Benign diseases of the lower reproductive tract.pptx
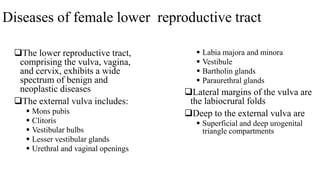
- 1. Diseases of female lower reproductive tract The lower reproductive tract, comprising the vulva, vagina, and cervix, exhibits a wide spectrum of benign and neoplastic diseases The external vulva includes: Mons pubis Clitoris Vestibular bulbs Lesser vestibular glands Urethral and vaginal openings Labia majora and minora Vestibule Bartholin glands Paraurethral glands Lateral margins of the vulva are the labiocrural folds Deep to the external vulva are Superficial and deep urogenital triangle compartments
- 5. Benign diseases of the vulva • Developmental abnormalities • Infectious conditions
- 6. Developmental abnormalities Congenital Vulvar hypoplasia, hyperplasia or duplication Clitoral enlargement o Clitoromegally noted at birth is suggestive of fetal exposure to excessive adrogens It is defined as a clitoral index greater than 10mm2. Labial fusion Acquired Labial hypertrophy Labial fusion Female genital mutilation Epidermal inclusion cysts
- 7. Labial hypertrophy • Labial width — Labia minora hypertrophy is generally described as protuberant labial tissue that projects beyond the labia majora. • In current practice, a stretch width of greater than 6 cm is generally felt to be consistent with hypertrophy
- 8. Labial fusion Also termed labial agglutination or adhesion Prevalence Prepubertal girls→1-5% Female infants→10% Cause is unknown Hypoestrogenism It is seen in infants and young girls and tends to undergo spontaneous resolution at puberty The diagnosis is made visually Treatment 1. Expectant management If the patient is asymptomatic, no intervention is necessary 2. Medical management Estrogen cream therapy 3. Manual separation 4. Surgical separation
- 9. Infectious conditions Bacterial Syphilis Granuloma Inguinale Lymphogranuloma Venereum (LGV) Chancroid Tuberculosis Viral Condyloma Acuminatum Herpesvirus Molluscum Contagiosum Varicella (Herpes Zoster) Cytomegalovirus Fungal Vulvar candidiasis Pityriasis versicolor Parasitic Pediculosis pubis, or pubic lice
- 10. Tuberculosis It most commonly affects the fallopian tubes and endometrium Fallopian tubes are involved in 90–100 % of cases Endometrium in 50-70% of cases Vulvar or vaginal TB Exceedingly rare(1–2 %) Lesions can be ulcerative or hyperplastic
- 11. Condyloma Acuminatum It is an exophytic lesion caused by infection with HPV Most commonly types 6 and 11 It is sexually transmitted disease When it is detected in a child, sexual abuse must be considered The lesions are usually asymptomatic and frequently multiple and multifocal It is not considered premalignant and do not progress to HSILs or carcinoma Management Topical agents Application of dilute podophyllin,imiquimod, or concentrated halogenated acetic acid (trichloroacetic acid) Electrosurgery, cryosurgery, laser ablation, or surgical excision Larger lesions and those refractory to topical treatments The overall recurrence rate is reported as 20–30%
- 13. Molluscum Contagiosum It is a viral infection of the skin Caused by a poxvirus (molluscum contagiosum virus) The lesions are small, raised, and usually white, pink, or flesh-colored with a dimple or pit in the center They’re usually smooth and firm Treatment options Curettage Cryosurgery Topical agents
- 14. Herpesvirus HSV type 2 is more common in vulvar infection Painful, erythematous swelling of the vulva, followed by the eruption of clusters of papules and vesicles which evolve into exquisitely painful ulcers Untreated, the ulcers of the initial episode heal in approximately 2–6 weeks, after which the virus lies dormant in regional sensory and autonomic ganglia Antiviral agents (acyclovir, valacyclovir,or famcyclovir) Speed healing Decrease viral shedding Decrease the incidence of new lesions
- 16. Inflammatory dermatoses Lichen simplex chronicus Lichen sclerosus Lichen planus Allergic or irritant contact dermatitis Atopic dermatitis Psoriasis Crohn’s disease
- 17. Primary skin lesion Size Description 1 Macules Lesions ≤1 cm They are nonpalpable lesions that vary in pigmentation from the surrounding skin and they have no depression or elevations 2 Patches Lesions > 1 cm 3 Papules Lesions ≤5 mm They are palpable, discrete lesions 4 Plaques Lesions >5 mm Superficial slightly raised lesions, often formed by a confluence of papules 5 Pustules Papules containing purulent material 6 Vesicles Lesions <5 mm Circumscribed skin lesions containing serous material 7 Bullae Lesions ≥ 5 mm Secondary skin lesion 1 Excoriation Superficial, often linear skin erosion caused by scratching 2 Lichenification Increased skin markings and thickening with induration 3 Scale Superficial epidermal cells that are dead and cast off from the skin 4 Crust A dried exudate on the skin surface, either serum, blood or pus or a combination 5 Fissure Deep skin split extending into the dermis 6 Erosion Superficial, focal loss of part of the epidermis 7 Ulceration Focal loss of the epidermis extending into the dermis
- 18. Lichen simplex chronicus It originates from an itch-scratch cycle that leads to chronic trauma It is often the end stage of other dermatologic conditions or irritants Lichen sclerosus, atopic dermatitis, or psoriasis Tight clothing,heat,sweating, or products like antiseptics,body fluids,body soaps,condoms,emollients etc The skin responds by thickening with exaggerated gray, leathery-appearing skin markings termed lichenfication Treatment involves halting the itch-scratch cycle Topical corticosteroid ointments help reduce inflammation Lubricants, such as plain petrolatum or vegetable oil, and cool sitz baths help to restore the skin's barrier function Oral antihistamine use, trimmed fingernails, and cotton gloves worn at night can help decrease scratching during sleep If symptoms fail to resolve, biopsy is indicated to exclude other pathology
- 19. LSC Thickened skin, Exaggerated skin markings
- 20. Lichen Sclerosus (LS) LS classically presents in postmenopausal women and prepubertal girls LS is more common in the premenarchal and postmenopausal years About 1–2% of patients in general gynecologic practice It is currently considered to be an autoimmune condition, occurring in genetically predisposed patients Approximately 20 to 30 % of pts with LS have other autoimmune disorders, such as Graves disease, Diabetes mellitus and SLE
- 21. Diagnosis The characteristic clinical picture and histologic findings typically confirm the diagnosis 1. Symptoms often worsen at night Pruritus-the most common LS with erosions or fissures: Pain Dysuria Dyspareunia 2. Physical examination Excoriations and vulvar skin thickening White atrophic papules The skin generally appears thinned and crinkled Thickened white plaques, areas of erythema, or nodularity should prompt biopsy to exclude preinvasive and malignant lesions
- 22. Vulvar LS 1. The skin is thin,shiny, pale, and wrinkled (parchment- like), with focal ecchymosis 2. There is loss of distinction between the labia majora and minora
- 23. Vulvar LS Note the thin and pale vulvar skin, loss of labia minora architecture, labia minora fusion beneath the clitoris, and hourglass distribution around vulva and anus
- 24. Treatment and surveillance Curative therapies are not available for lichen sclerosus Rx goals are symptom control and prevention of anatomic distortion 1. Vulvar Hygiene 2. Ultrapotent topical corticosteroids 3. Surgery o Reserved for complicated cases Introital stenosis Symptomatic clitoral adhesions Malignant transformation develops in 5% of pts Surveillance Every 6 to 12 months for life time Persistently symptomatic, new, or changing lesions are biopsied
- 25. Treatment 1. Vulvar Hygiene Avoid using gels, perfumed bath products, moisturizing wipes, and soaps, as they may contain irritants Avoid douching Use aqueous creams to clean the vulva and thoroughly rinse with tepid water Avoid using a harsh washcloth to clean the vulva After bathing, sparingly apply an emollient, such as plain petrolatum, to moist vulva epithelium Dab the vulva gently to dry Avoid wearing tight-fitting pants Select white cotton underwear Avoid washing undergarments in commercial washing detergents. Wash and rinse these items separately and Consider using a multirinse process with cold water to remove any remaining detergent residue Consider wearing skirts and no underwear at home and at night to avoid friction and aid drying 2. Ultrapotent topical corticosteroids First-line therapy 3. Surgery Reserved for complicated cases Introital stenosis Symptomatic clitoral adhesions
- 26. Lichen planus Involves both cutaneous and mucosal surfaces It affects 1-2 % of general population Symptoms Chronic vaginal discharge with intense vulvovaginal pruritus Burning pain Dyspareunia Postcoital bleeding Physical examination Papules classically are brightly erythematous or violaceous,flat-topped, shiny polygons Vaginal erosions can produce adhesions and synechiae, which may lead to vaginal obliteration Diagnosis Confirmed by biopsy
- 27. Vulvar erosive lichen planus Erythema and erosions on the vulvar labial mucosa
- 28. Lichen planus Thick, violaceous, hyperkeratotic plaque with a white, lacelike pattern on the surface
- 29. Treatment Vulvar hygiene Pharmacotherapy Ultrapotent topical corticosteroid ointments Systemic steroids Failed topical steroids Surgical adhesiolysis is a last resort
- 30. Contact dermatitis This condition is common and affects all ages It affects approximately 15–54% of women It is classified as allergic or irritant contact dermatitis ACD results from a T cell-mediated, delayed type hypersensitivity (DTH) reaction elicited by the contact of the skin with the offending chemical in individuals who have been previously sensitized to the same chemical ICD is a localized inflammatory skin response that results from direct cytotoxic effect of irritants The presentation of ICD and ACD is variable Acute ICD develops within minutes to hours of the exposure, while those of ACD take 24–48 hours to develop The lesions of ICD tend to be well circumscribed, confined to the area of contact, more likely to be painful, and less likely to develop vesicles and bullae, while those of ACD are more poorly demarcated, more likely to be pruritic, and more likely to develop vesicles and bullae Diagnosis Patch test To identify possible allergen Culture Biopsy
- 31. Treatment of vulvar contact dermatitis 1. Stop offending agents and/or practices 2. Correct vulvar skin barrier function Sitz bath twice daily with plain water Application of plain petrolatum 3. Treat any underlying infection Oral antifungal therapy Oral antibiotic administration 1. Reduce inflammation Topical corticosteroids twice daily for 1-3 weeks 0.05% clobetasol propionate ointment 0.1% triamcinolone ointment Systemic corticosteroids for severe irritation 2. Break the itch-scratch cycle Cool packs(avoid ice packs,which may injure skin) Plain,cold yogurt on a sanitary napkin for 5-10 minutes Consider an SSRI or an antihistamine
- 32. Vulvar contact dermatitis Reaction to povidone-iodine solution Contact sites show symmetric erythema and edema on the vulva, inner thighs, and buttock
- 33. Atopic Dermatitis It is predominantly a disease of childhood With 85% of patients presenting before age 5 with severe pruritic eruption 70% of children show spontaneous remission before they reach adulthood The disease first manifests in adulthood in only 2–8% of patients The frequency of vulvar involvement is unknown Scaly patches with fissuring are evident Diagnosis It is usually established by clinical findings and the appearance on the nongenital skin There is no cure for the disease Symptom control Emollients Topical corticosteroids
- 35. Psoriasis It is a chronic immune-mediated disease Its prevalence is 3.2% Involves the genitalia in 30–40% of patients The median age of onset in women is 25 years Symptoms of vulvar psoriasis Itching Burning Pain Physical examination Classic form Sharply demarcated erythematous papules and plaques covered with silvery scale Treatments are none curative Topical agents for mild disease Immunosuppressive therapy Methotrexate or Cyclosporine Phototherapy
- 36. Psoriasis Raised plaques are seen on the vulva
- 37. Crohn’s disease In vulvar disease concomitant gastrointestinal involvement is present Vulvar Crohn disease is typically asymptomatic Only a minority of patients complain of symptoms Pain Pruritus Discharge Dyspareunia Dysuria Physical examination Swelling of the labia minora and/or majora Deep, linear, “knife-like” ulcerations Treatment Systemic therapy with steroids Topical antibiotics and steroids Surgical resection Refractory lesions
- 38. Vulvar Crohn disease Linear "knife-cut" ulcerations and other lesions often affect inguinal, labiocrural, and interlabial folds
- 39. Vulvar cysts Epithelial inclusion cyst Bartholin cyst and abscess Mucous cyst Gartner duct cyst
- 40. Epithelial inclusion cyst Frequently develop on the vulva More common on the labia majora and clitoris They are benign lesions Treatment Rx is not usually necessary for asymptomatic small cysts Surgical excision If cyst is enlarging, symptomatic, or secondarily infected
- 41. Multiple, mobile, knotty epidermal inclusion cysts line the inner labia majora
- 42. Urethral Diverticulum Classic symptoms associated with urethral diverticula are known as the "3D's" 1) Dysuria 2) Dyspareunia 3) Dribbling(Postvoid) Women may also note recurrent UTI, vaginal wall tenderness, frequency, urgency, and chronic pelvic or urethral pain.
- 43. Urethral diverticulum seen in the anterior vaginal wall
- 44. Bartholin gland duct cyst and abscess Bartholin gland Secrete mucus to provide vaginal and vulvar lubrication Each gland is approximately 0.5 cm in size and drains tiny drops of mucous into a 2.5 cm long duct It open into the vulvar vestibule at about the 5 and 7 o’clock position, distal to the hymenal ring The most common large cyst of the vulva is a cystic dilation of an obstructed Bartholin duct Noninflamed cysts contain sterile, clear, mucinous fluid The underlying cause for obstruction is often unclear It may follow infection, trauma, mucus changes, or congenitally narrowed ducts Bartholin duct cysts and abscesses are fairly common, with a lifetime risk estimated to be 2%
- 45. Bartholin gland duct cyst An asymmetric bulge in the left lower vestibule
- 46. Diagnosis The diagnosis of both Bartholin cyst and abscesses are clinical Cyst It is typically painless, and may be asymptomatic Most are detected during a routine pelvic examination or by the woman herself Larger ones may cause discomfort, typically during sexual intercourse, sitting, or ambulating There is a soft, unilateral,round or ovoid ,painless mass in the posterior aspect of the vaginal introitus, at the site of the gland Abscesses Typically present with severe pain and swelling and patients are unable to walk, sit, or have sexual intercourse There is a large, tender, soft, or fluctuant mass at the site of the gland Abscess cultures Biopsy
- 47. Biopsy… Bartholin gland duct cysts and abscesses Uncommon after menopause and should raise concern for possible neoplasia Bartholin gland carcinoma is rare The median age at diagnosis is 57 years Cyst wall biopsy following cavity drainage to exclude rare Bartholin gland carcinoma is considered for at-risk cases Cysts in women older than 40 years, with solid components, fixation of the cyst or abscess wall to surrounding tissue, or with multiple recurrences are candidates
- 48. Microbiology Bartholin gland abscesses are polymicrobial infections ??? According to recent studies fewer abscesses are polymicrobial MRSA is increasing The single most common pathogen is Escherichia coli Bacteroides,peptostreptococcus species and staphylococcus faecalis are common N.gonorrhoeae and C.trachomatis may also be identified
- 49. Management No intervention is necessary for asymptomatic Bartholin cysts Cysts that are disfiguring or symptomatic are treated Procedures: 1. Incision and drainage The mainstay of treatment is I & D with placement of a Word catheter, under local anesthesia 2. Marsupialization It refers to a procedure whereby a new ductal orifice is created 3. Bartholin gland excision is a definitive treatment Antibiotic therapy Trimethoprim-sulfamethoxazole Amoxicillin-clavulanate + clindamycin Cefixime + clindamycin
- 50. Bartholin gland duct incision and drainage I & D with Word catheter placement I & D is easy to perform It is performed in an outpatient setting It has high risk of recurrence →2 -18 %
- 51. The goal of Bartholin gland duct I and D is to empty the cystic cavity and create a new epithelialized tract(Word catheter ) for gland drainage A 1 cm incision is made using a scalpel with a no. 11 blade to pierce the skin and underlying cyst or abscess wall The incision is placed on the cyst bulge,just outside and parallel to the hymen at 5 or 7 o’clock and medial to the Hart line A deflated Word catheter tip is placed into the empty cyst cavity. A syringe is wed to inject 2 to 3 mL of sterile saline through the catheter hub to inflate the balloon. Inflation should reach a diameter sufficient to keep the catheter from falling out of the incision Word catheter in place Abscess or cyst incision Word catheter
- 52. Bartholin gland duct marsupialization • A vertical or elliptical incision measuring 2 cm is made across the skin overlying the cystic bulge using a scalpel no. 15 blade • The incision is placed just outside and parallel to the hymen at 5 or 7 o‘clock and is positioned medial to Hart line Skin incision.
- 53. Marsupialization • It is performed in the operating room • It takes longer time and is more invasive • It has recurrence rates of 2 to 13 %
- 54. Wound closure The edges of the cyst wall are sutured to adjacent skin edges with interrupted sutures using 2-0 or 3-0 gauge delayed-absorbable sutures Cyst wall sutured open
- 55. Bartholin gland duct excision It is definitive procedure for treatment of both cysts and abscesses Excision must be performed in an operating room Candidates: Symptomatic cysts which repeatedly recur and refill Cysts with solid component Raise concern for malignancy Multilocular cysts Excision carries a high risk of complications Excessive bleeding Hematoma formation Cellulitis Scarring Disfigurement Dyspareunia
- 56. Bartholin abscess management algorithm
- 57. Vulvar mucous cyst • Most commonly seen in the vestibule or labia minora • Excision is curative
- 58. Benign lesions of the urethra • Urethral Prolapse • Urethral Caruncles • Urethral diverticulum
- 59. Urethral prolapse It is the circular eversion of the urethral mucosa through the urethral meatus with vascular congestion and possible strangulation It may occur at any age It is most common in premenarchal children and postmenopausal women It may be related to relative lack of estrogen. Physical examination Large red polypoid mass covered with urethral mucosa with edematous vascular submucosa, protruding from the urethra Histologic examination Cryosurgery is an effective method of treatment
- 60. Urethral prolapse in a young girl
- 61. Urethral Caruncles Caruncles are fleshy, friable, sessile, or polypoid masses that arise in the posterior urethra near the meatus Most patients are postmenopausal Average age of 68 years The etiology is unknown Reduced estrogenisation of urethral smooth muscle Other possible factors include irritation, trauma, and local congestion Caruncles often are asymptomatic Bleeding or dysuria Superficial ulceration Histologic examination Distinguish a caruncle from urethral prolapse Treatment Conservative approach-First line Sitz-baths Topical oestrogens Topical anti-inflammatories or steroids Surgery Severe symptoms after failed conservative management Uncertain diagnosis
- 63. Vulvodynia It is vulvar pain of at least three months duration, without a clear identifiable cause, which may have potential associated factors The prevalence is 3–7% The median age of onset is 28 years Treatments: Symptom relief Sitz baths Topical emollients Topical anesthetics Topical and oral antidepressants Oral neuropathic pain medications such as gabapentin Treatments… Symptom relief…. Elimination of possible irritants and allergens Adjunctive psychotherapy Vestibulectomy It is undertaken in some women with localized vestibulodynia, and short-term follow-up shows 60–85% of patients so treated experience significant relief
- 64. Precursor lesions and malignant tumors of the vulva Vulvar Intraepithelial Neoplasia (VIN) Vulvar cancer
- 65. Vulvar Intraepithelial Neoplasia-VIN HPV DNA has been found in up to 80% of VIN lesions Classification: VIN has three categories of squamous intraepithelial lesions (SIL): 1. Vulvar low-grade SIL (vulvar LSIL,flat condyloma, or HPV effect) 2. Vulvar high-grade SIL (vulvar HSIL, VIN usual type) They are commonly associated with oncogenic HPV infection o Particularly HPV 16 3. Differentiated VIN It tend to be unifocal and are typically found in older, nonsmoking, postmenopausal women in their sixth and seventh decade
- 66. VIN type Clinical presentation Risk factors Vulvar LSIL Formerly VIN 1 1. Flat lesions with basal atypia and koilocytic changes such as condyloma 2. Self-limited ,not precancerous HPV effect Vulvar HSIL Formerly VIN ususal type(VIN 2,VIN 3,Vulvar CIS) 1. Multicentric and multifocal disease 1. Younger women 2. Oncogenic HPV infection common 3. Cigarette smoking 4. Immunosuppression Differentiated VIN 1. Unproven but likely precursor to most vulvar SCC 2. Unicentric and unifocal disease . 3. A lesion may appear as an ulcer, warty papule, or hyperkeratotic plaque 1. Older postmenopausal women 2. Oncogenic HPV infection uncommon 3. Associated with vulvar dermatoses such as lichen sclerosus or LSC Vulvar squamous intraepithelial lesions
- 67. Diagnosis No screening strategies are available for vulvar HSIL detection VIN may be asymptomatic Symptoms Itching Burning Pain Clinially significant vulvar HSIL lesions are often visible without the aid of special techniques Vulvar biopsy Suspicious focal vulvar lesions Ulceration, surrounding induration, or inguinal adenopathy raises suspicion for invasive cancer
- 68. Extensive perineal and perianal extension of vulvar HSIL
- 69. Bulky lesion of differentiated VIN
- 70. Vulvoscopy It is microscopic examination of the vulva Selection of the best location for biopsy is usually aided by magnification with a colposcope Apply 3-5% acetic acid soaked gauze pad for 5 minutes o Acetic acid accentuates surface topography and may reveal acetowhite lesions not seen grossly The most abnormal-appearing areas are biopsied Careful documentation, mapping of vulvar biopsy sites, and photographs can aid future management
- 71. Management Objectives Excluding and preventing invasive disease Preserving vulvar appearance and function Improving patient symptoms Vulvar LSIL Self-limited and is not treated unless symptomatic Vulvar HSIL 87% of untreated high-grade VIN patients progresses to vulvar cancer, whereas only 3.8% of treated patients progresses to invasive cancer All vulvar HSIL must be treated 1. Laser ablation It requires full epithelial thickness cellular destruction 2. Wide local excision (WLE) With a gross surgical margin of 0.5 to 1 cm of normal tissue is preferred for large lesions 3. Cavitational ultrasonic surgical aspiration (CUSA) 4. Topical therapy It can be considered if there is no concern for invasive cancer
- 72. Prognosis and prevention Recurrence rates up to 50% are common Multifocal disease Immunocompromised status Prevention HPV vaccination Smoking cessation and improving compromised immune status Treat vulvar dermatosis Indefinite surveillance for multifocal LAGT disease is recommended
- 73. Vulvar cancer It constitutes only 6 % of all gynecologic malignancies Vulvar squamous neoplasia arise predominantly along the Hart line Approximately 90% of vulvar cancers are SCC Malignant melanoma is the second most common Vulvar cancer may involve any of the external vulvar structures Mons pubis Labia majora and minora Clitoris Vestibule Vestibular bulbs Bartholin glands Paraurethral glands Urethral and vaginal openings
- 74. Risk factors Age The average age at diagnosis is 65 years HPV infection 50 to 75 % of invasive vulvar cancers are associated with high risk HPV serotype HPV become a stronger contributor when combined with other cofactors Smoking-35 fold greater risk HSV infection Vulvar intraepithelial neoplasia (VIN) Approximately 4% of women with a history of high grade VIN subsequently develop vulvar cancer Chronic immunosuppression HIV Transplant patients Lichen sclerosus Affected keratinocytes show a proliferative phenotype
- 75. Diagnosis History and physical examination Women commonly present with pruritus and visible lesion They may also have pain, bleeding ,ulceration and inguinal mass Evaluate the entire vulva and perineal skin systematically Measure the primary tumor Evaluate cancer extension into other genitourinary compartments, the anal canal, the bony pelvis and inguinal lymph nodes Histopathology Specimen taken with a keyes punch should be approximately 4mm thick to include the surface epithelial lesion and the underlying stroma This permits evaluation for depth of invasion Imaging Abdomen, chest and pelvis CT MRI PET
- 76. Vulvar biopsy steps 1. A Keyes punch biopsy is placed against the biopsy site and gentle downward pressure is exerted as the punch is rotated 2. A core biopsy is created that extends through the epidermis and into the dermis 3. The tip of a fine needle is used to elevate the core, while fine scissors incise its base
- 77. Management Surgery Surgery is often an integral part of vulvar cancer treatment Wide local excision Vulvectomy Inguinofemoral lymphadenectomy Neoadjuvant chemoradiation Surveillance
- 78. Disease of the vagina Developmental disorders Imperforate hymen Vaginal agenesis Transverse vaginal septum Infectious inflammatory disorders Vaginitis Candidiasis Bacterial vaginosis Trichomonas vaginalis Acquired immunodeficiency syndrome Group B streptococcus Actinomycetes Tuberculosis Noninfectious inflammatory diseases Crohn disease Lesions that follow trauma, surgery, and radiation Atrophic vaginitis Vaginal prolapse Fallopian tube prolapse
- 80. Imperforate hymen… Failure of the inferior end of the vaginal plate to canalize Incidence: 1 in 1000 to 2000 females Clinical features 1. In neonatal period o Hydro/mucocolpos Most cases are asymptomatic Bulging translucent yellow-gray mass It resolves as estrogen levels decline 2. Adolescents after menarche o Hematocolpos,hematometra and hematosalpinx The vaginal canal greatly distends, and the cervix may dilate with cyclic menstruation Cyclic pain, amenorrhea, abdominal pain, and difficulty with urination or defecation The trapped menstrual blood creates a bluish bulge at the introitus Treatment Many advocate repair either in infancy or after thelarche, but before menarche o Presence of estrogen improves tissue healing o Avoids formation of hematocolpometra Hymenectomy o Cruciate incision is made anteroposteriorly from 10 to 4 and from 2 to 8 o'clock positions o The hymenal leaflet are excised and then over sewn with interrupted stitches using 3-0 or 4-0 vicryl or chromic suture o The vagina is copiously irrigated with sterile saline solution o Local wound care includes twice-daily sitz baths o Assess patency of introitus and healing 1-2 weeks after surgery
- 81. The hymenal leaflet are excised and then over sewn with interrupted stitches using 3-0 or 4-0 vicryl or chromic suture
- 82. Hymenectomy The indication for hymenectomy may include complain of amenorrhea, pain, abdominal mass, and urinary and defecation dysfunction Hymen Incision To avoid injury to the urethra anteriorly and to the rectum posteriorly, the surgeon avoids creating pure vertical and horizontal incisions. Instead, a cruciate incision is made anteroposteriorly from 10 to 4 and from 2 to 8 o'clock into the hymeneal membrane Hymenal leaflet trimming
- 83. Transverse vaginal septum It results when there is failure of fusion and/or canalization of the urogenital sinus and mullerian ducts Incidence 1 in 70,000 females It can develop at any level within the vagina Approximately 46 % are found in the upper vagina, 35 to 40 % in the middle portion, and 15 to 20% in the lower vagina
- 84. Transverse vaginal septum… Diagnosis: Patients usually present with symptoms similar to those of imperforate hymen Symptoms and signs o Primary amenorrhea and pelvic pain o Abdominal or pelvic mass o Foreshortened vagina and inability to identify the cervix Imaging o Sonography or MRI confirms the diagnosis o MRI It is most helpful prior to surgery to determine the septal thickness and depth It also help to differentiate a high vaginal septum from cervical agenesis
- 85. Management Antibiotic prophylaxis is usually administered Vaginal septum excision is best performed in a post pubertal adolescent or young adult Thin septum Excision followed by end-to end anastomosis Thick septum Excision followed by skin or buccal mucosal grafts Intercourse is delayed for 6 weeks post surgery Mold advice Soft stent for 7 days Plastic dilator for 12 weeks Intercourse at least twice each week
- 86. Vaginal septum excision • Enema bowel preparation aids rectal decompression to permit greater vaginal traction for visualization • The septum is then incised transversely at its center to avoid laceration of the urethra, bladder, or rectum. • A finger is placed through the transverse incision and is centered cephalad to delineate the upper vaginal wall and the circumferential margins of the septum • Once the septum's perimeter and thickness is defined, the initial transverse incision is extended laterally to the vaginal wall margins. The septum is widely excised circumferentially along its base to minimize postoperative stricture • Others surgeons prefer to create cruciate incisions similar to those with hymenectomy • The four wedges are then trimmed close to the vaginal wall If the septum was thin, a simple circumferential ring of interrupted stitches is constructed using 2-0 gauge delayed-absorbable suture to reapproximate vaginal mucosal edges
- 87. Atrophic vaginitis Physiologic events in postmenopausal women Reflect estrogen deprivation o Atrophy of the squamous epithelium of the vagina A minor trauma may facilitate a transition from simple atrophy to atrophic vaginitis o A loss of glycogen and an increase in pH o A change in the vaginal flora Reduction in the lactobacilli Symptoms Many patients are asymptomatic There may be minor vaginal bleeding, pruritus, dysuria, or dyspareunia Physical examination A pale-appearing mucosa, with petechiae and loss of rugal folds Treatment There usually is a good response to estrogen replacement Antibiotic therapy rarely is necessary
- 88. Vaginal agenesis Lack of the lower portion of the vagina with otherwise normal pubertal maturation and external genitalia The urogenital sinus fails to contribute its expected caudal portion of the vagina As a result, the lower portion of the vagina, usually one-fifth to one-third of the total length, is replaced by 2 to 3 cm of fibrous tissue It does not often become apparent until menarche
- 89. Vaginal Agenesis… Symptoms Cyclic pelvic pain due to hematocolpos or hematometra Physical examination The hymeneal ring is normal, and no bulging membrane is seen Proximal to the ring, only a vaginal dimple or small pouch is found A rectoabdominal examination confirms midline organs Imaging Sonography or MRI will display upper reproductive tract organs MRI is the most accurate diagnostic tool o Length of the atresia o Amount of upper vaginal dilation o Presence of a cervix A cervix in such cases distinguishes vaginal atresia from mullerian agenesis Treatment follows that for mullerian agenesis
- 90. Vaginal cysts and neoplasms Squamous inclusion cyst Cysts of the vagina are relatively uncommon Gartner’s duct cysts Mullerian cyst Benign neoplasms Squamous papilloma Condyloma acuminatum Müllerian papilloma Leiomyoma Rhabdomyoma Malignant neoplasms Vaginal intraepithelial neoplasia Vaginal cancer Primary vaginal cancer is rare, constituting only 1%–2% of all female genital tract malignancies and only 10% of all vaginal malignant neoplasms
- 91. Gartner duct cyst It is derived from remnants of the mesonephric (Wolffian) ducts They are typically asymptomatic Symptoms Dyspareunia Vaginal pain, and Difficulty inserting tampons Physical examination Reveals a tense cyst that is palpable or seen to bulge beneath the vaginal wall They are thin walled, translucent, and contain clear fluid They are most often located along the anterolateral wall of the vagina Observation is reasonable in most cases Marsupialization or excision may be appropriate for symptomatic Gartner duct cysts
- 92. Benign disease of the cervix Cervicitis Noninfectious cervicitis Infectious cervicitis Benign tumors Endocervical polyps Mesodermal stromal polyp Cysts Nabothian cyst Inclusion cyst
- 93. Endocervical polyp These lesions represent overgrowths of benign endocervical stroma covered by mucinous columnar epithelium They typically appear as single, red, smooth, elongated masses extending from the endocervical canal It is found more frequently in multiparas They are usually asymptomatic, but they can cause intermenstrual or postcoital bleeding or symptomatic vaginal discharge Many of them are identified by visual inspection during pelvic examination They are typically benign, and premalignant or malignant transformation develops in less than 1 % Most recommend removal and histologic evaluation of all polypoid lesions
- 94. Nabothian Cyst • Nabothian cysts are the most common type of cyst of the cervix and develop within the transformation zone secondary to squamous metaplasia covering over and obstructing endocervical glands. Grossly, these lesions appear as yellow white cysts that are frequently multiple and can measure up to 1.5 cm in diameter. Microscopically, they are lined by a somewhat flattened, single layer of mucin-producing endocervical epithelium (Fig. 50). In some cases, squamous metaplasia of the lining epithelium occurs. The lining epithelium is almost always at least focally positive with mucicarimine stains allowing these lesions to be distinguished from
- 95. Cervical Stenosis This narrowing of the cervical canal or opening may be congenital or acquired. Diagnosis is based on symptoms and physical findings Symptoms of stenosis in menstruating women include dysmenorrhea, amenorrhea and infertility Postmenopausal women are usually asymptomatic until fluid, exudates, or blood accumulates behind the obstruction If the obstruction is complete, a soft, enlarged uterus from trapped intracavitary fluid is sometimes palpable An inability to introduce a dilator into the endocervical canal is generally considered diagnostic Cervical stenosis is relived by introduction of dilators Preprocedural misoprostol may aid by softening the cervix In postmenopausal women, pretreatment for several weeks with vaginal estrogen cream may also assist dilation.
- 96. Precancerous and cancerous lesions of the cervix
- 102. Preinvasive Lesions of the Lower Genital Tract
- 103. Introduction • The introduction of Pap test has reduced the incidence and mortality rate from invasive cervical cancer by more than 70 percent
- 104. Terminology and histology of cervical intraepithelial neoplasia LAST: lower anogenital squamous terminology; LSIL: low-grade squamous intraepithelial lesions; HSIL: high-grade squamous intraepithelial lesions; CIN: cervical intraepithelial neoplasia. * CIN 2 that is p16-positive is classified as HSIL. CIN 2 that is p16-negative is classified as LSIL. Squamous neoplasia of the vagina, vulva, perianal,and anal squamous epithelia (VaIN, VIN, PAIN, and AIN, respectively) are graded similarly with the caveat that VIN 1 is no longer recognized
- 105. Anatomic considerations External Genitalia o Micropapillomatosis labialis Minute epithelial projections on the inner labia minora Uniform in size and shape and arise singly from their base attachments Often shows spontaneous regression, and treatment is not indicated o HPV lesions Multifocal and asymmetric, and to have multiple papillations arising from a single base
- 106. SCJ everts outward on to ectocervix SCJ regresses into endocervical canal Adolescence Squamous metaplasia Pregnancy Menopause COC use Prolonged lactation Cervix Squamocolumnar Junction • The original squamocolumnar junction (SCJ) marks the terminal site of the upward migration of squamous epithelium during embryonic development • When visible on the ectocervix, the SCJ is a pink, smooth squamous epithelium juxtaposed against the red, velvety columnar epithelium surrounding the external cervical os • The location of the SCJ varies with age and hormonal status Long term pop use
- 107. Squamous Metaplasia the normal replacement of columnar by squamous epithelium on the cervix Squamous metaplasia is most active during adolescence and pregnancy This normal process creates a progressively widening band of metaplastic and maturing squamous epithelium, termed the transformation zone ( Z), between the congenital (original) columnar epithelium and the squamous epithelium
- 108. Transformation Zone and Cervical Neoplasia • The transformation zone consists of the band of squamous metaplasia lying between the original SCJ and new (current) SCJ • Nearly all cervical neoplasia, both squamous and columnar, develops within the Z, usually adjacent to the new or current SCJ
- 109. Human papillomavirus • HPV primarily infects squamous or metaplastic epithelial cells. • Intact virus is shed during normal desquamation of superficial squames. • Late genes are not strongly expressed in high-grade neoplastic lesions • Completion of the viral life cycle takes place only within an intact, fully differentiating squamous epithelium. • HPV is a nonlytic virus, and therefore infectiousness depends on normal desquamation of infected epithelial cells.
- 111. L1 and L2 are two “late” genes of the human papillomavirus (HPV) genome. These genes encode proteins responsible for which of the following? a. Capsid construction b. Regulatory functions c. DNA synthesis and replication d. Conformational changes aiding entry into the host cell
- 112. HPV16,18,31 ,33,35,45,58 • 95% of cervical ca HPV 6,11 • Genital wart • laryngeal papillomas HPV TYPES High risk (HR) Low risk HPV 16 is the most oncogenic type 45% of CIN3 55% of cervical ca Anogenital and oropharyngeal ca HPV 18 13% of SCC 40% of adenocarcinoma HPV 16 and 18 70% of cervical ca 68 % of SCC 85% of Adenocarcinoma HPV 45 3rd most common type for cervical ca HR HPV infection does not cause neoplasia in most infected women, and additional host, viral, and environmental factors determine progression to LG neoplasia Genital HPV Infection=It is the most common STD(USA)
- 114. Clinically, human papillomavirus (HPV) types are classified as high risk (HR) or low risk (LR) based upon their oncogenic potential. Which two HR HPV types together account for approximately 70 percent of cervical cancers worldwide? a. 6 and 11 b. 11 and 45 c. 16 and 18 d. 18 and 31
- 115. Transmission Risk factors the number of sexual partners Both life time and recent early coitarche Cervical HR HPV infection generally requires penetrative intercourse All women who are sexually active should undergo cervical cancer screening regardless of sexual orientation Infection with HPV, predominantly HR types, is very common soon after initiation of sexual activity
- 116. Transmission… Genital warts that develop in children after infancy(1-3years) o Possibilities are: Sexual abuse Nonsexual contact Autoinoculation Fomite transfer Congenital HPV infection from vertical transmission beyond transient skin colonization is rare Infection is not linked to maternal genital warts or route of delivery Indication for cesarean delivery :Large genital wart that may obstruct delivery or Avulse and bleed
- 117. Infection Outcomes Most infections are subclinical. Spontaneous resolution is the most common outcome. Neoplasia is the least common manifestation of HPV infection, developing as the result of persistent infection with integration of HPV DNA The natural history of genital HPV infection varies between individuals and over time Latent infection refers to that in which cells are infected, but HPV remains quiescent Productive infections are characterized by viral life-cycle completion and plentiful production of infectious viral particles Subclinical infections may be indirectly identified as low- grade cytologic, colposcopic, or histologic abnormalities
- 118. HPV Infection Diagnosis • HPV infection is suspected based on clinical lesions or results of cytology, histology, and colposcopy, all of which are subjective and often inaccurate. • Moreover, serology is unreliable and cannot distinguish past from current infection • culture of HPV is not feasible • Thus, diagnosis is confirmed only by the direct detection of HPV nucleic acids by methods that include in situ hybridization, nucleic acid amplication testing (NAA ), polymerase chain reaction (PCR),or others • Tests are not indicated or useful for routine STD screening • Appropriate clinical uses or HR HPV testing include: cotesting with cervical cytology screening in women aged 30 years or older, triage or surveillance of certain abnormal cytology results and untreated CIN, and posttreatment surveillance • One HR HPV test (cobas HPV test) was recently FDA approved as a stand-alone screening test for cervical cancer for women 25 years of age and older
- 119. Infection Treatment • The indications to treat HPV-related LG disease are symptomatic warts, high-grade neoplasia, or invasive cancer. • Treatment of cervical LSIL (HPV changes or CIN 1) is not necessary and is considered only after observation for at least 2 years. • Mechanical removal or destruction, topical immunomodulators, and chemical or thermal coagulation can be used • Examination of a male partner does not benefit a female partner either by in influencing reinfection or by altering the clinical course or treatment outcome or genital warts for LG neoplasia
- 120. Infection Prevention Behavior • Sexual abstinence, delaying coitarche, and limiting the number of sexual partners are logical strategies to avoid genital HPV infection and its adverse effects. Vaccines • Prophylactic vaccines elicit type-specific humoral antibody production that prevents new HPV infection by blocking its entry into host cells • They do not prevent transient HPV positivity or resolve preexistent infection • HPV vaccines have the potential to prevent malignancies at least six body sites that include cervix, vulva, vagina, penis, anal canal, and oropharynx
- 121. Vaccines • There are three HPV vaccines (FDA approved) • All three vaccines contain adjuvants that boost the immune response to vaccine antigens. • Testing for HPV is not recommended prior to vaccination • ACIP target group:Girls aged 11 to 12 years (as early as age 9 years) Vaccine type HPV type covered Remark % of Cx prevented Cervarix (HPV2) HPV 16,18 bivalent vaccine Gardasil (HPV4) HPV 6, 11, 16, and 18 quadrivalent vaccine 65 Gardasil 9 (HPV9) 6,11,16,18, 31, 33, 45, 52, and 58 nonavalent vaccine 80
- 122. HPV vaccine • They are administered in three intramuscular doses during a 6-month period. • Specifically, the second dose is given 1 to 2 months after the first dose, and the third dose is given 6 months after the first dose. • Immune compromised women are candidates to receive the vaccine • All three vaccines show nearly 100-percent efficacy in preventing incident infection and high-grade cervical neoplasia from HPV types included in the vaccines • HPV4 and HPV9 are approved for genital wart prevention in both males and females • HPV vaccines are highly immunogenic with maintenance of protection for at least 5 to 8 years after vaccination • No evidence supports the need for later booster dosing • Because HPV vaccines prevent most, but not all, HPV related cervical cancers, cervical cancer screening should continue per current guidelines
- 123. • Catch-up vaccination is also recommended for all 13- to 26-year-old persons • ACOG recommends shared decision-making with persons aged 27 to 45 years who have not previously received the HPV vaccine and are at risk of acquiring HPV. • IfHPV vaccination is initiated before age 15 years, only 2 doses are needed. This is because the vaccine is more immunogenic at an earlier age. The second dose is given 6 to 12 months following the first
- 124. • HPVvaccines have excellent safety profiles, are well-tolerated, and can be administered along with other recommended vaccinations. Injection- site erythema, pain, and sweling are common. These can increase in severity following subsequent doses but are usually mild to moderate. HPV vaccination is avoided during pregnancy, but pregnancy testing is not recommended prior to administration (American College of Obstetricians and Gynecologists, 2017). If inadvertently given during pregnancy, no action is needed. Vaccination can be given during lactation. Immunocompromised persons are candidates to receive the vaccine and show high seroconversion rates despite concerns for a blunted immune response. 9vHPV should be given with caution to persons who experienced an allergic reaction to a prior dose, have an allergy to yeast, or have had a recent febrile illness
- 125. CIN • CIN is most strongly related to persistent genital hrHPV infection and aging • Inadequate screening is a strong cervical neoplasia risk factor.
- 126. Natural History • Preinvasive lesions can spontaneously regress, remain stable, or progress • The risk of progression to invasive cancer rises with CIN severity
- 127. CIN diagnosis • Cervical Cytology • HPV testing • Current Cervical Cancer Screening Guidelines • Colposcopy • Biopsy
- 128. Which of the following is true regarding the clinical performance of the Pap test? a. Higher sensitivity than specificity b. Higher specificity than sensitivity c. Equally low sensitivity and specificity d. Equally high sensitivity and specificity
- 129. Cervical cytology oThe preventive power of Pap testing lies in regular serial screening oThe Papanicolaou (Pap) test Specificity→98% Sensitivity→45-65% Sampling of the transformation zone at the SCJ adds substantial sensitivity of the Pap test
- 130. How can we optimize the pap test? oSchedule to avoid menstruation oPatients should abstain from vaginal intercourse, douching, vaginal tampon use, and intravaginal medicinal or contraceptive creams for a minimum of 24 to 48 hours before tested oTreatment of cervicitis or vaginitis prior to Pap testing is optimal oAdd the following clinical information to pathology requisition forms LNMP Pregnancy or menopausal status Exogenous hormone use Abnormal bleeding, and Prior abnormal Pap test findings IUCD
- 131. Cytology Collection • Three types of plastic devices are commonly used to sample the cervix: the spatula, broom, and endocervical brush (cytobrush) • Wooden collection devices and cotton swabs are no longer recommended due to their inferior collection and release of cells
- 132. Devices 1. Plastic spatula Predominantly samples the ectocervix distal endocervical canal It firmly scrapes the cervical surface while completing at least one full rotation 2. Endocervlcal brush samples the endocervical canal To minimize bleeding, the brush is used after the ectoccrvix has been sampled and is rotated only one-quarter to one-half turn 3. Plastic broom Samples both endo- and ectocervical epithelium simultaneously Five rotations in the same direction are recommended. Broom devices are favored for liquid-based Pap testing.
- 133. HPV Testing Indications • cervical cancer screening • triage of lesser cytologic abnormalities to later repeat testing or immediate colposcopy • surveillance after colposcopy, or surveillance after treatment
- 134. Co-testing o Pap test plus HPV test o Raises the sensitivity of a single screening test for high-grade neoplasia and leads to earlier detection and management of HSIL o It offers a nearly 100-percent negative predictive value for high-grade neoplasia. o Result can be: Both negative • Repeat after 5 years Cytology positive but HPV negative • ??? Cytology negative but HPV positive • Occur in 10% of the cases • co-testing is repeated 12 months later • A reflex test specifically for HPVs 16 and 18 If positive immediate colposcopy recommended
- 135. Primary HPV Testing oHPV testing alone is approximately twice as sensitive (>90%) as a single Pap test and leads to earlier detection of high-grade disease. oTo counter the lower specificity: Genotyping is part of primary HPV screening for cervical disease and allows the triage of women who test positive for HPV 16 or 18 to immediate colposcopy If positive for non HPV 16 and 18→Reflex cytology is proposed • Colposcopy for abnormal cytology oApproved by FDA for primary cervical cancer screening in women aged ≥25 years
- 136. Appropriate clinical uses for high-risk human papillomavirus (HPV) testing include which of the following? a. Surveillance after treatment of cervical neoplasia b. Cotesting (cytology plus HPV testing) as screening for women 30 years or older c. Triage or surveillance of certain abnormal cervical cytology results or untreated cervical intraepithelial neoplasia (CIN) d. All o the above
- 137. Current cervical cancer screening guidelines The choice of screening strategy should be a shared decision by the provider and patient.
- 138. ACS/ASCCP/ASCP/ACOG deem co-testing preferable to cytology alone in women ≥30 years
- 139. Screening Discontinuation • Screening may be stopped at age 65 years in those at average risk for cervical cancer and who have undergone adequate screening, regardless of past or current sexual history. • Adequate screening is defined as three consecutive, negative cytology results or two consecutive, negative co-test results in the prior 10 years, with the most recent result occurring within the past 5 years
- 140. If all Pap tests to date have been negative and performed at recommended intervals, cervical cancer screening discontinuation would be acceptable for which fo the following women? a. A 42-year-old woman with prior hysterectomy for leiomyomas b. A 72-year-old woman in good health with one prior sexual partner and one new sexual partner or 6 months c. A 55-year-old woman with metastatic breast cancer refusing further therapeutic cancer interventions d. All o the above are reasonable candidates or discontinuation o cervical cancer screening.
- 141. Post hysterectomy • All guidelines recommend against Pap test screening for women who have undergone total hysterectomy (cervix removed) for a benign disease indication and who lack a prior high-grade CIN or cervical cancer diagnosis. • Women who have undergone supracervical hysterectomy should continue routine screening. • The American College of Obstetricians and Gynecologists (2018b) recommends Pap testing of the vaginal cuff every 3 years for 20 years after initial posttreatrment surveillance, which is traditionally a schedule of three Pap tests in the first 2 years posthysterectomy
- 142. Immunocompromised Patients • With HIV infection, screening should commence within 1 year of sexual activity onset and no later than age 21 years. • Women aged 21 to 29 years should receive Pap testing at the time of HIV diagnosis • If an initial Pap test result is negative, testing should be repeated 6 or 12 months later and then continued every 12 months. After three consecutive, negative Pap test results, the interval of Pap testing can be extended to 3 years. For women aged ≥30 years, cytology screening can be followed as just described, or cotesting every 3 years can begin. This co- testing interval is shorter than for immune competent women. Cervical cancer screening is continued indefinitely even in those aged 65 years or older who have been adequately screened. • After hysterectomy for benign disease, vaginal cuff cytology is not recommended.
- 143. A 55-year-old patient undergoes a conization procedure for cervical intraepithelial neoplasia (CIN 3)/ carcinoma in situ (CIS). Appropriate postexcision surveillance over the subsequent 2 to 3 years reveals no recurrence. Which of the following screening schedules is most appropriate for her beyond this posttreatment surveillance? a. Discontinue screening b. Annual screening until age 75 then may discontinue c. Routine screening until age 65 then may discontinue d. Routine screening for at least 20 years even if screening extends beyond age 65
- 144. Immunocompromised Patients… • Those with prior high-grade cervical neoplasia or cancer should have annual vaginal cuff cytology
- 145. The Bethesda System • Cervical cytology reporting is standardized by the Bethesda System nomenclature.
- 146. Epithelial Cell Abnormality Management • A cytology report interprets a screening test and does not provide a final diagnosis.
- 147. Atypical Squamous Cells of Undetermined Significance ASC -US Positive Negative Reflex HPV testing Colposcopy Cotest every 3 years No HPV test Repeat cytology in 1 year Risk of CIN 2 or 3 is 5-10% Risk of cancer is 1-2% Rate of HPV positivity is app 50%
- 148. Low-Grade Squamous intraepithelial Lesion. • Colposcopy is generally indicated for LSIL cytology.
- 149. Atypical Squamous Cells, Cannot Exclude HSIL • Colposcopy is indicated regardless of age or HPV test result • If SCJ is not visualized ,do diagnostic excision
- 150. High-Grade Squamous lntraepithelial Lesion. • Colposcopic evaluation is warranted regardless of age or HPV status • If SCJ not visualized ,do diagnostic excision • Altenatively, immediate excision is acceptable in some nonpregnant patients depending on other factors such as age and concerns regarding future pregnancy
- 151. Glandular Cell Abnormalities • Initial evaluation of a cytologic glandular cell abnormality includes colposcopy and endocervical sampling, regardless of HPV status. • It also includes endometrial sampling in patients aged ≥35 years or in younger women with risk factors for endometrial disease • Reflex HPV testing is not recommended for the triage of glandular cytologic abnormalities for fear that a negative result will dissuade appropriate evaluation.
- 152. Carcinoma. • Cytology results suspicious for squamous cell carcinoma or adenocarcinoma are rare and carry the highest risk of invasive cancer. • If initial evaluation fails to reveal invasive cancer, a diagnostic excision procedure is indicated
- 153. Colposcopy • The colposcope provides a bright light source and variable magnification through an optical lens system or high resolution digital imaging. • Sensitivity estimates range between 50 and 80 percent • Colposcopic examination is optimally timed to avoid menses but is not delayed if there is a visible cervical lesion or abnormal bleeding, or if the patient is unlikely to return. • Solutions used during colposcopy are normal saline, 3- to 5-percent acetic acid, and Lugol iodine
- 154. Solutions used • To begin, normal saline helps remove discharge and cervical mucus and allows initial assessment of vascular patterns and surface contours. A green (red-free) light filter adds contrast to aid vascular pattern visualization (Fig. 29-9). Acetic acid 3- to 5-percent solution is mucolytic and exerts its whitening effects, termed acetowhitening, presumably by reversibly denaturing cellular proteins. This causes neoplastic areas to appear denser compared with the normal surrounding epithelium, and lesions assume varying hues of transient whiteness. Lugol iodine solution stains mature, glycogen-rich squamous epithelium a dark purple-brown color in reproductive-aged women with normal serum estrogen levels. Due to incomplete maturation, dysplastic epithelium has a lower glycogen content, fails to fully stain, and appears yellow
- 155. Lesion Grading • With colposcopy, normal squamous epithelium of the cervix appears featureless, pale-pink and smooth. Blood vessels lie below this layer and therefore are not visible or are seen as a fine capillary network • The mucin-secreting columnar epithelium appears red due to its thinness and close proximity of underlying blood vessels. Its villous appearance derives from epithelial peaks and crypts
- 156. Biopsy Ectocervical Biopsy oAll acetowhite lesions and other abnormalities are biopsied using cervical biopsy forceps under direct colposcopic visualization Recomendations encourage biopsy of all acctowhite areas; two to four biopsies of abnormalities are recommended for optimal sensitivity Endocervical Sampling oEndocervical curettage is performed by introducing an endocervical curette 1 to 2 cm into the cervical canal oIndications The SCJ is not fully visualized. The SCJ is fully visualized, but no lesion is identified. Initial evaluation of ASC-H, HSIL, AGC, or AIS cytology test results Tissue from endocervical sampling is always sent separately from ectocervical biopsies for histologic evaluation
- 157. Pregnancy oPregnancy does not alter the natural history of cervical disease oPregnancy is an opportunity to screen patients aged ≥21 years as indicated oWhen colposcopy is indicated, its primary goal during pregnancy is to exclude invasive cancer oColposcopy and biopsy are safe and accurate during pregnancy oEndocervical and endometrial sampling are never performed during pregnancy to avoid amnionic membrane rupture, infection, or other harm to the pregnancy oCIN is reevaluated postpanum since lesion grade frequently changes after delivery and puerperal remodeling
- 158. CERVICAL INTRAEPITHELIAL NEOPLASIA MANAGEMENT • CIN management may be surveillance or treatment • CIN severity, colposcopic findings, age, and reproductive plans play key roles in cervical disease management.
- 159. CIN 1 oHistologic LSIL (HPV changes or CIN 1) oCIN 1 is no longer treated immediately periodic cytology or co-testing. oTreatment is acceptable only if CIN 1 persists for more than 2 years Ablation • Criteria require that the SCJ and all lesions are fully seen during colposcopy and that the endocervical sampling lacks HSIL (CIN 2/3) or ungraded CIN Excision • If the above criteria are not met and treatment is indicated, excision is recommended and ablation is unacceptable
- 160. HSIL: CIN 2 and CIN 3 • Generally, treatment is recommended for CIN 2 or CIN 3 because of the significant malignant potential and the efficacy of treatment to eradicate precancers. • Treatment modalities include either ablation or excision of the entire TZ • Recurrent or persist HSIL after treatment is managed with repeat excision, not ablation • Hysterectomy may be indicated if repeat excision is needed but not anatomically feasible or if high-grade CIN recurs or persists and invasive cancer has been thoroughly excluded • Hysterectomy as primary therapy is unacceptable • For young women, particularly of low parity, with CIN 2 or HSIL (CIN 2/3, not otherwise specified) surveillance or treatment is acceptable, if the SCJ and all lesions are fully seen during colposcopy
- 161. Adenocarcinoma in Situ • Exclusion of coexistent invasive cancer and removal of all affected tissue are primary goals • AIS can be multifocal, lie deep within endocervical crypts, and extend high into the endocervical canal • Thus, diagnostic excision is recommended to exclude invasive cancer with maximum certainty • cold-knife conization is favored over loop electrosurgical excision procedure (LEEP) to get an intact specimen with the most interpretable margins • Ifthe excised specimen shows no invasive cancer, hysterectomy is recommended in women who have completed childbearing
- 162. Postcolposcopy Surveillance without Treatment • When colposcopy following abnormal screening tests fails to diagnose a high-grade precancer or there is spontaneous regression ofhigh- grade CIN in younger women, further surveillance is indicated. • Surveillance involves repeat cytology, HPV testing, or colposcopy alone or in combination at specific intervals depending on the original abnormal cytology result, patient age, and current guidelines. • Exceptions are AGC, favor neoplasia and AIS Pap test results. These are always followed by excision unless invasive cancer is diagnosed during initial colposcopic examination and biopsy
- 163. CERVICAL INTRAEPITHELIAL NEOPLASIA TREATMENT • Current treatment of CIN is limited to ablation or excision procedures targeting the entire TZ • Thus, individual cervical lesions are not treated. Any treatment ideally should reach a depth of 5 to 7 mm from the surface to treat CIN adequately. Surgical treatments have an approximate 90-percent success rate
- 164. Ablation • This involves physical destruction of tissue and is generally effective for noninvasive ectocervical disease • Before ablation, glandular neoplasia or invasive cancer are excluded with the greatest possible certainty. • Ablation should not be used after previous therapy, after glandular cytologic abnormalities, or for AIS • The most commonly used ablative treatment modalities are cryosurgery and carbon dioxide (C02) laser
- 165. Excision • Excision procedures are favored when the risk of invasive cancer is significant • Excision is also indicated for persistence or recurrence ofhigh-grade CIN after treatment • Excisional modalities include LEEP, also known as LLETZ (large loop excision of the transformation zone}; cold-knife conization (CKC); and laser conization.
- 167. Surveillance after Treatment or Regression • Post-treatment surveillance with cytology, HPV testing, and/or colposcopy is required to confirm treatment success • After excision, surveillance will be influenced by margin status. • After treatment for high-grade cervical dysplasia or invasive cancer, screening continues for at least 20 years, even ifscreening extends beyond age 65. • If an excision margin or endocervical curettage performed immediatdy after an excision is positive for HSIL {CIN 2 or CIN 3), repeat excision may be indicated. Repeat excision is indicated for special circumstances such as AIS or microinvasive carcinoma at the excision margins.
- 168. Hysterectomy • Hysterectomy is unacceptable as primary therapy for CIN • However, it may be considered when treating recurrent high-grade cervical disease if childbearing has been completed or if a repeat cervical excision is strongly indicated but not technically feasible. • Hysterectomy is the preferred treatment of AIS, if future fertility is not desired and excision has excluded invasive cancer. Even with negative cervical margins, hysterectomy performed for CIN 2 or worse is not completely protective.
- 169. Cervical Cancer oCervical cancer is the most common gynecologic cancer in women worldwide oWomen have 1 in 132 lifetime risk of developing this cancer oThe median age at diagnosis of cervical cancer is 50 years oHPV is the primary etiologic infectious agent associated with cervical cancer 99.7 percent of cervical cancers are associated with an oncogenic HPV subtype
- 170. Risk factors o Lack of regular cervical screening o HPV infection o Lower education attainment,older age,neighborhood poverty Related to lower rate of cervical screening o Cigarette smoking 2-3 fold increased risk for HSIL or invasive cancer Reduced clearance of hr HPV infection Modify viral oncoprotein expression o Parity 7-four fold 1 or 2-two fold oLong term COC use o HPV positive +COC user-4 fold o Relative risk decrease after 10 years of cessation oMultiple sexual partner > 6 life time sexual partner oEarly coitarche Before 20 years oImmunosupression Cervical ca is AIDS defining illness Transplant recipients on azathioprine
- 171. PATHOPHYSIOLOGY o Tumorigenesis Unlike low-risk serotypes, oncogenic HPV serotypes can integrate into human DNA Amplification of viral replication and subsequent transformation of normal cells into tumor cells may follow E7 oncoprotein binds to the retinoblastoma (Rb) tumor suppressor protein, whereas E6 binds to the p53 tumor suppressor protein • In both instances, binding leads to degradation of these suppressor proteins. • The E6 effect of p53 degradation is well studied and linked with the proliferation and immortalization of cervical cells
- 172. Spectrum of cervical dysplasia • A. This initial point shows the cell at risk due to active HPV infection. The HPV genome (blue ring) exists as a plasmid, separate from the host DNA. • B. The clinically relevant preinvasive lesion, cervical intraepithelial neoplasia 3 (CIN 3) or carcinoma in situ (CIS), is an intermediate stage in cervical cancer development. The HPV genome has become integrated into the host DNA, resulting in increased proliferative ability. • C. Interactive effects between environmental insults, host immunity, and somatic cell genomic variations lead to invasive cervical cancer
- 173. Tumor Spread Lymphatic Spread o The cervix has a rich network of lymphatics, which follow the course of the uterine artery o The pattern of tumor spread typically follows cervical lymphatic drainage o In contrast, lymphatic channels from the posterior cervix course through the rectal pillars and the uterosacral ligaments to the rectal lymph nodes. Lymph Node Groups Paracervical and parametrial lymph node Obtrator lymph node Paraaortic lymph node Internal,external and common iliac lymph nodes
- 174. Lymphatic drainage of the cervix The parametrial lymph nodes are removed during radical hysterectomy. Pelvic and paraaortic nodes also may be removed by lymphadenectomy
- 175. Lymphovascular Space Involvement • LVSI is poor prognostic indicator but not included in the clinical staging of cervical cancer
- 176. Local and Distant Tumor Extension • With extension through the parametria to the pelvic sidewall, ureteral blockage frequently develops, resulting in hydronephrosis • Additionally the bladder may be invaded by direct tumor extension through the vesicouterine ligaments (bladder pillars). The rectum is invaded less often because it is anatomically separated from cervix by the posterior cul-de-sac. Distant metastasis results from hematogenous dissemination, and the lungs, ovaries, liver, and bone are the most frequently affected.
- 177. HISTOLOGIC TYPES o Squamous cell carcinomas represent 70% of all cervical cancer, and adenocarcinomas account for 25% of cervical cancers. o The other cell types are rare o SCC-arise from the ectocervix o Adenocarcinoma-arise from the endocervical mucus-producing columnar cells. o Mucinous adenocarcinomas are the most common o Endometeroidadenocarcinomas are the second most frequently identified and display glands resembling those of the endometrium o Women with Peutz-Jegher syndrome are at higher risk of developing adenoma malignum(Minimal deviation) contain a greater number of glands positioned at a deeper level than normal endocervical glands.
- 178. Prognosis Comparison • Women with adenocarcinomas have worse overall survival rates at every stage compared with those with squamous cell carcinoma(FIGO) Other Tumor Types oThe following has poor prognosis Neuroendocrine tumors of the cervix are highly aggressive Cervical sarcoma • leiomyosarcomas • stromal sarcomas Melanomas
- 179. DIAGNOSIS Symptoms • Some women diagnosed with this cancer are asymptomatic. In others, early-stage cervical cancer may create a watery, blood-tinged vaginal discharge. Intermittent vaginal bleeding that follows coitus or douching also can be noted. As a malignancy enlarges, bleeding typically intensifies, and occasionally, a woman presents with uncontrolled hemorrhage from a tumor bed
- 180. Physical examination o Most have normal general physical examination o External genitalia and vaginal examination o Inspect anogenital area o Speculum examination o Bimanual examination The proximal posterior vaginal wall is most commonly involved o Rectovaginal examination Thick hard irregular rectovaginal septum oDigital rectal examination Appreciate the parametrial,uterosacral and pelvic side wall involvement Thick irregular firm and less mobile A fixed mass indicates that tumor has poorly extended to the pelvic side walls • Lower extremity edema • Low back pain radiating to legs • Hydronephrosis oLymphatic tumor spread to supraclavicular and inguinal lymphadenopathy oHematuria or Vesicovaginal or rectovaginal fistula
- 181. Papanicolaou Test and Cervical Biopsy oHistologic evaluation of cervical biopsy is the primary tool to diagnose cervical cancer oPap testing alone for evaluation of a suspicious lesion is discouraged Due to low single test sensitivity(53-80%) • Thus, the preventive power of Pap testing lies in regular serial screening Take biopsy for diagnosis • Biopsies are taken from the tumor periphery and include underlying stroma oCervical punch biopsies or conization specimens are the most accurate for allowing assessment of cervical cancer invasion
- 182. STAGING o Historically, cervical cancer has been staged clinically. o The current staging system now incorporates radiologic and surgical evaluation Lymph node metastases worsen patient prognosis and may be identified with imaging. o early-stage disease refers to FIGO stages I through IIA. o The term advanced-stage disease describes stages IIB and higher o Accurate evaluation is critical to appropriate treatment planning
- 185. Which of the following tests is NOT used for staging cervical cancer per the International Federation of Gynecology and Obstetrics (FIGO)? a. Cystoscopy b. Chest radiograph c. Intravenous pyelogram d. Computed tomography scan
- 186. Imaging • Imaging results can tailor treatment for an individual.
- 187. MRI • Measures tumor size, delineates cervical tumor boundaries, and identifies surrounding bladder, rectal, or parametrial invasion. • Offers superior contrast resolution at soft tissue interface • Less accurate for diagnosing microscopic or deep cervical stromal invasion or identifying minimal parametrial extension • For primary cervical cancer, MR imaging is superior to CT for determining carcinoma size, local tumor extension, and lymph node involvement
- 188. Computed Tomography • for the assessment of nodal involvement and distant metastatic disease • CT can also aid detection of ureteral obstruction • CT is not accurate for assessing subtle parametrial invasion or deep cervical stromal invasion • CT is also limited by its inability to detect small volume metastatic involvement in normal-size lymph nodes.
- 189. Positron Emission Tomography • Enable an imaging of functional processes within the body • FDG-PET is superior to CT or MR imaging for lymph node metastasis identification • However, PET is insensitive for lymphatic metastasis <5 mm
- 190. LYMPH NODE DISSECTION • It offers accurate metastasis detection and may modify a patient's primary treatment strategy • Potential candidates include patients with positive or suspected positive pelvic nodes undergoing chemoradiation treatment • During lymphadenectomy, most experts recommend lymph node dissection in the common iliac and paraaortic region and resection of macroscopic lymph nodes
- 191. PROGNOSIS • FIGO stage is the most significant prognostic factor • Lymph node involvement is an important prognostic feature • In addition, the number of nodal metastases is predictive • In general, microscopic nodal involvement has a better prognosis than macroscopic nodal disease
- 192. EARLY-STAGE PRIMARY DISEASE TREATMENT • Early stage disease includes stage I to IIA • Stage IA is a microinvasive cervical cancer that carries a minor risk of lymph node involvement and excellent prognosis following treatment.
- 193. Stage IA1 oRisk of nodal metastasis-1.5% oOption of treatment Cervical conization Total extrafascial hysterectomy (type I hysterectomy) is preferred for women who have completed childbearing oWhen LVSI present in Stage IA1,the risk of lymph node metastasis is app 5% Modified radical hysterectomy (type II hysterectomy) and pelvic lymphadenectomy. Radical trachelectomy with pelvic lymph node dissection can be considered in those patients desiring fertility preservation
- 194. What is the most appropriate treatment for a 30-year old woman who has stage IA1 adenocarcinoma of the cervix, negative lymphovascular space invasion (LVSI), and strongly desires future fertility? a. trachelectomy b. Cold-knife conization c. Extra fascial hysterectomy d. Modifed ( type II) radical hysterectomy
- 195. Stage IA2 o These cancers have a 7-percent risk of lymph node metastasis and carry a >4- percent risk of disease recurrence o Radical (or modified radical) hysterectomy and pevic lymphadenectomy is recommended. o For fertility preservation, stage IA2 squamous cervical lesions may be treated with radical trachelectomy and lymphadenectomy. o A nonabsorbable cerclage may be placed concurrently with radical trachelectomy to improve cervical competence during pregnancy o Preoperative MR imaging to evaluate the parametria and/or CT scan to evaluate extracervical disease is recommended in these cases.
- 196. IA1 and IA2 • Alternatively, patients with stage IAl and IA2 cervical cancer can be treated with intracavitary brachytherapy alone with excellent results • Potential candidates for vaginal brachytherapy include women who are elderly or who are not surgical candidates due to comorbid medical disease
- 198. Which of the following statements about radical trachelectomy is FALSE? a. Cesarean delivery is required if pregnancy achieved. b. Preterm birth rates are increased after radical trachelectomy. c. At least 1 cm of endocervix must remain attached to the uterus. d. If the shave margin is positive, hysterectomy is completed
- 200. Stage 1B to IIA • Stage IB to IIA cancers do not extend into the parametria and thus can be managed with either surgery or chemoradiation • In general, radical hysterectomy for stage IB through IIA tumors is usually selected for premenopausal women who wish to preserve ovarian function and for women who have concerns about altered sexual functioning following radiotherapy. • Age and weight are not contraindications to surgery. • Surgery is contraindicated in patients with severe cardiac or pulmonary disease
- 201. Weighing Surgical and Radiotherapy Complications Early-stage cervical cancer radical surgery • Ureteral stricture • Vaginal fistulas, bladder dysfunction,constipation, wound breakdown, lymphocyst, and lymphedema • VTE Radiation therapy • altered sexual function secondary to a shortened vagina • Dyspareunia • psychologic factors • vaginal stenosis • Late urinary and bowel complications such as fistula formation, enteritis, proctitis, and bowel obstruction
- 202. Positive Pelvic Lymph Nodes • Approximately 15 percent of patients with clinical stage I through IIA cervical cancers will have positive pelvic nodes. oRisk factors for lymph node involvement include Histologic grade Depth of invasion Stromal invasion Parametrial extension LVSI
- 203. Recurrence Risk For women who have completed radical surgery for early- stage cervical cancer, the GOG has defined risk factors to help identify women for tumor recurrence
- 204. ADVANCED-STAGE PRIMARY DISEASE TREATMENT • Radiation Therapy • Both external beam pelvic radiation and brachytherapy are typically delivered • During evaluation, if paraaortic nodal metastases are found, extended field radiation can be added to treat these affected lymph nodes
- 205. Chemoradiation • Chemotherapy given concurrently with radiation therapy significantly improves overall and disease free survival rates in women with cervical cancer • It is now recommended that cisplatin based chemotherapy should be considered in women undergoing radiation for cervical cancer
- 206. Pelvic Exenteration for Primary Disease • Stage IVA without distant spread
- 207. StagelVB • poor prognosis • palliation
- 208. SURVEILLANCE Following Radiotherapy o In general, patients are seen at 3month intervals for 2 years, then every 6 months until 5 years have passed from treatment, and then annually o Vaginal dilator or have vaginal intercourse o Pelvic examination and/or radiologic scanning shrinkage of the mass o Rectovaginal examination Nodularity in the ligaments and parametria o Manual nodal survey neck, supraclavicular, axillary, and inguinal lymph nodes o A cervical or vaginal cuff Pap test also is collected annually for 20 years after treatment completion o Colposcopy ,biopsy ,CT or CT/PET as needed
- 209. SURVEILLANCE … • Following Surgery • After a radical hysterectomy, 80 percent of recurrences are detected within the subsequent 2 years • During patient surveillance, an abnormal pelvic mass or abnormal pelvic examination finding typically prompts CT scanning of the abdomen and pelvis. • Clinical findings include cervical or vaginal lesion, rectovaginal nodularity, pain radiating down the posterior thigh, or new-onset lower extremity edema. Pelvic recurrences after radical hysterectomy, if diagnosed early, can be treated with radiation therapy • The same schedule of visits and Pap tests as outlined above for surveillance following radiotherapy is then recommended
- 210. SURVEILLANCE … • Hormone Therapy • Cervical cancer is not estrogen-dependent and thus hormone therapy is not contraindicated to treat menopausal symptoms • Either systemic or vaginal forms of estrogen are suitable.
- 211. SECONDARY DISEASE • This is defined as either persistent or recurrent cancer • usually palliative Rx • pelvic radiation if not received before • Metastatic cervical cancer is not curable • Pelvic Exenteration for Secondary Disease • Radiotherapy or Chemotherapy for Secondary Disease chemoradiation for radiotherapy naive pts
- 212. PALLIATIVE CARE • Pain management forms the basis of palliation • Many will require narcotics • Treat constipation • Home hospice
- 213. MANAGEMENT DURING PREGNANCY • A greater proportion of patients have stage I disease • A Pap test is recommended for all pregnant patients older than 21 at the initial prenatal visit. • Additionally, clinically suspicious lesions are directly biopsied • If Pap test results reveal HSIL, adenocarcinoma in situ (AIS), or suspected malignancy, colposcopy is performed and biopsies are obtained. • endocervical curettage is excluded to prevent amnionic sac rupture • IfPap testing indicates malignant cells and colposcopy-directed biopsy fails to confirm malignancy, diagnostic conization may be necessary
- 214. Stages I and II Cancer in Pregnancy • Women with positive nodes may elect to be treated with definitive treatment, rather than delay. • Given the outcomes, a planned treatment delay is generally acceptable for women who are 20 or more weeks' gestational age at diagnosis • For patients with stage IA2 through IIAI, a cesarean section via a classical uterine incision may be performed at term, followed immediately by radical hysterectomy and lymph node dissection. Notably, a classical cesarean incision minimizes the risk of cutting through tumor in the lower uterine segment, which can cause serious blood loss and result in tumor spread • (stage IAl) may deliver vaginally and he reevaluated 6 weeks postpartwn
- 215. Advanced Cervical Cancer in Pregnancy • Women with advanced cervical cancer diagnosed prior to fetal viability are offered primary chemoradiation. • Spontaneous abortion of the fetus tends to follow whole-pelvic radiation therapy. • For women who decline pregnancy termination, systemic chemotherapy can be administered. Cisplatin with vincristine or paclitaxel can be administered in pregnancy. • If cancer is diagnosed after fetal viability is reached and a delay until fetal pulmonary maturity is elected, then a classical cesarean delivery is performed. Chemoradiation is administered after uterine involution. • For patients with advanced disease and treatment delay, pregnancy may impair prognosis. A woman who elects to delay treatment, to provide quantifiable benefit to her fetus, will need to accept an undefined risk of disease progression.
- 216. A 29-year-old primigravida at 10 weeks’ gestation has a Pap test result of adenocarcinoma in situ (AIS). Colposcopy and biopsies performed are concerning for invasive adenocarcinoma. What is the best next step? a. Pregnancy termination b. Conization at 6 weeks’ postpartum c. Cesarean radical hysterectomy at term d. Conization early in the second trimester