Diagnostic Testing for Bacterial STDs and UTIs
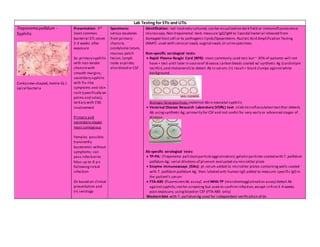
- 1. Lab Testing for STIs and UTIs Treponema pallidum - Syphilis Corkscrew-shaped,motile G(-) spiral bacteria Presentation: 3rd most common bacterial STI;onset 2-3 weeks after exposure Sx: primary syphilis with non-tender chancrewith smooth margins; secondary syphilis with flu-like symptoms and skin rash (specifically on palms and soles); tertiary with CNS involvement Primary and secondary stages most contagious Females: possible transiently bacteremic without symptoms; can pass infection to fetus up to 8 yrs followinginitial infection Dx based on clinical presentation and (+) serology Specimens: serous exudates from primary chancre, condyloma latum, mucous patch lesion,lymph node aspirate; also blood or CSF Identification: not routinely cultured; can be visualized on dark field or immunofluorescence microscopy.Non-treponemal tests measure IgG/IgM to lipoidal material released from damaged host cell or to pathogenic lipids/lipoproteins.Nucleic Acid Amplification Testing (NAAT) used with cervical swab,vaginal swab,or urinespecimen. Non-specific serological tests: Rapid Plasma Reagin Card (RPR): most commonly used test but ~ 30% of patients will not have + test until later in courseof disease; carbon beads coated w/ synthetic Ag (cardiolipin lecithin,and cholesterol) to detect Ab in serum; (+) result= black clumps againstwhite background. Biologic falsepositives:maternal Ab in neonatal syphilis Venereal Disease Research Laboratory (VDRL) test: slidemicroflocculation testthat detects Ab usingsynthetic Ag; primarily for CSF and not useful for very early or advanced stages of disease Ab-specific serological tests: TP-PA: (Treponema pallidumparticleagglutination):gelatin particles coated with T. pallidum pallidum Ag; serial dilutions of ptserum evaluated via microtiter plate Enzyme immunoassays (EIAs): pt serum added to microtiter plates containingwells coated with T. pallidum pallidum Ag, then labeled anti-human IgG added to measure specific IgGin the patient’s serum FTA-ABS (fluorescentAb assay) and MHA-TP (microhemagglutination assay) detect Ab againstsyphilis;notfor screening but used to confirm infection,except in first3-4 weeks post-exposure, usingblood or CSF (FTA-ABS only) Western blot with T. pallidumAg used for independent verification of dx
- 2. Neisseria Gonorrhoeae- Gonorrhea “Bean-shaped” G(-) diplococci with flattened sides adjacent sides,cell wallsappear outlined Presentation: 2nd most common bacterial STI and causeof urethral discharge;onset 2 - 3 d after exposure Sx: intense dysuria and purulent discharge;may be asymptomatic Uncomplicated Gonorrhea: infection of columnar epithelial cells in mucosal membranes of lower genital tract Other presentations: Oropharyngeal, anorectal,ocular Specimens: Genital tract, urine(firstvoid), anal area, oropharynx, conjunctiva, Bartholin’s glands, fallopian tubes, endometrium, blood,jointfluid, skin lesions, neonate gastric contents 30 – 60% males have frequent co- infection w/ C. trachomatis; recommend test for syphilisand HIV Collection Method: Mucosal surface sampled with Dacron swabs - fatty acids in cotton swabs may kill Gonorrhoeae Urethral samples > 1 hr after urination Discard anorectal swabs contaminated w/ fecal material and repeat Culture: should always beperformed to test for β-lactamaseproduction Media: inoculation directly onto media and incubated at 35 – 37° C in CO2 enriched atmosphere Chocolateagar supplemented w/ IsoVitaleX (supplies factors Vand X) – nonselectivemedia for cultivation Modified Thayer-Martin (MTM), Martin- Lewis (ML) and New York City (NYC) media - selectivemedia for use with samples containingnormal flora Non-culture methods: ELIZA and nucleic acid test (NAAT) Transport: rapidly loses viability in buffered, nonnutritive transportmedia Storage: CO2 enriched environment when incubator not available Identification: Patient samples may have large# PMNs, some having intracellular G(-) diplococci;numbers of intracellular pathogen low in both early and late phases of infection Male: presumptive Dx based on patient hx, clinical signs & symptoms, and G(-) diplococci within PMNs Female: urogenital tract contains flora closely resemblingN. Gonorrhoeae; G(-) results only presumptive until confirmed by (+) culture or (+) PCR
- 3. Chlamydiatrachomatis G(-) Nonmotile G(-) coccobacillary organisms lined up likea “school of fish” Presentation: Most common bacterial STI and most common causeof urethral discharge;most frequently reported STI in U.S. Sx: most asymptomatic but if symptoms arepresent, onset 1-3 weeks after exposure Females: may have abnormal vaginal dischargeor burningduring urination;if spread to fallopian tubes then may have lowback or abdominal pain;cervical infection can spread to rectum Males:may have urethral itching/burning,discharge,or burning duringurination Two forms: Elementary bodies (EB): small,dense spherical bodies with diameter of 0.6 – 0.4 µm; extracellular formand is infectious Reticulate bodies (RB): larger cocci with diameter of 0.6 – 1.0 µm; intracellular formthatis metabolically activewithin host cell Culture and Identification: Difficultto culture; culture usingHeLa or McCoy host cells in tissue culture(second most sensitivetest) Presence of inclusion bodies differential for C.trachomatis vs.C. psittici or C.pneumoniae PCR based tests most sensitive DFA staining3rd mostsensitivefor detection Non-culture methods: ELIZA and nucleic acid test(NAAT) Rapid tests areavailableto detect Ab against C.trachomatis strains L1, L2, and L3 that causelymphogranuloma venereum; may yield false positiveresults dueto cross-reactivity with other C. trachomatis strains,so resultmustbe confirmed with more sensitivetesting standards
- 4. Non-gonococcal urethritis (NGU): Onset 10 -14 d, less severe Sx than Gonorrhea (often asymptomatic) > 100,000 (105) = UTI/ bacteruria 104 – 105 = possiblebacteruria 103 – 104 = suspect, retest and use clean catch < 103 = normal levels and any bacteria likely normal flora Urine sedimentation rate: ~ 75% of patients with UTIs will havemore than 100 WBCs/mL of urine Gram stain:1-2 bacteria per 1000x microscopic field yieldspresumptive dx of bacteruria Escherichia coli G(-) Rare causeof urethral discharge Group 1: produces acid by fermentation of lactosein Bacturcultmedium – resultis yellow E. coli, Citrobacter, Enterobacter, Streptococci, Enterococci Urine specimen must be transported to lab within 30 minutes to prevent falsely elevated counts – E. coli generation time ~ 20 min. Bacturcult test: Culture medium supplyingnutrients for growth of various species of aerobic bacteria Proteus swarminginhibited by para-nitropheyl glycerol Contains phenol red indicator,which turns yellowin presence of acid and red in alkalineconditions Pure cultures: discretecolonies with detectable characteristics produced by medium; presumptive differentiation into 3 groups Group 1: ferments lactoseand produces acid yellow medium Group 2: produce rose to orange medium Group 3: alkalineconditions magenta medium Mixed cultures should be checked for divergent characteristicsand may indicatecontamination;especially common in females when urine stream contacts external genitalia Mixed cultures with less than 1000 bacteria /mL of urine= contamination (1 species normally dominant) Limits of Bacturcult test: presumptive results,color changes can be masked by drug effects (dyes, antibacterials),results may vary based on condition of patient and viability of bacteria in specimen,the results must be evaluated in lightof total clinical information obtained,and mixed cultures may produce inconclusivecolor changes thatdo not directly correlatewith relativeproportion of bacteria in the sample Enterobacter G(-) Citrobacter G(-) Proteus G(-) Group 3: produces alkalineconditions in Bacturcultmedium – resultis magenta (purple-red) Proteus and Pseudomonas Pseudomonas G(-) Klebsiella pneumoniae G(-) Group 2: conditions produced by these bacteria (includingsomePseudomonas species and some Enterococci species) resultin rose to orange coloration of Bacturcultmedium Klebsiella pneumoniae, Staphylococci, Streptococci and Enterococci, Pseudomonas Enterococci G(+) Streptococcus G(+) Staphylococcus G(+) Uristix 4 Reagent Strips: strips contain 4 separatereagent zones to test for presence of glucose, protein, nitrite and leukocytes in urine Glucose: glucoseoxidaseand peroxidaseenzymes present catalyzereaction of color change rangingfrom green to brown Protein: at constant pH, yellow is protein (-) and any color rangingfromyellow-green to green to blue-green is protein (+) Nitrite: at acidicpH,dietary nitrate is converted to nitriteby G(-) bacteria in urine,producinga pink color Leukocytes: production of a purplecolor indicates thepresence of granulocytic leukocytes containingesterases thatcatalyzehydrolysis of chromogenic ester substrates on test strip; presumptive test indicatingpresenceof PMNs – PMN content must be verified and pathogen must be identified