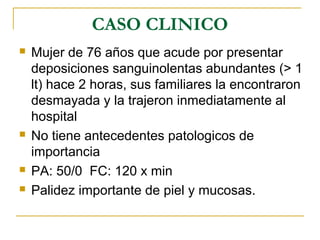
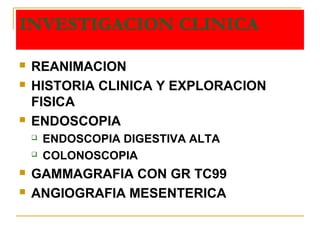
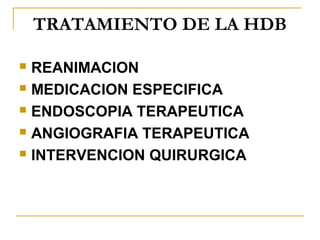
Este documento trata sobre la hemorragia digestiva baja (HDB), definida como sangrado por debajo del ángulo de Treitz. Presenta estadísticas sobre su incidencia y causas más comunes como la diverticulosis y las angiodisplasias. Describe un caso clínico de HDB masiva y los exámenes endoscópicos y de imagen utilizados para diagnosticar la causa subyacente. Finalmente, resume las consideraciones generales y específicas para el tratamiento de la HDB.