Problems in late preterm babies, iap bps,bangalore,webinar, 20-5-20 - Dr Karthik Nagesh
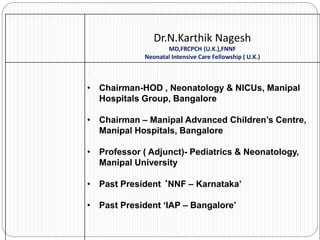
- 1. Dr.N.Karthik Nagesh MD,FRCPCH (U.K.),FNNF Neonatal Intensive Care Fellowship ( U.K.) ’ • Chairman-HOD , Neonatology & NICUs, Manipal Hospitals Group, Bangalore • Chairman – Manipal Advanced Children’s Centre, Manipal Hospitals, Bangalore • Professor ( Adjunct)- Pediatrics & Neonatology, Manipal University • Past President ‘NNF – Karnataka’ • Past President ‘IAP – Bangalore’
- 2. PROBLEMS OF THE LATE PRETERM NEWBORNS
- 3. Panelists Dr. Pradeep G.C.M , Professor & HOD of Neonatology, M.S. Ramaiah Medical College & Hospitals, Bangalore Dr. Vishwanath Kamoji, Consultant Neonatologist & Pediatrician, Columbia Asia Hospital, Hebbal, Bangalore Dr. Nandini Nagar, Consultant Neonatologist & Pediatrician, Cloudnine Hospital, Jayanagar, Bangalore
- 4. NICU Growth in Karnataka - Three Decad
- 5. About 1000 SNCUs+NICUs **India needs 20 000–30 000 level 3 NICU beds and 75 000–100 000 level 2 SNCU beds….
- 7. EPIDEMIOLOGY Every year, an estimated 15 million babies are born preterm and this number is rising Approximately 1 million children die each year due to complications of preterm birth Late preterm births - increasing trend ( about 6-9% of Births and 71 % of all Preterms). Morbidity & Mortality more in late preterms compared to terms
- 9. Problems Of The Late Preterms
- 11. Morbidity of Late Preterm Infants Sapiro-mendoza CK et al, Pediatrics 2008
- 13. The Late Preterm – Physiologic Immaturity Transient Tachypnea of the Newborn(TTNB) Respiratory Distress Syndrome(RDS) Persistent Pulmonary Hypertension(PPHN) Respiratory Failure Jaundice Hypoglycemia Thermoregulation Problems Feeding Difficulties Neuro – Developmental Impairment
- 15. Adverse neonatal outcome – Early term Babies
- 18. NICU admission - by Weeks of gestation 0 5 10 15 20 25 30 35 14 10 12.3 34.8 40 wks- 17/127 39wks- 10/113 38wks- 14/120 37wks- 15/43
- 19. RDS by weeks of gestation 0 5 10 15 20 25 4.7 4.4 4.1 23.2 40wks- 6/127 39wk s- 5/113 38wks -5/120 37 wks- 10/43
- 21. COMPLICATIONS Temperature Instability RDS Feeding Difficulties Hypoglycemia Hyperbilirubinemia Apnea Neonatal Sepsis Prolonged Hospital Stay Readmission
- 22. Respiratory issues in late preterm Prof Pradeep GCM M.S.Ramaiah Medical College Bengaluru
- 23. Introduction Studies have consistently shown that late preterm infants have higher respiratory morbidity and mortality compared with full-term infants Incidence of respiratory distress in late preterm is 28.9% as compared to term( 4.2%) 35 weeks’ gestation are nine fold more likely, to have respiratory distress compared with babies born at term
- 24. Respiratory Manifestation Etiology of respiratory distress is diverse and includes Transient tachypnea of the newborn RDS Persistent pulmonary hypertension Apnea
- 25. Need for Mechanical Ventilation
- 26. Respiratory Manifestation Why late preterm infants are at risk for developing respiratory distress?
- 27. Management Antenatal Steroids Close monitoring for respiratory distress Early respiratory support / Surfactant
- 28. Thank you !
- 29. ISSUES OF THERMOREGULATION & HYPOGLYCEMIA IN LATE PRETERMS DR PRIYA SHIVALLI DCH, DNB, FELLOWSHIP IN NEONATOLOGY (IAP) CONSULTANT NEONATOLOGIST & PEDIATRICIAN VAGUS SUPERSPECIALITY HOSPITAL BENGALURU
- 30. Acute complications of late preterm birth. Wang ML, Dorer DJ, Fleming M, et al. Clinical outcomes of near-term infants. Pediatrics. 2004;114:372–376.
- 31. Hypothermia is more common than we think – A silent killer! In low income and middle income countries (LMICs) prevalence in community settings ranges from 11%- 92%, in hospital setting ranges from 8%- 85%. Independently associated with increased mortality 1.6 to 1.9 times. Hypothermia can cause a Healthy baby to become ill and a sick baby to deteriorate dramatically.
- 32. PREDISPOSING FACTORS IN LATE PRETERMS Larger surface area per unit body weight Decreased thermal insulation due to lack of subcutaneous fat Reduced brown adipose tissue (Nonshivering thermogenesis) Decreased tone
- 36. Prevention and Management In Delivery room Thermoneutral environment Kangaroo mother care Clothing / Swaddling Incubators / Radiant warmer Polyethylene plastic wraps If Temp <36deg C Swaddle baby and cover head with a cap If after 30 mins, <36degC Place under radiant warmer If still <36degC Shift to NICU Further evaluation and treatment Measure temperature every hour for first 6hrs Then minimum of every 6hrs until discharge
- 38. KANGAROO MOTHER CARE BENEFITS Improved survival Temperature regulation Physiologic stability Reduced Sepsis Pain reduction Sleep organisation Improved growth Improved breastfeeding Early discharge Increased IQ
- 39. The Effects of Skin-to-Skin Care on Late Preterm and Term Infants At-Risk for Neonatal Hypoglycemia Arpitha Chiruvolu, Kimberly Miklis and Veeral Tolia Pediatrics May 2018, 142 ABSTRACT Objective: The objective of this study was to evaluate the effects of prolonged skin-to-skin care (SSC) during blood glucose monitoring (12–24 hours) in late preterm and term infants at-risk for neonatal hypoglycemia (NH). Study design: We conducted a retrospective pre- and postintervention study. We compared late preterm and term infants at-risk for NH born in a 1-year period before the SSC intervention, May 1, 2013, to April 30, 2014 (pre-SSC) to at-risk infants born in the year following the implementation of SSC intervention, May 1, 2014, to April 30, 2015 (post-SSC). Results: The number of hypoglycemia admissions to neonatal intensive care unit among at-risk infants for NH decreased significantly from 8.1% pre-SSC period to 3.5% post-SSC period (P = 0.018). The number of infants receiving intravenous dextrose bolus in the newborn nursery also decreased significantly from 5.9% to 2.1% (P = 0.02). Number of infants discharged exclusively breastfeeding increased from 36.4% to 45.7%, although not statistically significant (P = 0.074). Conclusion: This SSC intervention, as implemented in our hospital, was associated with a significant decrease in newborn hypoglycemia admissions to neonatal intensive care unit. The SSC intervention was safe
- 40. EMBRACE - WARMER BEMPU –Monitors temperature with alarm
- 41. HYPOGLYCEMIA IN LATE PRETERMS Incidence of hypoglycemia is inversely proportional to gestational age Glucose levels fall 1-2 hrs after birth In late preterm infants: Immature hepatic glycogenolysis Decreased adipose tissue lipolysis Deficient hepatic gluconeogenesis and ketogenesis Hepatic enzyme immaturity
- 44. DEFINITION Operational threshold Blood glucose level of < 40 mg/dL WHO – BGL OF < 45 mg/Dl Transitional Neonatal Hypoglycemia- TNH Normal physiological adaptation to postnatal life.
- 45. SCREENING ‘AT RISK’ Neonate Preterm <37 weeks Small for gestational age (SGA) Large for gestational age (LGA) Infant of diabetic mother (IDM)
- 46. TIME SCHEDULE OF BLOOD GLUCOSE MONITORING CATEGORY OF INFANTS TIME SCHEDULE At risk neonates 2, 6, 12, 24, 48 and 72 hrs of life Sick neonates ( sepsis, asphyxia, polycythemia, shock during acute phase of illness ) Every 6 – 8 hrly Neonates on parenteral nutrition Initial 72hrs: every 6-8hrs After 72hrs: once a day AIIMS PROTOCOL 2019
- 47. DIAGNOSIS Point of care-Glucometer Measures whole blood glucose Error prone Lab glucose estimation – plasma glucose level ( 10-15% more than whole BGL) Glucose oxidase method, Fluoride tubes preferred Continuous glucose monitoring sensor (CGMS) Experimental
- 48. J Pediatr, 2010 Aug;157(2):198-202.e1. Continuous Glucose Monitoring in Newborn Babies at Risk of Hypoglycemia Deborah L Harris1, Malcolm R Battin, Philip J Weston, Jane E Harding Abstract Objective: To determine the usefulness of continuous glucose monitoring in babies at risk of neonatal hypoglycemia. Study design: Babies >/=32 weeks old who were at risk of hypoglycemia and admitted to newborn intensive care received routine treatment, including intermittent blood glucose measurement using the glucose oxidase method, and blinded continuous interstitial glucose monitoring. Results: Continuous glucose monitoring was well tolerated in 102 infants. There was good agreement between blood and interstitial glucose concentrations (mean difference, 0.0 mmol/L; 95% CI, -1.1-1.1). Low glucose concentrations (<2.6 mmol/L) were detected in 32 babies (32%) with blood sampling and in 45 babies (44%) with continuous monitoring. There were 265 episodes of low interstitial glucose concentrations, 215 (81%) of which were not detected with blood glucose measurement. One hundred seven episodes in 34 babies lasted >30 minutes, 78 (73%) of which were not detected with blood glucose measurement. Conclusion: Continuous interstitial glucose monitoring detects many more episodes of low glucose concentrations than blood glucose measurement. The physiological significance of these previously undetected episodes is unknown.
- 49. AAP GUIDELINES
- 50. TABLE TO CALCULATE GLUCOSE INFUSION RATE IN NEONATES
- 52. Lancet 2013 Dec 21;382(9910):2077-83. Dextrose Gel for Neonatal Hypoglycaemia (The Sugar Babies Study): A Randomised, Double-Blind, Placebo-Controlled Trial Deborah L Harris1, Philip J Weston2, Matthew Signal3, J Geoffrey Chase3, Jane E Harding4 Abstract Background: Neonatal hypoglycaemia is common, and a preventable cause of brain damage. Dextrose gel is used to reverse hypoglycaemia in individuals with diabetes; however, little evidence exists for its use in babies. We aimed to assess whether treatment with dextrose gel was more effective than feeding alone for reversal of neonatal hypoglycaemia in at-risk babies. Methods: We undertook a randomised, double-blind, placebo-controlled trial at a tertiary centre in New Zealand between Dec 1, 2008, and Nov 31, 2010. Babies aged 35-42 weeks' gestation, younger than 48-h-old, and at risk of hypoglycaemia were randomly assigned (1:1), via computer-generated blocked randomisation, to 40% dextrose gel 200 mg/kg or placebo gel. Randomisation was stratified by maternal diabetes and birthweight. Group allocation was concealed from clinicians, families, and all study investigators. The primary outcome was treatment failure, defined as a blood glucose concentration of less than 2·6 mmol/L after two treatment attempts. Analysis was by intention to treat. The trial is registered with Australian New Zealand Clinical Trials Registry, number ACTRN12608000623392. Findings: Of 514 enrolled babies, 242 (47%) became hypoglycaemic and were randomised. Five babies were randomised in error, leaving 237 for analysis: 118 (50%) in the dextrose group and 119 (50%) in the placebo group. Dextrose gel reduced the frequency of treatment failure compared with placebo (16 [14%] vs 29 [24%]; relative risk 0·57, 95% CI 0·33-0·98; p=0·04). We noted no serious adverse events. Three (3%) babies in the placebo group each had one blood glucose concentration of 0·9 mmol/L. No other adverse events took place. Interpretation: Treatment with dextrose gel is inexpensive and simple to administer. Dextrose gel should be considered for first-line treatment to manage hypoglycaemia in late preterm and term babies in the first 48 h after birth.
- 53. ADDITIONAL EVALUATION Recurrent/Resistant Hypoglycemia Refractory Hypoglycemia (>12mg/kg/min GIR) Prolonged hypoglycemia ( >7days) Critical lab sample (<40mg/dL) Insulin, Cortisol, Betahydroxy butarate, FFA Ammonia , Lactate, Urine ketones, reducing substances, GH, TSH, TMS, Urine GCMS Genetic testing - SUR1, KiR6.2 mutations 18F-fluoro- L- DOPA PET scan- pancreas
- 54. Management of Resistant Hypoglycemia Hydrocortisone -5mg/kg/day BD IV Diazoxide – 5-15mg/kg/day TDS PO Octreotide -5-35mcg/kg/day TDS SC Glucagon -0.2mg/kg SC/IM Nifedepine Sirolimus Surgery
- 55. Neonatal Hypoglycemic Brain Injury NHBI involves particularly parieto- occipital cortex and subcortical white matter
- 56. JAMA Pediatr. 2017 Oct; 171(10): 972–983. Association of Neonatal Glycemia With Neurodevelopmental Outcomes at 4.5 Years Christopher J. D. McKinlay, PhD,1,2 Jane M. Alsweiler, PhD,1,2 Nicola S. Anstice, PhD,3 et al1, for the Children With Hypoglycemia and Their Later Development (CHYLD) Study Team Abstract Importance Hypoglycemia is common during neonatal transition and may cause permanent neurological impairment, but optimal intervention thresholds are unknown. Objective To test the hypothesis that neurodevelopment at 4.5 years is related to the severity and frequency of neonatal hypoglycemia. Design, Setting, and Participants The Children With Hypoglycemia and Their Later Development (CHYLD) Study is a prospective cohort investigation of moderate to late preterm and term infants born at risk of hypoglycemia. Clinicians were masked to neonatal interstitial glucose concentrations; outcome assessors were masked to neonatal glycemic status. The setting was a regional perinatal center in Hamilton, New Zealand. The study was conducted from December 2006 to November 2010. The dates of the follow-up were September 2011 to June 2015. Participants were 614 neonates born from 32 weeks’ gestation with at least 1 risk factor for hypoglycemia, including diabetic mother, preterm, small, large, or acute illness. Blood and masked interstitial glucose concentrations were measured for up to 7 days after birth. Infants with hypoglycemia (whole-blood glucose concentration <47 mg/dL) were treated to maintain blood glucose concentration of at least 47 mg/dL. Exposures Neonatal hypoglycemic episode, defined as at least 1 consecutive blood glucose concentration less than 47 mg/dL, a severe episode (<36 mg/dL), or recurrent (≥3 episodes). An interstitial episode was defined as an interstitial glucose concentration less than 47 mg/dL for at least 10 minutes. Main Outcomes and Measures Cognitive function, executive function, visual function, and motor function were assessed at 4.5 years. The primary outcome was neurosensory impairment, defined as poor performance in one or more domains. Results In total, 477 of 604 eligible children (79.0%) were assessed. Their mean (SD) age at the time of assessment was 4.5 (0.1) years, and 228 (47.8%) were female. Those exposed to neonatal hypoglycemia (280 [58.7%]) did not have increased risk of neurosensory impairment (risk difference [RD], 0.01; 95% CI, −0.07 to 0.10 and risk ratio [RR], 0.96; 95% CI, 0.77 to 1.21). However, hypoglycemia was associated with increased risk of low executive function (RD, 0.05; 95% CI, 0.01 to 0.10 and RR, 2.32; 95% CI, 1.17 to 4.59) and visual motor function (RD, 0.03; 95% CI, 0.01 to 0.06 and RR, 3.67; 95% CI, 1.15 to 11.69), with highest risk in children exposed to severe, recurrent, or clinically undetected (interstitial episodes only) hypoglycemia. Conclusions and Relevance Neonatal hypoglycemia was not associated with increased risk of combined neurosensory impairment at 4.5 years but was associated with a dose-dependent increased risk of poor executive function and visual motor function, even if not detected clinically, and may thus influence later learning. Randomized trials are needed to determine optimal screening and intervention thresholds based on assessment of neurodevelopment at least to school age.
- 57. TAKE HOME MESSAGES Late preterms experience temperature instability and hypoglycemia mostly in initial 48 hrs. Ineffective thermoregulation in the late preterm infant predisposes the infant to significant complications. Encourage early breast feeding within 1hr of birth and screen for hypoglycemia for 48hrs-72hrs. Early recognition and management prevent short and long term morbidity and mortality. Need to create awareness among health care providers.
- 58. THANK YOU
- 59. Jaundice and dehydration in late preterm neonates Dr. Nandini Nagar Consultant neonatologist and pediatrician Cloudnine hospital, Jayanagar, Bangalore
- 60. Why worry about jaundice in late preterm neonates? Bilirubin levels in late preterm neonates peaks later (at 7 days rather than 5 days) Stays elevated longer Reacher higher mean levels as compared to term neonates (207 micromol/L vs 190 micromol/L) Risk of BIND is higher at lower levels of serum bilirubin as compared to term neonates Risk of BIND doubles for every week below 37 weeks Exclusive breastfeeding increases the risk of extreme hyperbilirubinemia (428 micromol/L) by a factor of 6 Safe discharge of the late preterm infant. R K Whyte, Canadian Pediatric Society, Fetus and Newborn Committee. Pediatr Child Health.2010 Dec; 15(10):655-660
- 61. Feeding difficulties in late preterm - dehydration Late preterm babies adapt quickly to enteral feeds BUT Deglutition, peristaltic function and sphincter function may be immature in the esophagus, stomach and intestines Lead to poor coordination of sucking and swallowing Delay in establishment of breast feeding Excessive weight loss/poor weight gain in the first week - dehydration
- 62. Comparison of short-term outcomes Jaundice requiring phototherapy (18% in late preterm vs 2.5% in term) Hypoglycemia (6.8% vs 0.4%) Respiratory distress (4.2% vs 0.1%) Sepsis (0.4% vs 0.04%) IVH (0.2% vs 0.02%) Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Melamed N, et al. Obstet Gynecol. 2009; 114 (2 Pt 1): 253
- 63. Increased risk of jaundice and BIND Decreased capacity to handle unconjugated bilirubin Decreased hepatic uptake Decreased uridine diphosphoglucuronate glucuronosyl transferase (UGT) activity Increased enterohepatic circulation Delayed postnatal maturation of hepatic bilirubin uptake and conjugation Delayed establishment of enteral feeding
- 64. Copyrights apply
- 65. Copyrights apply
- 66. BIND pontine brainstem oculomotor nuclei globus pallidus auditory pathways Hippocampus Diencephalon subthalamic nuclei Cerebellum vermis - disordered visual gaze (eg, limitations of upward gaze) - sensorineural hearing impairment gait abnormalities (choreoathetoid cerebral palsy) - speech and language disorders - Subtle neuromotor signs are associated with a range of processing disorders due to visuo-oculomotor, auditory, speech, and expressive language disturbances
- 67. MRI brain changes MRI brain imaging shows hyperintense signals in T1 weighted sequences in the globus pallidus, that then shifts to bilateral hyperintense
- 68. Copyrights apply
- 69. predisposed to significant hyperbilirubinemia and other morbidity LAMBS study (Elaine M Boyle et al, ADC, 2015) – Neonatal outcomes and delivery of care for infants born late preterm or moderately preterm: a prospective population- based study Tonse Raju et al, Pediatrics, 2006 – Optimising care and outcome for late preterm (near-term) infants: A summary of the workshop sponsored by the NICHHD Tonse Raju, Pediatrics, 2017 – The “Late Preterm” Birth – Ten Years Later (under Pediatric perspectives) Kumar C et al, J neonatal biology, 2014 – Late Preterm and Early Term Neonates: A New group of high-risk newborn in neonatology with varied complications
- 70. Incidence, course and prediction of significant hyperbilirubinemia (study from Turkey) 219 term and 146 near term newborns 6th hour and daily bilirubin checked until day 7 Late preterms had a 2.4-fold higher risk of developing significant hyperbilirubinemia Day 5 and day 7 serum bilirubin levels were significantly higher in the near-term group Incidence, course and prediction of hyperbilirubinemia in near-term and term newborns. Sarici SU, et al. Pediatrics. 2004; 113(4):775
- 72. - Prospective cohort study including neonates >35 weeks gestation over a period of 6 months from Mar to Aug in 2011 - Risk factors for significant hyperbilirubinemia were identified and serum bilirubin was tested at 36 – 48 hours of age, before discharge - Excluded – NICU admission for any acute illness, Blood group incompatibility, congenital anomalies, those who received IV antibiotics - 486 infants were included in the final analysis, of which 14% developed significant hyperbilirubinemia
- 73. On univariate analysis, serum total bilirubin, gestational age and percentage of weight loss were predictive of significant hyperbilirubinemia On multiple logistic regression, pre-discharge bilirubin had better predictive ability than GA and % of weight loss Most of the late preterms who had jaundice had significant hyperbilirubinemia, and it was statistically significant
- 75. Copyrights apply
- 76. Copyrights apply
- 77. Indications to treat in late preterms without risk factors Phototherapy indications 24 hours of age: >10 mg/dl (171 micromol/L) 48 hours of age: >13 mg/dl (222 micromol/L) 72 hours of age: >15 mg/dl (257 micromol/L) Exchange transfusion indications 24 hours of age: >16.5 mg/dl (282 micromol/L) 48 hours of age: >19 mg/dl (325 micromol/L) >72 hours of age: >21 mg/dl (359 micromol/L) Courtesy: UptoDate
- 78. Indications to treat in late preterms with risk factors Phototherapy indications 24 hours of age: >8 mg/dl (137 micromol/L) 48 hours of age: >11 mg/dl (188 micromol/L) 72 hours of age: >13.5 mg/dl (231 micromol/L) Exchange transfusion indications 24 hours of age: >15 mg/dl (257 micromol/L) 48 hours of age: >17 mg/dl (291 micromol/L) >72 hours of age: >18.5 mg/dl (316 micromol/L) Courtesy: UptoDate
- 79. Phototherapy Exposure to light of wavelength 425 – 475 nm Mechanisms of action: Structural isomerization of bilirubin to lumirubin (major), photo-oxidation to polar molecules, photoisomerization to a less toxic bilirubin isomer Results in a decline in bilirubin by 2 – 3 mg/dl within 4 – 6 hours Greater the spectral power (irradiance X BSA), faster the drop in bilirubin Irradiance of white lights is 8 – 10 microW/cm2/nm, and that of blue LED lights is 30 - 35 microW/cm2/nm
- 80. Monitoring during and after phototherapy Feeding – breast feeding, EBM, donor milk, formula Continuous NG feeds Hydration status, urine output Temperature – LED lights do not cause much overheating Fibre-optic biliblanket can be used during feeding, or in conjunction with LED lights Rebound hyperbilirubinemia
- 83. Double volume exchange transfusion Very rarely performed nowadays In a tertiary care NICU with facilities for central line insertion and ventilation Whole blood required, or red cells of maternal blood group reconstituted with plasma (or O negative red cells with AB negative plasma) Crossmatched, irradiated blood that is negative for all known microorganisms like CMV, HIV, Hep B and C, and syphilis Central lines, preferably UVC, UAC or UVC alone 5 – 10 ml aliquots SBR falls to ½ to ¾ of the pre-exchange value
- 84. IVIG In infants with Rh isoimmune hemolytic disease, in whom SBR is rising despite phototherapy, or is within 2 – 3 gm/dL of the threshold for exchange transfusion Dose – 0.5 to 1 gm/kg over 2 hours Can be repeated if indicated after 12 hours
- 85. Hearing screening Hearing screening preferably using BERA is necessary for neonates that have been treated for significant hyperbilirubinemia, as it can lead to sensorineural hearing loss.
- 86. Key points Late preterm neonates are at a higher risk of delayed establishment of enteral feeding and dehydration Greater risk of significant hyperbilirubinemia and BIND Support early breast feeding, lactation nurses to help Have a low threshold for EBM, donor milk, formula Fortify EBM Continuous NG feeds is a good option if there’s excessive weight loss and jaundice Delay discharge from hospital
- 87. Thank You BENGALURU CHENNAI MUMBAI PUNE GURUGRAM NAVI MUMBAI CHANDIGARH NOIDA Our Locations Website http://cloudninecare.com/
- 88. Feeding, Nutrition and Neurology Late preterm INFANTS
- 89. Feeding- Hypothetical case 34 week old LSCS for PIH 1.6 kg mild respiratory distress. Normal Doppler's How many would start on D10 or TPN with as initial fluid. How many would wait for Mother’s milk, for how long. Would you commence on NG or direct breast feeds as distress resolves?
- 90. Feeding- Hypothetical case This we are considering as a singleton. Gets compounded when you consider Twins and Triplets The majority of them would not go to term, and are born around 32-36 weeks for various reasons
- 91. Feeding Preterm infants have functional taste receptors from 18 weeks’ gestation and flavors perception from around 24 weeks’ gestation This may be bypassed by the NG route Suck swallow and breathing coordination- 33-34 weeks
- 92. Feeding: Energy requirement Dextrose Vs PN IV Infusions-27% of LP infants vs 5% of term , very few LP and ET babies will receive parenteral nutrition support^ PN Vs 10% dextrose in LP infants while waiting for maternal milk supply to meet demand and for full enteral feeds to be tolerated * Each day of parenteral support in LP infants has been reported to predict an increase in time to achieve full oral feeds of 2 h (hazard ratio: 0.92; 95% CI: 0.89– 0.95). ^Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical outcomes of near-term infants. Pediatrics 2004;114:372–6. *Alexander T, Bloomfield FH. Nutritional management of moderate–late preterm infants: survey of current practice. J Paediatr Child Health 2018 Aug 27. https:// doi.org/10.1111/jpc.14201.
- 93. Feeding: Which milk? Breast milk Donor Breast milk Formula?? Encourage early BF- within the first hour if possible Encourage Kangaroo Mother care, stimulation of milk production through regular expressing
- 94. Feeding : Problems HYPOGLYCEMIA – is one of the commonest reasons for additional nutritional support in LP infants. 3-4 x higher than term babies and recurrent 50% of hepatic glycogen stores, a key source of glucose in the immediate newborn period, are deposited between 36 and 40 weeks gestation- which these babies lack! HYPERNATREMIA- More common in LP than term babies for the same reasons, associated with wt loss and feeding difficulties. Need to be managed appropriately as discussed
- 95. Feeding: Immediate Problems 3 months Oromotor dysfunction Avoidant feeding Most commonly Choking Spitting 1 year of life Improved, but persist Admission to NICU vs Nursery fared worse with more later admissions
- 96. FLAMINGO study “Feeding in Late And Moderately preterm Infants Nutrition and Growth Outcomes (FLAMINGO): a cohort study with an embedded RCT, double-blind trial in formula-fed infants to investigate the effects of a new infant formula on growth and body composition.” 140 subjects in the RCT, with an anticipated 250 subjects in the cohort study. Each subject will be included from randomisation until study end for a maximum of 25 months, comprising of a 6-7 month intervention period in the RCT and a follow up period until a corrected age of 24 months of age. Recruitment is expected to be completed in April 2022. Aim to see if early provision of a different formula makes a difference to these babies Supported by Danone / Nutricia
- 97. Feeding: ESPGHaN Recommendations Breast feed & support Hypoglycemia IVF/ TPN Robust Unit Policies Rooming in /care Temp control/ BEMPU Discharge policies- May need to be individualised Further
- 98. Feeding: Vitamins/ Minerals AAP/ ESPGHAN Recommendations Fe for six months Vit D through early childhood • MULTIVITS • CALCIUM PHOSPHATE • Vit D At full feeds/ 2 weeks •IRON At 4-6 weeks • FORTIFIERS esp <1500g For adequate calories
- 99. Brain growth and development Occurs in very specific orders and time frames. It also occurs at different rates during different gestational ages, which creates critical periods of development during which cells are susceptible to insults or injuries. Injury in critical period of growth and differentiation can change the trajectory of brain development, resulting in different patterns of brain injury and repair which manifest as unique neurologic outcomes. Brain growth has been shown to be altered simply by being born preterm, as evidenced by studies showing differences in magnetic resonance imaging (MRI) between late preterm and FTI* . *Walsh JM, Doyle LW, Anderson PJ, et al. Moderate and late preterm birth: effect on brain size and maturation at term-equivalent age. Radiology 2014;273:232–40.
- 100. Brain growth and development The late preterm brain is still immature and more likely to experience noxious stimuli from medical complications after birth such as RDS, sugars,apneas hyperbilirubinemia etc Evidence from animal models reveals that these factors can promote or precipitate neuronal cell death in the immature brain*. There is some evidence that it is unable to defend against such toxicities. *Bhutta AT, Anand KJ. Abnormal cognition and behavior in preterm neonates linked
- 101. MRI* 38-44 week Measures of brain size, BPD, and other brain structures such as the deep grey nuclei, cerebellum, and corpus callosum were smaller in MLPT infants than in full-term infants Measures of the extra-axial spaces, namely interhemispheric distance and superior extra-axial distance, were significantly larger in MLPT infants than in control infants (P , .001), suggesting the presence of larger cerebrospinal fluid volumes in MLPT infants. With regard to brain maturation, MLPT infants had less mature gyral folding and less complete myelination of the posterior limb of the internal capsule at term-equivalent age. *Walsh JM, Doyle LW, Anderson PJ, et al. Moderate and late preterm birth: effect on brain size and maturation at term-equivalent age. Radiology 2014;273:232–40.
- 102. MRI* 38-44 week *Walsh JM, Doyle LW, Anderson PJ, et al. Moderate and late preterm birth: effect on brain size and maturation at term-equivalent age. Radiology 2014;273:232–40.
- 103. MRI* 38-44 week *Walsh JM, Doyle LW, Anderson PJ, et al. Moderate and late preterm birth: effect on brain size and maturation at term-equivalent age. Radiology 2014;273:232–40.
- 104. neurodevelopment 36% • Dev delay • Disability 50% • Risk of SEN in school 10 x • As many children than EPT Compared to Full term Infants
- 105. Early outcomes @ CGA 2 yrs Compared to FTI, LPI performed worse in cognitive, language, and motor domains, with greatest disparity in the language domain. They also showed evidence of poorer social–emotional competence. Remain at a greater risk of Speech and Language delay Generally LPI do not automatically qualify for early intervention Many researchers have hypothesized that the worse neurodevelopmental outcomes of LPI may have to do with their more complicated medical courses compared to FTI.
- 106. SCHOOL AGE outcomes LPI scored lower in reading in kindergarten and first grade. Children delivered late preterm had a 30% higher adjusted odds of needing special and individualised education plan than those born full term. Low IQs, Language skills. Less attention span
- 107. ADOLESCENT AND ADULT outcomes Mainly from Sweden, Denmark – 25-50 yrs old Difficult to extrapolate considering the leaping advances of neonatology in those years.
- 108. Neurodev-Unanswered queries Are delays time bound or permanent Is there an opportunity to intervene for better outcomes. Which LPIs are at highest risk Are there specific delays that are common or are they global
- 109. General Measures in Improving Neurodevelopment in the preterm Design of space with room for KMC Light – have a dark or QUIET TIME / no procedure time Sound- Speak in low tone. Alarms, telephone tones, creaky cupboards / Incubator pots and doors/to be adjusted to minimise sund. Activity level- Maintain Calm, quite and soothing atmosphere Olfactory inputs- remove noxious and unfamiliar senses- spray/ nicotine / scents
- 110. General Measures in Improving Neurodevelopment in the preterm Bed / Clothes- Nesting/ swaddling. Positioning- support and facilitate physiologically well-aligned positions whether the infant is on the back, tummy or side. Feeding and Burping- From early on time the infant’s feeding to be supportive of the infant’s sleep and wake cycles so that the infant may learn to recognize feelings of hunger and satiation. Support the parent to breastfeed the infant. Bloods- Sucrose / breast feeding Medical equipments- tapes/ NG/ Nasal canula to
- 111. Issues in LPT Short Term Morbidities Health Care Costs Hospital Stays Re-Hospitalization
- 112. DISCHARGE CRITERIA Vital signs normal for 12hrs before discharge Passage of 1 stool spontaneously Adequate urine output 24 hours of successful breast feeding If wt loss >7% in 48hr- further assessment before discharge Risk assessment plan for jaundice for infants discharged within 72hr of birth Mother & caregivers demonstrate competency in care of the infant
- 114. How do Antenatal Steroids Work? Science Accelerate development of pneumocytes, thus improving lung mechanics (maximal lung volume, compliance) and gas exchange Increases surfactant production Induction of surfactant release, absorption of alveolar fluid, increase lung antioxidant enzymes Reduction in RDS, moderate to severe RDS Reduction in Intraventricular hemorrhage, Necrotising enterocolitis, mortality, systemic sepsis
- 115. LPT – Way Forward ! ‘Evidence Based’ Practice Guidelines Accurate Dating – Pregnancy, Fetal Maturity Antenatal Steroids – Extended use ( NNT-35)
Notas del editor
- Until recently, we have classified infants by GA in : Preterm, Term and post-term, however due to difference in their physiology, development, morbidity, mortality and long term outcome, we are using a new terminology to describe the GA: preterm, LPT, ET and term.
- Although survival of MLPT babies is excellent, these babies constitute a much larger proportion of the health care burden related to prematurity than do extremely preterm babies
- Nutritional guidelines and requirements for late or moderately preterm (LMPT) infants are notably absent although they represent the largest population of preterm infants. Although survival of MLPT babies is excellent, these babies constitute a much larger proportion of the health care burden related to prematurity than do extremely preterm babies
- If you say one thing and you colleague says anything else, you are not alone. These differences are seen world wide, with physicians commencing on Iv fluids, gradually increasing the NG feeds and then to oral feeds in varying combinations depending on the baby’s clinical condition. Whilst waiting for full milk feeds to be tolerated, there are no data on whether the provision of dextrose alone is sufficient, despite the inevitable catabolism and accumulating nitrogen deficit , or whether babies should receive parenteral nutrition containing protein. All of these approaches are in use around the world. These difficulties in feeding delay their discharge from the hospital.
- What the parents see is a well formed baby with beautiful 10 tiny fingers and toes, rosy cheeks and a normally breathing baby- they want to go home! And that is despite you spending time with them explaining issues related to feeding.
- Most nutrition guidelines provide recommendations for more preterm (< 32/40) or very low birth weight neonates (< 1500 g) but few provide nutritional recommendations for LP and ET babies !! There is little evidence regarding whether PN is more beneficial than 10% dextrose in LP infants while waiting for maternal milk supply to meet demand and for full enteral feeds to be tolerated but its use in LP infants appears to be rare *
- MLPT babies inevitably experience a delay between birth and the establishment of full enteral feeds due to immature suck/swallow/breathe coordination, immature gut motility, and delayed supply of sufficient breastmilk. In absence of breast feeds they can be offred feeds via palada/ cup to help with suck/ swallow coordination.
- These infants are also prone to develop nutritionally related neonatal morbidities such as hypoglycaemia, poor feeding, dehydration and malnutrition in the early neonatal period In utero, there’s a constant supply of glucose which is abruptly halted when the cord is cut.
- Compared with their term-born peers, it observed that infants born LMPT were at increased risk of oral motor problems, such as chewing, biting, and swallowing, and refusal/picky eating, such as selective eating, eating too little or too slowly, or having a poor appetite at 2 y corrected age.
- Mothers of LMPT preterm infants should receive qualified, extended lactation support, and frequent follow-up. Health care providers should remain vigilant for evidence of poor breast milk transfer and infant problems related to poor intake. Individual feeding plans should also include special considerations to compensate for immature feeding skills and difficulties in establishing lactation and breastfeeding.
- Iron- <2500 g - 1 to 2 mg/kg/d & < 2000 g should receive 2 to 3 mg/kg/d - up to 6 months age. LMPT infants require a daily vitamin D supplement of at least 400 IU/d throughout early childhood.
- Most of the research into brain sequelae of preterm birth has been in children and young adults born very preterm (ie, , 32 weeks of gestation at birth) yet the burden of prematurity is mostly in moderate and late preterm (MLPT) infants (those born with ges- tational ages between 32 weeks and zero days and 36 weeks and 6 days), who account for approximately 80% of all preterm births (3,4).
- This demonstrates that LPI have academic challenges that persist through elementary school.