 5,9% < 0,001 5 y Recurrence Number 27 54 8 y Loval Recurrence Rate (n = 86 pts) 3,5% 17,6% < 0,05 5 y axillary recurrence rate 0,5% 2,5% 0,048
- 13. R Radiotherapy + Tamoxifen (n=317) Tamoxifen (n=319) . Phase III trial, randomised, inclusions 1994 – 1999 . 636 patients, 5 years median follow-up . Age > 70 year<s . T1 . Free Exerese Margins . N- . HR+ . Stratification : . Axillary dissection . Age <> 75 ans
- 14. RT + Tam Tam Valeur p 5 y Local Recurrence Rate 1% 4% < 0,001 At 10 years DFS Hugues JCO 2013 98% 90% <0,05 5 y Recurrence Number 2 16 Metastatic Recurrences (n = 86 pts) 7 7 ns Secondary Mastectomy 2 6 ns
- 15. . Phase III trial, randomised, inclusions 1996 – 2004 . 869 patients, 53,8 months median follow-up . Middle Age 66 years . T < 3 cm . Free Margins . HR+ . Gr I,II . N- . Stratification : . Age . Hormo.tt . Node Statut . Grade . Center Radiotherapy + Tam or AI (n=414) Tam or AI (n=417) R
- 16. RT + Ho Ho Valeur p 5y Local recuurence Rate À 6 ans 0,4% 0,4% 5,1% 9% 0,001 5 y Reccurence Number 2 19
- 17. n Phase III trial, randomised n 264 patients, 12,1 years median follow-up n Middle Age > 40 years . T < 2 cm . Free Margins > 1 cm n HR+ . N- . « low agressivity » (Ki 67<10%, phase S < 7%) n Stratification : . Age . Hormon.tt . Node Statut . Grade . Center Radiotherapy Observation R Local Recurrence - 11, 6 % p= 0,0013 - 27,2 %
- 18. Rechute locale RT + Ho Rechute locale Ho Fischer et al. at 8 ans 2,8 % 16,5 % Fyles et al. at 8 ans 3,5 % 17,6 % Hughes et al. at 7 ans 1 % 7 % Potter et al. at 6 ans 0,4 % 9 % Holli et al. at 12 ans 11,6 % 27,2 % Historically : Local recurrence Rate – arm without Radiotherapy : - 35 % RL at 8 years ; Clark , JNCI 1996 - 24 % RL at 10 years ; Liljegren , JCO 1999 Less selected Tumors …
- 19. New breast cancers molecular classifications What is the impact on recurrence ? Genetic Substratum for the different biological profiles Luminal A : RO+ ou RP+ Her2- Luminal B : RO+ou RP+ Her2+ Her2+ : RO- RP-Her2+ Basal : RO-RP-Her2- . 797 patients (Dana-Farber, Massachusetts), fu 70 months . Sub-types : Luminal A, Luminal B, Her2+, Basal Local Recurrences : Her2+ & Basal > Luminal A & B (p=s) Metastases : Her2+ & Basal > Luminal A & B (p=s) N’Guyen et al. JCO 2008 Local Recurrence rate is associated to : Factors HR ajusted IC-95% p-valeur HER-2 9.2 1.6-51 0.012 Triple NEG 7.1 1.6-31 0.009 Nguyen PL et al. JCO 2008;26:2373-8
- 20. Joensuu et al. Clin Cancer Res 2003 pT1a HER2+ / N-‐ T< 1 cm Press et al. J Clin Oncol 15:2894-2904 5-10 mm HER2- HER2+ HER2- HER2- HER2+ HER2+
- 23. Tumorectomy + Radiotherapy Good Cosmetic Results for majority of patients Toledano et al. IJROBP 2007
- 24. Niméus-Malström E et al. Br Cancer Res 2008 All Reccurences are not the same …
- 25. T1 , N0 without systemic treatment : - 90% 10 years - Recurrence Free Survival (RFS) - 75% 10y RFS if Grade III and/or emboles vasc. 1259 ptes T1N0 of NSABP / RFS at 8 ans Surgery alone Surgery + systemic < RE -‐ 81% 90% (chemo) RE + 86% 93% (Tam)
- 26. For 4 locoregional recurrences avoided at 5 years = 1 saved life at 15 years
- 27. Schroen et al. JCO05 Ballast et al. IJROBP06Relation between distance to RT Type of breast surgery for T1 16 40 80 >80
- 28. Irradiation Partial Accelerated 2 concepts : - Irradiation of a partial breast volume - Irradiation hypofractionnated accelerated Up to 30% of women in North America who undergo breast-conserving surgery do not undergo breast irradiation, in part because of the inconvenience of the therapy and its cost.
- 29. French physiologist Claude Bernard, who focused attention on deductive scientific research, and who stated that : Bernard C: Introduction àl’Etude de la Médecine Experimentale. Paris, France, J.B. Bailliere, 1865 “A hypothesis, is the obligatory starting point of all experimental reasoning, and is only of value if it can be tested »
- 30. The American « engouement » for mammosite Abbott et al.(SEER) Cancer 2011 Clinical Application before scientific proof
- 31. CONSENSUS STATEMENT ACCELERATED PARTIAL BREAST IRRADIATION CONSENSUS STATEMENT FROM THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY (ASTRO) BENJAMIN D. SMITH, M.D.,*y DOUGLAS W. ARTHUR, M.D.,z THOMAS A. BUCHHOLZ, M.D.,y BRUCE G. HAFFTY, M.D.,x CAROL A. HAHN, M.D.,k PATRICIA H. HARDENBERGH, M.D.,{ THOMAS B. JULIAN, M.D.,# LAWRENCE B. MARKS, M.D.,** DORIN A. TODOR, PH.D.,z FRANK A. VICINI, M.D.,yy TIMOTHY J. WHELAN, M.D.,zz JULIA WHITE, M.D.,xx JENNIFER Y. WO, M.D.,kk AND JAY R. HARRIS, M.D.{{ *Radiation Oncology Flight, Wilford Hall Medical Center, Lackland AFB, TX; y Department of Radiation Oncology, The University of Texas M. D. Anderson Cancer Center, Houston, TX; z Department of Radiation Oncology, Medical College of Virginia, Virginia Commonwealth University, Richmond, VA; x Department of Radiation Oncology, University of Medicine and Dentistry of New Jersey – Robert Wood Johnson Medical School, New Brunswick, NJ; k Department of Radiation Oncology, Duke University Medical School, Durham, NC; { Shaw Regional Cancer Center, Veil, CO; # Department of Human Oncology, Allegheny General Hospital, Pittsburgh, PA; **Department of Radiation Oncology, University of North Carolina Medical School, Chapel Hill, NC; yy Department of Radiation Oncology, William Beaumont Hospital, Royal Oak, MI; zz Department of Radiation Oncology, Juravinski Cancer Center, Hamilton, ON, Canada; xx Department of Radiation Oncology, Medical College of Wisconsin, Milwaukee, WI; kk Harvard Radiation Oncology Residency Program, Boston, MA; and {{ Department of Radiation Oncology, Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston, MA Purpose: To present guidance for patients and physicians regarding the use of accelerated partial-breast irradia- tion (APBI), based on current published evidence complemented by expert opinion. Methods and Materials: A systematic search of the National Library of Medicine’s PubMed database yielded 645 candidate original research articles potentially applicable to APBI. Of these, 4 randomized trials and 38 prospec- tive single-arm studies were identified. A Task Force composed of all authors synthesized the published evidence and, through a series of meetings, reached consensus regarding the recommendations contained herein. Results: The Task Force proposed three patient groups: (1) a ‘‘suitable’’ group, for whom APBI outside of a clinical trial is acceptable, (2) a ‘‘cautionary’’ group, for whom caution and concern should be applied when considering APBI outside of a clinical trial, and (3) an ‘‘unsuitable’’ group, for whom APBI outside of a clinical trial is not gen- erally considered warranted. Patients who choose treatment with APBI should be informed that whole-breast irradiation (WBI) is an established treatment with a much longer track record that has documented long-term effectiveness and safety. Reprint requests to: Benjamin D. Smith, M.D., 2200 Bergquist Drive, Suite 1, Lackland AFB, TX 78236. Tel: (210) 292-5589; Fax: (210) 292-3773; E-mail: benjamin.smith@lackland.af.mil Supplementary material for this article can be found at www. redjournal.org. This document was prepared by the Accelerated Partial Breast Irradiation Consensus Statement Task Force of the Health Services Research Committee of the American Society for Radiation Oncol- ogy (ASTRO). Before initiation of this Consensus Statement, all members of the Task Group writing the Statement were required to complete conflict of interest statements. These statements are maintained at ASTRO Headquarters in Fairfax, VA, and pertinent conflict information is published with the report. Individuals with disqualifying conflicts have been recused from participation in this Consensus Statement. these guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably di- rected to obtaining the same results. The ultimate judgment regard- ing the propriety of any specific therapy must be made by the physician and the patient in light of all the circumstances presented by the individual patient. ASTRO assumes no liability for the infor- mation, conclusions, and findings contained in its consensus state- ments. In addition, these guidelines cannot be assumed to apply to the use of these interventions performed in the context of clinical tri- als, given that clinical studies are designed to evaluate or validate in- novative approaches in a disease for which improved staging and treatment are needed or are being explored. This Consensus Statement was prepared on the basis of informa- tion available at the time the Task Group was conducting its research and discussions on the topic. There may be new developments that CONSENSUS STATEMENT ACCELERATED PARTIAL BREAST IRRADIATION CONSENSUS STATEMENT FROM THE AMERICAN SOCIETY FOR RADIATION ONCOLOGY (ASTRO) BENJAMIN D. SMITH, M.D.,*y DOUGLAS W. ARTHUR, M.D.,z THOMAS A. BUCHHOLZ, M.D.,y BRUCE G. HAFFTY, M.D.,x CAROL A. HAHN, M.D.,k PATRICIA H. HARDENBERGH, M.D.,{ THOMAS B. JULIAN, M.D.,# LAWRENCE B. MARKS, M.D.,** DORIN A. TODOR, PH.D.,z FRANK A. VICINI, M.D.,yy TIMOTHY J. WHELAN, M.D.,zz JULIA WHITE, M.D.,xx JENNIFER Y. WO, M.D.,kk AND JAY R. HARRIS, M.D.{{ *Radiation Oncology Flight, Wilford Hall Medical Center, Lackland AFB, TX; y Department of Radiation Oncology, The University of Texas M. D. Anderson Cancer Center, Houston, TX; z Department of Radiation Oncology, Medical College of Virginia, Virginia Commonwealth University, Richmond, VA; x Department of Radiation Oncology, University of Medicine and Dentistry of New Jersey – Robert Wood Johnson Medical School, New Brunswick, NJ; k Department of Radiation Oncology, Duke University Medical School, Durham, NC; { Shaw Regional Cancer Center, Veil, CO; # Department of Human Oncology, Allegheny General Hospital, Pittsburgh, PA; **Department of Radiation Oncology, University of North Carolina Medical School, Chapel Hill, NC; yy Department of Radiation Oncology, William Beaumont Hospital, Royal Oak, MI; zz Department of Radiation Oncology, Juravinski Cancer Center, Hamilton, ON, Canada; xx Department of Radiation Oncology, Medical College of Wisconsin, Milwaukee, WI; kk Harvard Radiation Oncology Residency Program, Boston, MA; and {{ Department of Radiation Oncology, Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston, MA Purpose: To present guidance for patients and physicians regarding the use of accelerated partial-breast irradia- tion (APBI), based on current published evidence complemented by expert opinion. Methods and Materials: A systematic search of the National Library of Medicine’s PubMed database yielded 645 candidate original research articles potentially applicable to APBI. Of these, 4 randomized trials and 38 prospec- tive single-arm studies were identified. A Task Force composed of all authors synthesized the published evidence and, through a series of meetings, reached consensus regarding the recommendations contained herein. Results: The Task Force proposed three patient groups: (1) a ‘‘suitable’’ group, for whom APBI outside of a clinical trial is acceptable, (2) a ‘‘cautionary’’ group, for whom caution and concern should be applied when considering APBI outside of a clinical trial, and (3) an ‘‘unsuitable’’ group, for whom APBI outside of a clinical trial is not gen- erally considered warranted. Patients who choose treatment with APBI should be informed that whole-breast irradiation (WBI) is an established treatment with a much longer track record that has documented long-term effectiveness and safety. Reprint requests to: Benjamin D. Smith, M.D., 2200 Bergquist Drive, Suite 1, Lackland AFB, TX 78236. Tel: (210) 292-5589; Fax: (210) 292-3773; E-mail: benjamin.smith@lackland.af.mil Supplementary material for this article can be found at www. redjournal.org. This document was prepared by the Accelerated Partial Breast Irradiation Consensus Statement Task Force of the Health Services these guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably di- rected to obtaining the same results. The ultimate judgment regard- ing the propriety of any specific therapy must be made by the physician and the patient in light of all the circumstances presented by the individual patient. ASTRO assumes no liability for the infor- mation, conclusions, and findings contained in its consensus state- Int. J. Radiation Oncology Biol. Phys., Vol. 74, No. 4, pp. 987–1001, 2009 Copyright Ó 2009 American Society for Radiation Oncology. Published by Elsevier Inc. Printed in the USA. 0360-3016/09/$–see front matter doi:10.1016/j.ijrobp.2009.02.031 consistent with the presence of a mutation, should not receive APBI outside of a clinical trial because of the absence of lit- erature supporting the use of APBI in this setting. Table 2. Patients ‘‘suitable’’ for APBI if all criteria are present Factor Criterion Patient factors Age $60 y BRCA1/2 mutation Not present Pathologic factors Tumor size #2 cm* T stage T1 Margins Negative by at least 2 mm Grade Any LVSI Noy ER status Positive Multicentricity Unicentric only Multifocality Clinically unifocal with total size #2.0 cmz Histology Invasive ductal or other favorable subtypesx Pure DCIS Not allowed EIC Not allowed Associated LCIS Allowed Nodal factors N stage pN0 (i- , i+ ) Nodal surgery SN Bx or ALNDjj Treatment factors Neoadjuvant therapy Not allowed Abbreviations: APBI = accelerated partial-breast irradiation; LVSI = lymph–vascular space invasion; ER = estrogen receptor; DCIS = ductal carcinoma in situ; EIC = extensive intraductal com- ponent; LCIS = lobular carcinoma in situ; SN Bx = sentinel lymph node biopsy; ALND = axillary lymph node dissection. Criteria are derived from data (when available) and conservative panel judgment. Table 3. ‘‘Cautionary’’ group: Any of these criteria should invoke caution and concern when considering APBI Factor Criterion Patient factors Age 50–59 y Pathologic factors Tumor size 2.1–3.0 cm* T stage T0 or T2 Margins Close (<2 mm) LVSI Limited/focal ER status Negativey Multifocality Clinically unifocal with total size 2.1–3.0 cmz Histology Invasive lobular Pure DCIS #3 cm EIC #3 cm Abbreviations as in Table 2. * The size of the invasive tumor component as defined by the American Joint Committee on Cancer (81). y Patients with ER-negative tumors are strongly encouraged to enroll in the National Surgical Adjuvant Breast and Bowel Project B-39/Radiation Therapy and Oncology Group 04-13 clinical trial (78). z Microscopic multifocality allowed, provided the lesion is clini- cally unifocal (a single discrete lesion by physical examination and ultrasonography/mammography) and the total lesion size (including foci of multifocality and intervening normal breast parenchyma) falls between 2.1 and 3.0 cm. APBI consensus statement d B. D. SMITH et al. 991 Table 2. Patients ‘‘suitable’’ for APBI if all criteria are present Factor Criterion t factors e $60 y CA1/2 mutation Not present logic factors mor size #2 cm* tage T1 rgins Negative by at least 2 mm de Any SI Noy status Positive lticentricity Unicentric only ltifocality Clinically unifocal with total size #2.0 cmz tology Invasive ductal or other favorable subtypesx e DCIS Not allowed C Not allowed ociated LCIS Allowed factors tage pN0 (i- , i+ ) dal surgery SN Bx or ALNDjj ment factors oadjuvant therapy Not allowed breviations: APBI = accelerated partial-breast irradiation; = lymph–vascular space invasion; ER = estrogen receptor; Table 3. ‘‘Cautionary’’ group: Any of these criteria should invoke caution and concern when considering APBI Factor Criterion Patient factors Age 50–59 y Pathologic factors Tumor size 2.1–3.0 cm* T stage T0 or T2 Margins Close (<2 mm) LVSI Limited/focal ER status Negativey Multifocality Clinically unifocal with total size 2.1–3.0 cmz Histology Invasive lobular Pure DCIS #3 cm EIC #3 cm Abbreviations as in Table 2. * The size of the invasive tumor component as defined by the American Joint Committee on Cancer (81). y Patients with ER-negative tumors are strongly encouraged to enroll in the National Surgical Adjuvant Breast and Bowel Project B-39/Radiation Therapy and Oncology Group 04-13 clinical trial (78). z Microscopic multifocality allowed, provided the lesion is clini- cally unifocal (a single discrete lesion by physical examination and ultrasonography/mammography) and the total lesion size (including foci of multifocality and intervening normal breast parenchyma) falls between 2.1 and 3.0 cm. APBI consensus statement d B. D. SMITH et al. 991 such patients, relatively few patients of this age have actually enrolled in such trials. Therefore, the Task Force thought that the data were too limited to determine this age cohort’s suit- ability. Few women aged <50 years have been treated with APBI in prospective single-arm studies, and thus, the Task Force strongly recommended against APBI outside of a clin- ical trial for this patient group at this time. It was noted that data from the University of Wisconsin prospective single- arm study indicated that the risk of IBTR may not be exces- sively high among appropriately selected women aged <50 years (76); however, there were only 70 patients aged <50 years in this study, and the median follow-up time was only 48.5 months. Therefore, the panel thought that confir- matory data were required before endorsing off-protocol APBI for this younger patient group. Finally, the Task Force recommended that carriers of deleterious BRCA1 or BRCA2 mutations, or individuals with a personal or family history consistent with the presence of a mutation, should not receive APBI outside of a clinical trial because of the absence of lit- erature supporting the use of APBI in this setting. Regarding pathologic characteristics, the Task Force rec- ommended measuring the maximum size of the invasive Pure DCIS Not allowed EIC Not allowed Associated LCIS Allowed Nodal factors N stage pN0 (i- , i+ ) Nodal surgery SN Bx or ALNDjj Treatment factors Neoadjuvant therapy Not allowed Abbreviations: APBI = accelerated partial-breast irradiation; LVSI = lymph–vascular space invasion; ER = estrogen receptor; DCIS = ductal carcinoma in situ; EIC = extensive intraductal com- ponent; LCIS = lobular carcinoma in situ; SN Bx = sentinel lymph node biopsy; ALND = axillary lymph node dissection. Criteria are derived from data (when available) and conservative panel judgment. * The size of the invasive tumor component as defined by the American Joint Committee on Cancer (81). y The finding of possible or equivocal LVSI should be disre- garded. z Microscopic multifocality allowed, provided the lesion is clini- cally unifocal (a single discrete lesion by physical examination and ultrasonography/mammography) and the total lesion size (including foci of multifocality and intervening normal breast parenchyma) does not exceed 2 cm. x Favorable subtypes include mucinous, tubular, and colloid. jj Pathologic staging is not required for DCIS. * The size of the invasive tumor component as defined by the American Joint Committee on Cancer (81). y Patients with ER-negative tumors are strongly encouraged to enroll in the National Surgical Adjuvant Breast and Bowel Projec B-39/Radiation Therapy and Oncology Group 04-13 clinical tria (78). z Microscopic multifocality allowed, provided the lesion is clini cally unifocal (a single discrete lesion by physical examination and ultrasonography/mammography) and the total lesion size (including foci of multifocality and intervening normal breast parenchyma falls between 2.1 and 3.0 cm. Table 4. Patients ‘‘unsuitable’’ for APBI outside of a clinical trial if any of these criteria are present Factor Criterion Patient factors Age <50 y BRCA1/2 mutation Present Pathologic factors Tumor size* >3 cm T stage T3-4 Margins Positive LVSI Extensive Multicentricity Present Multifocality If microscopically multifocal >3 cm in total size or if clinically multifocal Pure DCIS If >3 cm in size EIC If >3 cm in size Nodal factors N stage pN1, pN2, pN3 Nodal surgery None performed Treatment factors Neoadjuvant therapy If used Abbreviations as in Table 2. If any of these factors are present, the Task Force recommends against the use of APBI outside of a prospective clinical trial. * The size of the invasive tumor component as defined by the American Joint Committee on Cancer (81).
- 33. Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer:5-year results for local control and overall survival from theTARGIT-A randomised trial Jayant SVaidya, FrederikWenz, Max Bulsara, Jeffrey STobias, David J Joseph, Mohammed Keshtgar, Henrik L Flyger, Samuele Massarut, Michael Alvarado, Christobel Saunders,Wolfgang Eiermann, Marinos Metaxas, Elena Sperk, Marc Sütterlin, Douglas Brown, Laura Esserman, Mario Roncadin, AlastairThompson, John A Dewar, Helle M R Holtveg, Steffi Pigorsch, Mary Falzon, Eleanor Harris, April Matthews, Chris Brew-Graves, Ingrid Potyka,Tammy Corica, Norman RWilliams, Michael Baum, on behalf of theTARGIT trialists’ group Summary Background The TARGIT-A trial compared risk-adapted radiotherapy using single-dose targeted intraoperative radiotherapy (TARGIT) versus fractionated external beam radiotherapy (EBRT) for breast cancer. We report 5-year results for local recurrence and the first analysis of overall survival. Methods TARGIT-A was a randomised, non-inferiority trial. Women aged 45 years and older with invasive ductal carcinoma were enrolled and randomly assigned in a 1:1 ratio to receive TARGIT or whole-breast EBRT, with blocks stratified by centre and by timing of delivery of targeted intraoperative radiotherapy: randomisation occurred either before lumpectomy (prepathology stratum, TARGIT concurrent with lumpectomy) or after lumpectomy (postpathology stratum, TARGIT given subsequently by reopening the wound). Patients in the TARGIT group received supplemental EBRT (excluding a boost) if unforeseen adverse features were detected on final pathology, thus radiotherapy was risk-adapted. The primary outcome was absolute difference in local recurrence in the conserved breast, with a prespecified non-inferiority margin of 2·5% at 5 years; prespecified analyses included outcomes as per timing of randomisation in relation to lumpectomy. Secondary outcomes included complications and mortality. This study is registered with ClinicalTrials.gov, number NCT00983684. Findings Patients were enrolled at 33 centres in 11 countries, between March 24, 2000, and June 25, 2012. 1721 patients were randomised to TARGIT and 1730 to EBRT. Supplemental EBRT after TARGIT was necessary in 15·2% [239 of 1571] of patients who received TARGIT (21·6% prepathology, 3·6% postpathology). 3451 patients had a median follow-up of 2 years and 5 months (IQR 12–52 months), 2020 of 4 years, and 1222 of 5 years. The 5-year risk for local recurrence in the conserved breast was 3·3% (95% CI 2·1–5·1) for TARGIT versus 1·3% (0·7–2·5) for EBRT (p=0·042). TARGIT concurrently with lumpectomy (prepathology, n=2298) had much the same results as EBRT: 2·1% (1·1–4·2) versus 1·1% (0·5–2·5; p=0·31). With delayed TARGIT (postpathology, n=1153) the between-group difference was larger than 2·5% (TARGIT 5·4% [3·0–9·7] vs EBRT 1·7% [0·6–4·9]; p=0·069). Overall, breast cancer mortality was much the same between groups (2·6% [1·5–4·3] for TARGIT vs 1·9% [1·1–3·2] for EBRT; p=0·56) but there were significantly fewer non-breast-cancer deaths with TARGIT (1·4% [0·8–2·5] vs 3·5% [2·3–5·2]; p=0·0086), attributable to fewer deaths from cardiovascular causes and other cancers. Overall mortality was 3·9% (2·7–5·8) for TARGIT versus 5·3% (3·9–7·3) for EBRT (p=0·099). Wound-related complications were much the same between groups but grade 3 or 4 skin complications were significantly reduced with TARGIT (four of 1720 vs 13 of 1731, p=0·029). Interpretation TARGIT concurrent with lumpectomy within a risk-adapted approach should be considered as an option for eligible patients with breast cancer carefully selected as per the TARGIT-A trial protocol, as an alternative Lancet 2014; 383: 603–13 Published Online November 11, 2013 http://dx.doi.org/10.1016/ S0140-6736(13)61950-9 This online publication has been corrected.The corrected version first appeared atthelancet.com on February 14, 2014 See Comment page 578 Copyright ©Vaidya et al. Open Access article distributed under the terms of CC BY-NC-ND ClinicalTrialsGroup, Division of Surgery and Interventional Science, University College London, London, UK (Prof J SVaidya PhD, C Brew-Graves MSc, I Potyka PhD, M Metaxas PhD, N RWilliams PhD, Prof M Baum MD); Department of RadiationOncology (Prof FWenz MD, E Sperk MD), and Department ofGynecology andObstetrics (Prof M Sütterlin MD), University MedicalCentre Mannheim, University of Heidelberg, Heidelberg, Germany; Department of Biostatistics, University of Notre Dame, Fremantle,WA, Australia (Prof M Bulsara PhD); Department of Radiation Oncology (Prof D J Joseph FRACR, T Corica BSc), and Department of Surgery (Prof C Saunders FRACS), www.thelancet.com Vol 383 February 15, 2014 603 Summary Background The TARGIT-A trial compared risk-adapted radiotherapy using single-dose targeted intraoperative radiotherapy (TARGIT) versus fractionated external beam radiotherapy (EBRT) for breast cancer. We report 5-year results for local recurrence and the first analysis of overall survival. Methods TARGIT-A was a randomised, non-inferiority trial. Women aged 45 years and older with invasive ductal carcinoma were enrolled and randomly assigned in a 1:1 ratio to receive TARGIT or whole-breast EBRT, with blocks stratified by centre and by timing of delivery of targeted intraoperative radiotherapy: randomisation occurred either before lumpectomy (prepathology stratum, TARGIT concurrent with lumpectomy) or after lumpectomy (postpathology stratum, TARGIT given subsequently by reopening the wound). Patients in the TARGIT group received supplemental EBRT (excluding a boost) if unforeseen adverse features were detected on final pathology, thus radiotherapy was risk-adapted. The primary outcome was absolute difference in local recurrence in the conserved breast, with a prespecified non-inferiority margin of 2·5% at 5 years; prespecified analyses included outcomes as per timing of randomisation in relation to lumpectomy. Secondary outcomes included complications and mortality. This study is registered with ClinicalTrials.gov, number NCT00983684. Findings Patients were enrolled at 33 centres in 11 countries, between March 24, 2000, and June 25, 2012. 1721 patients were randomised to TARGIT and 1730 to EBRT. Supplemental EBRT after TARGIT was necessary in 15·2% [239 of 1571] of patients who received TARGIT (21·6% prepathology, 3·6% postpathology). 3451 patients had a median follow-up of 2 years and 5 months (IQR 12–52 months), 2020 of 4 years, and 1222 of 5 years. The 5-year risk for local recurrence in the conserved breast was 3·3% (95% CI 2·1–5·1) for TARGIT versus 1·3% (0·7–2·5) for EBRT (p=0·042). TARGIT concurrently with lumpectomy (prepathology, n=2298) had much the same results as EBRT: 2·1% (1·1–4·2) versus 1·1% (0·5–2·5; p=0·31). With delayed TARGIT (postpathology, n=1153) the between-group difference was larger than 2·5% (TARGIT 5·4% [3·0–9·7] vs EBRT 1·7% [0·6–4·9]; p=0·069). Overall, breast cancer mortality was much the same between groups (2·6% [1·5–4·3] for TARGIT vs 1·9% [1·1–3·2] for EBRT; p=0·56) but there were significantly fewer non-breast-cancer deaths with TARGIT (1·4% [0·8–2·5] vs 3·5% [2·3–5·2]; p=0·0086), attributable to fewer deaths from cardiovascular causes and other cancers. Overall mortality was 3·9% (2·7–5·8) for TARGIT versus 5·3% (3·9–7·3) for EBRT (p=0·099). Wound-related complications were much the same between groups but grade 3 or 4 skin complications were significantly reduced with TARGIT (four of 1720 vs 13 of 1731, p=0·029). Interpretation TARGIT concurrent with lumpectomy within a risk-adapted approach should be considered as an option for eligible patients with breast cancer carefully selected as per the TARGIT-A trial protocol, as an alternative to postoperative EBRT. Funding University College London Hospitals (UCLH)/UCL Comprehensive Biomedical Research Centre, UCLH Charities, National Institute for Health Research Health Technology Assessment programme, Ninewells Cancer Campaign, National Health and Medical Research Council, and German Federal Ministry of Education and Research. Introduction Adjuvant whole-breast external beam radiotherapy (EBRT) is deemed mandatory after lumpectomy for breast cancer on the basis of the reduction of local recurrence in the conserved breast and of breast cancer mortality.1 Even in highly selected patients, omission of radiotherapy increases the risk of local recurrence.2–5 To develop a more refined and personalised approach to adjuvant radiotherapy, we designed the TARGIT-A (TARGeted Intraoperative radioTherapy Alone) trial.6 The Lancet 2014; 383: 603–13 Published Online November 11, 2013 http://dx.doi.org/10.1016/ S0140-6736(13)61950-9 This online publication has been corrected.The corrected version first appeared atthelancet.com on February 14, 2014 See Comment page 578 Copyright © Vaidya et al. Open Access article distributed under the terms of CC BY-NC-ND ClinicalTrials Group, Division of Surgery and Interventional Science, University College London, London, UK (Prof J SVaidya PhD, C Brew-Graves MSc, I Potyka PhD, M Metaxas PhD, N RWilliams PhD, Prof M Baum MD); Department of Radiation Oncology (Prof FWenz MD, E Sperk MD), and Department of Gynecology and Obstetrics (Prof M Sütterlin MD), University Medical Centre Mannheim, University of Heidelberg, Heidelberg, Germany; Department of Biostatistics, University of Notre Dame, Fremantle,WA, Australia (Prof M Bulsara PhD); Department of Radiation Oncology (Prof D J Joseph FRACR, T Corica BSc), and Department of Surgery (Prof C Saunders FRACS), Sir Charles Gairdner Hospital, Perth,WA, Australia; Department of Clinical Oncology (Prof J STobias FRCR), and Department of Pathology (M Falzon FRCPath), University College London Hospitals, London, UK; Department of Surgery, Royal Free Hospital, London, UK (Prof M Keshtgar PhD, Prof J S Vaidya); Department of Surgery,Whittington Hopsital, TARGIT stratum (figure 3; appendix). In the postpathology stratum—ie, when TARGIT was delivered as a delayed procedure by reopening the lumpectomy cavity, 1153 patients—the difference in local recurrence in the conserved breast between the two groups was larger than 2·5%: TARGIT 5·4% (95% CI 3·0–9·7) vs EBRT 1·7% (0·6–4·9; p=0·069). Breast-cancer mortality was three patients for TARGIT versus one patient for EBRT (1·2%, 0·4–4·2 vs 0·5%, 0·1–3·5; p=0·35), and non- breast-cancer mortality was five patients for TARGIT versus eight patients for EBRT (1·58%, 0·62–3·97 vs 1·76%, 0·7–4·4; p=0·32). Thus, in absolute terms, there were eight additional local recurrences and one less death in the postpathology TARGIT stratum (figure 3). The results of a comparison26 of cumulative incidence for local recurrence in the presence of competing risks (death and withdrawal from trial) were no different from Kaplan-Meier estimates, showing that these risks did not bias the main results (data not shown). Analysis limited to the mature cohort, first reported in 2010 (n=2232, median follow-up now 3 years 7 months), in which most events had occurred (32 of 34 local recurrences and 85 of 88 deaths), yielded much the same results (data not shown). Table 3 shows the Z score and pnon-inferiority for the primary outcome of local recurrence in the conserved breast, for the whole cohort, the mature cohort, and the earliest cohort. Non-inferiority is established for the whole cohort and for prepathology patients but not for post- pathology patients. Figure 4 shows the primary (local recurrence in the conserved breast) and secondary outcomes (deaths) for the prepathology stratum. It shows the differences in 5-year estimates for these outcomes for the whole cohort, There were fewer grade 3 or 4 radiotherapy-related skin complications with TARGIT than with EBRT (four of 1721 vs 13 of 1730, p=0·029). In post-hoc exploratory analyses, we noted no sig- nificant difference in 5-year risk of regional recurrence Number at risk TARGIT EBRT 0 1679 1696 1 1251 1244 2 963 956 3 679 674 4 491 479 5 290 296 0 5 10 Recurrence(%) A Local recurrence Log-rank p=0·042 TARGIT 23 events EBRT 11 events Number at risk TARGIT EBRT 0 1679 1696 1 1251 1243 2 966 957 3 683 676 4 495 481 5 294 297 0 5 10 Recurrence(%) B Regional recurrence Log-rank p=0·609 TARGIT 8 events EBRT 6 events Number at risk TARGIT EBRT 0 1721 1730 1 1285 1272 2 997 978 3 706 693 4 514 496 5 309 302 Years 0 5 10 Mortality(%) C Death Log-rank p=0·099 TARGIT 37 events EBRT 51 events Figure 2: Kaplan-Meier analysis of local recurrence in the conserved breast, regional recurrence (axillary and supraclavicular), and deaths Local recurrence wasthe primary outcome, death was a secondary outcome, regional recurrence was an exploratory outcome.Three ofthe 14 regional recurrences had breast recurrence as well (oneTARGIT andtwo EBRT). (A) Local TARGIT EBRT Other cancers 8 16 Cardiovascular causes Cardiac* 2 8 Stroke 0 2 Ischaemic bowel 0 1 Other† 7 8 Total 17 35 5-year risk 1·4% forTARGIT versus 3·5% for EBRT; log-rank p=0·0086. TARGIT=targeted intraoperative radiotherapy. EBRT=external beam radiotherapy. *Included one “sudden death at home” in EBRT group. †TARGIT: two diabetes, one renal failure, one liver failure, one sepsis, one Alzheimer’s disease, one unknown; EBRT: one myelopathy, one perforated bowel, one pneumonia, one old age, four unknown. The patient and tumour characteristics and trial profile are in the appendix. The risk-adapted design is shown in the trial profile—eg, of the 1140 patients allocated TARGIT in the prepathology stratum, 219 received TARGIT and EBRT as per protocol, because they were shown to have characteristics of high-risk disease postoperatively (appendix). There was no significant difference between prepathology and postpathology in the timing of delivery of EBRT (p=0·58). Most cancers were small and of good prognosis (87% [2685 of 3082] were up to 2 cm, 85% [2573 of 3032] grades 1 or 2, 84% [2610 of 3112] node negative, 93% [2874 of 3093] oestrogen-receptor positive and 82% [2462 of 3016] progesterone-receptor positive) and detected by screening 69% [2102 of 3063]. The appen- dix shows tumour characteristics and main results as per treatment received. 93·7% [3234 of 3451] of patients were seen within the year before datalock or had at least 5 years of follow- up (appendix). The whole cohort of 3451 patients had a median follow-up of 2 years and 5 months (IRQ 12–52 months), 2020 patients had a median follow- up of 4 years, and 1222 patients had a median follow-up of 5 years. The mature cohort of 2232 patients, which was originally reported in 2010, had a median follow up of 3 years and 7 months (IRQ 30–61 months). Table 1 shows detailed results for the local recurrence in the conserved breast (primary outcome), any other recurrence (exploratory outcome), and death (secon- dary outcome). The 5-year risks for local recurrence in the conserved breast for TARGIT versus EBRT were 3·3% (95% CI 2·1–5·1) versus 1·3% (0·7–2·5; p=0·042). Breast cancer mortality was much the same in the two groups: 2·6% (1·5–4·3) for TARGIT versus 1·9% (1·1–3·2) for EBRT (p=0·56), but there were significantly fewer non-breast- cancer deaths in the TARGIT group than the EBRT group (1·4%, 0·8–2·5 vs 3·5%, 2·3–5·2; p=0·0086), attributable to fewer deaths from cardiovascular causes and other cancers (figure 1, table 2). Overall mortality for TARGIT was 3·9% (2·7–5·8) versus 5·3% (3·9–7·3) for EBRT (p=0·099). Overall, in absolute terms, there were 12 additional local recurrences but 14 fewer deaths in the TARGIT group (figures 1, 2). Despite the poor prognostic factors for survival in the group selected to receive TARGIT plus EBRT, as shown by the increased breast cancer mortality (8·0%, 95% CI 3·5–17·5), local recurrence was low in that group (0·9%, 0·1–6·1), and did not differ from those who received TARGIT alone (appendix). In the prepathology stratum—ie, when TARGIT was delivered during the initial lumpectomy, 2298 patients— the risk of local recurrence in the conserved breast was much the same for TARGIT as for EBRT: TARGIT 2·1% (95% CI 1·1–4·2) versus EBRT 1·1% (0·5–2·5; p=0·31). Breast-cancer mortality was 17 patients for TARGIT 5 10 rtality(%) A Breast cancer deaths B Non-breast cancer deaths Log-rank p=0·56 Log-rank p=0·0086 TARGIT 20 events EBRT 16 events TARGIT 17 events EBRT 35 events Events; 5-year cumulative risk (95%CI) Absolute difference* TARGIT EBRT All patients Local recurrence (n=3375) 23; 3·3% (2·1–5·1) 11; 1·3% (0·7–2·5) 12 (2·0%) Any other recurrence (n=3375) 46; 4·9% (3·5–6·9) 37; 4·4% (3·0–6·4) 9 (0·5%) Death (n=3451) 37; 3·9% (2·7–5·8) 51; 5·3%(3·9–7·3) –14 (–1·4%) Prepathology† Local recurrence (n=2234) 10; 2·1% (1·1–4·2) 6; 1·1% (0·5–2·5) 4 (1·0%) Any other recurrence (n=2234) 29; 4·8% (3·1–7·3) 25; 4·7% (3·0–7·4) 4 (0·1%) Death (n=2298) 29; 4·6% (1·8–6·0) 42; 6·9% (4·3–9·6) –13 (–2·3%) Postpathology‡ Local recurrence (n=1141) 13; 5·4% (3·0–9·7) 5; 1·7%(0·6–4·9) 8 (3·7%) Any other recurrence (n=1141) 17; 5·2% (3·0–8·8) 12; 3·7% (1·9–7·0) 5 (1·5%) Death (n=1153) 8; 2·8% (1·3–5·9) 9; 2·3% (1·0–5·2) –1 (0·5%) TARGIT=targeted intraoperative radiotherapy. EBRT=external beam radiotherapy. *In Kaplan-Meier point estimate at 5 years (TARGIT minus EBRT). †TARGIT given at same time as lumpectomy. ‡TARGIT given after lumpectomy, as separate procedure. Table 1: Results of primary (local recurrence in the conserved breast), secondary (death), and exploratory (any other recurrence) outcomes for all patients and the two strata as per timing of randomisation and delivery ofTARGIT www.thelancet.com Vol 383 February 15, 2014 603 results for local recurrence and the first analysis of overall survival. Methods TARGIT-A was a randomised, non-inferiority trial. Women aged 45 years and older with invasive ductal carcinoma were enrolled and randomly assigned in a 1:1 ratio to receive TARGIT or whole-breast EBRT, with blocks stratified by centre and by timing of delivery of targeted intraoperative radiotherapy: randomisation occurred either before lumpectomy (prepathology stratum, TARGIT concurrent with lumpectomy) or after lumpectomy (postpathology stratum, TARGIT given subsequently by reopening the wound). Patients in the TARGIT group received supplemental EBRT (excluding a boost) if unforeseen adverse features were detected on final pathology, thus radiotherapy was risk-adapted. The primary outcome was absolute difference in local recurrence in the conserved breast, with a prespecified non-inferiority margin of 2·5% at 5 years; prespecified analyses included outcomes as per timing of randomisation in relation to lumpectomy. Secondary outcomes included complications and mortality. This study is registered with ClinicalTrials.gov, number NCT00983684. Findings Patients were enrolled at 33 centres in 11 countries, between March 24, 2000, and June 25, 2012. 1721 patients were randomised to TARGIT and 1730 to EBRT. Supplemental EBRT after TARGIT was necessary in 15·2% [239 of 1571] of patients who received TARGIT (21·6% prepathology, 3·6% postpathology). 3451 patients had a median follow-up of 2 years and 5 months (IQR 12–52 months), 2020 of 4 years, and 1222 of 5 years. The 5-year risk for local recurrence in the conserved breast was 3·3% (95% CI 2·1–5·1) for TARGIT versus 1·3% (0·7–2·5) for EBRT (p=0·042). TARGIT concurrently with lumpectomy (prepathology, n=2298) had much the same results as EBRT: 2·1% (1·1–4·2) versus 1·1% (0·5–2·5; p=0·31). With delayed TARGIT (postpathology, n=1153) the between-group difference was larger than 2·5% (TARGIT 5·4% [3·0–9·7] vs EBRT 1·7% [0·6–4·9]; p=0·069). Overall, breast cancer mortality was much the same between groups (2·6% [1·5–4·3] for TARGIT vs 1·9% [1·1–3·2] for EBRT; p=0·56) but there were significantly fewer non-breast-cancer deaths with TARGIT (1·4% [0·8–2·5] vs 3·5% [2·3–5·2]; p=0·0086), attributable to fewer deaths from cardiovascular causes and other cancers. Overall mortality was 3·9% (2·7–5·8) for TARGIT versus 5·3% (3·9–7·3) for EBRT (p=0·099). Wound-related complications were much the same between groups but grade 3 or 4 skin complications were significantly reduced with TARGIT (four of 1720 vs 13 of 1731, p=0·029). Interpretation TARGIT concurrent with lumpectomy within a risk-adapted approach should be considered as an option for eligible patients with breast cancer carefully selected as per the TARGIT-A trial protocol, as an alternative to postoperative EBRT. Funding University College London Hospitals (UCLH)/UCL Comprehensive Biomedical Research Centre, UCLH Charities, National Institute for Health Research Health Technology Assessment programme, Ninewells Cancer Campaign, National Health and Medical Research Council, and German Federal Ministry of Education and Research. Introduction Adjuvant whole-breast external beam radiotherapy (EBRT) is deemed mandatory after lumpectomy for breast cancer on the basis of the reduction of local recurrence in the conserved breast and of breast cancer mortality.1 Even in highly selected patients, omission of radiotherapy increases the risk of local recurrence.2–5 To develop a more refined and personalised approach to adjuvant radiotherapy, we designed the TARGIT-A (TARGeted Intraoperative radioTherapy Alone) trial.6 The November 11, 2013 http://dx.doi.org/10.1016/ S0140-6736(13)61950-9 This online publication has been corrected.The corrected version first appeared atthelancet.com on February 14, 2014 See Comment page 578 Copyright ©Vaidya et al. Open Access article distributed under the terms of CC BY-NC-ND ClinicalTrialsGroup, Division of Surgery and Interventional Science, University College London, London, UK (Prof J SVaidya PhD, C Brew-Graves MSc, I Potyka PhD, M Metaxas PhD, N RWilliams PhD, Prof M Baum MD); Department of RadiationOncology (Prof FWenz MD, E Sperk MD), and Department ofGynecology andObstetrics (Prof M Sütterlin MD), University MedicalCentre Mannheim, University of Heidelberg, Heidelberg, Germany; Department of Biostatistics, University of Notre Dame, Fremantle,WA, Australia (Prof M Bulsara PhD); Department of Radiation Oncology (Prof D J Joseph FRACR, T Corica BSc), and Department of Surgery (Prof C Saunders FRACS), SirCharlesGairdner Hospital, Perth,WA, Australia; Department ofClinical Oncology (Prof J STobias FRCR), and Department of Pathology (M Falzon FRCPath), University College London Hospitals, London, UK; Department of Surgery, Royal Free Hospital, London, UK (Prof M Keshtgar PhD, Prof J SVaidya); Department of Surgery,Whittington Hopsital,
- 34. Table 6. Randomized trials comparing whole-beast irradiation with APBI Trial N Median follow-up (y) Lumpectomy cavity definition Arms IBTR Tumor bed failure LRF CSS OS TARGIT 779 0.98 Intraoperative assessment (1) Whole-breast RT* . . . . . (2) APBI: IORT delivering 20 Gy to cavity surface with 50-kV photons . . . . . NIC, Hungary 258 5.5 Surgical clips (1) Whole-breast RT: 50 Gy in 25 fractions using either Cobalt-60 (n =29) or 6–9-MV photons (n = 100)y 3.4% (4/130) 1.7% (2/130) . 96% 91.8% (2) APBI: HDR interstitial implant to 36.4 Gy in 7 fractions b.i.d. (n = 88) or external-beam RT with electrons to 50 Gy in 25 daily fractions (n = 40).z PTV defined as lumpectomy cavity + 2 cm 4.7% (6/128) 1.6% (2/128) . 98.3% 94.6% At 5 y p = 0.50 At 5 y p = NR At 5 y p = NR At 5 y p = NR YBCG 174 8 ‘‘A combination of preoperative information if available, scar position, and patient recollection’’ (1) Whole-breast RT: 40 Gy in 15 fractions followed by boost of 15 Gy in 5 fractions 4% (4/90) . 9% (8/90) . 73% (2) APBI: 55 Gy in 20 fractions using external-beam techniques.x PTV not defined 12% (10/84) 8% (7/84) 24% (20/84) . 70% At 8 y At 8 y At 8 y At 8 y p = 0.07 p = NR p = 0.05{ p = 0.75 Christie Hospital 708 5.4 Not specified (1) Whole-breast RT: 40 Gy in 15 fractions without a boost 11.0% (24/355) . . . 71% (2) APBI: 40–42.5 Gy in 8 fractions using 8–14-MeVjj electrons to an average field size of 8 Â 6 cm. PTV constituted the entire quadrant of the index lesion 19.6% (52/353) . . . 73% At 7 y p < 0.001{ At 7 y p = NR Abbreviations: LRF = local–regional failure; CSS = cause-specific survival; OS = overall survival; IORT = intraoperative radiotherapy; RT = radiotherapy; HDR = high-dose-rate; NR = not reported; PTV = planning target volume. Full trial names are shown in Table 1. Other abbreviations as in Tables 2 and 5. A period (.) indicates that data were not available. * Details of whole-breast RT not specified. y One patient received a 16-Gy electron boost, and 22 received a dose <50 Gy. z Seven patients received a dose <50 Gy. Although patients treated with electrons received partial-breast irradiation, treatment was given using conventional fractionation and thus was not accelerated. x External-beam techniques included tangents, appositional Cobalt-60 or Cesium-137 teletherapy, or en face electrons (energy not reported). jj Electron energy was 10 MeV for most patients and 14 MeV for patients with ‘‘large breasts.’’ { Statistically significant comparison. APBIconsensusstatementdB.D.SMITHetal. Table 7. Comparison of clinical studies by APBI treatment technique Treatment technique Total patients Total follow-up (patient-years) Average follow-up (y) Interstitial 1,321 7,133 5.4 MammoSite 1,787 4,110 2.3 Intraoperative 681 1,430 2.1 External beam 3D-CRT/IMRT 319 335 1.0 Protons 40 20 0.5 996 I. J. Radiation Oncology d Biology d PhysicsNSABP B39 : Reexcision T bed with extemporane Negative Margins 134 reexcision : 38% of relectures = positive margins But at > 10 mm : < 10% (n=13) Vicini ; IJROBP 2004
- 35. Which Real target volume for breast Radiotherapy ? Underevaluation of phenomenoms at distance of tumorectomy bed : microenvironment..
- 36. pN+ pN0 Recurrence rate without adjuvant treatment • D’après Early Breast Cancer Trialists’ Collaborative Group 1998 meta-analysis,1 adapté 2 1. Early Breast Cancer Trialists’ Collaborative Group. Lancet. 1998;351:1451. 2. Update of Houghton. J Clin Oncol. 2005;23(16S):24s. Abstract 582. Tauxderécidive annuel(%) 0 4 8 12 16 0 2 4 6 8 10 Années Early Pic Late Pic
- 37. « Tumor size is “Halstedian” in concept … More than 2,000 patients entered into the National Surgical Adjuvant Breast Project were utilized to evaluate the validity of the concept that the size of breast neoplasms influences prognosis. It was concluded that size alone is not as consequential to the fate of the patient as are other factors relative to the tumor and/or host that determine the development of metastases. . . . Since size (ie, growth) is now recognized to be dependent on such factors as the number of proliferating cells, the length of the cycle—which is not always uniform—the extent of cell death or cell loss and the number of nonproliferating cells,. . . it is difficult to relate size to the age of a tumor » « a large tumor that had not metastasized prior to its removal may be considered early and a small one that had already disseminated may be considered late » Bernard FISHER 1970 monograph
- 38. Merci de votre attention
