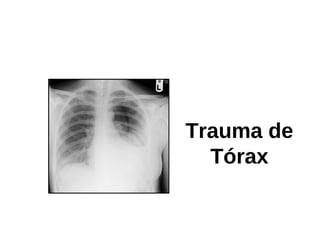
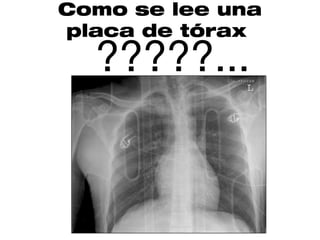
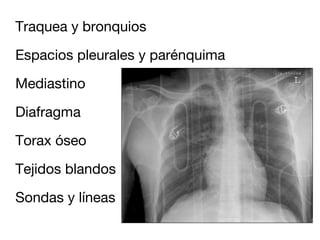
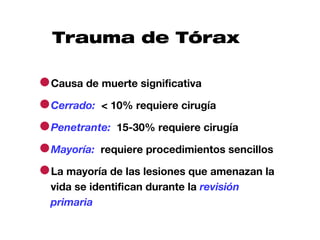
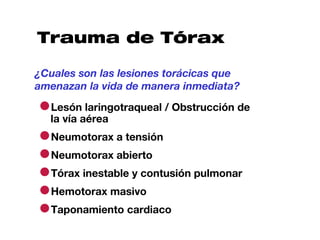
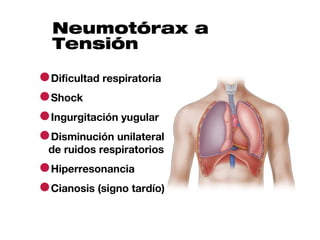
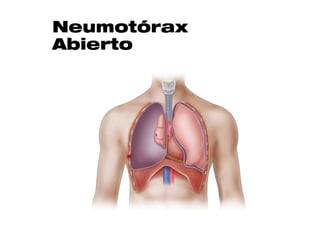
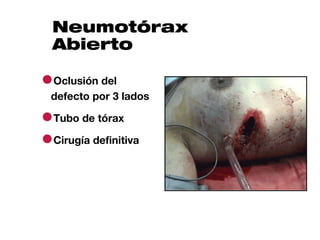
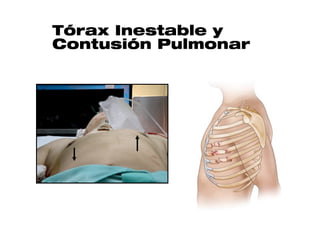
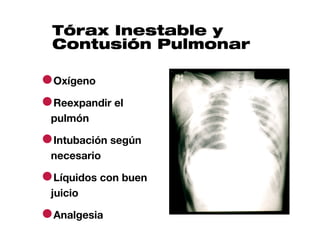
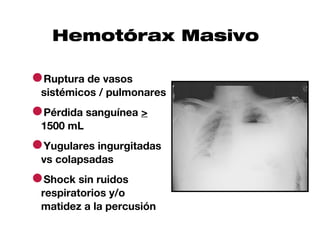
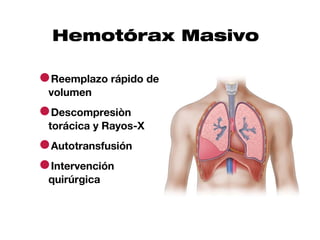
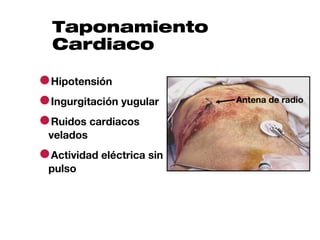
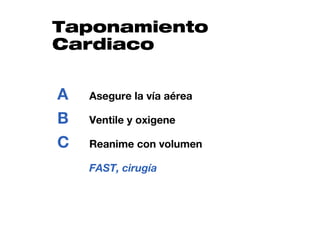
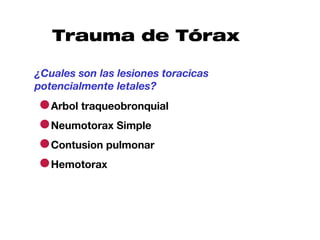
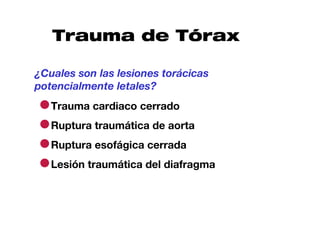
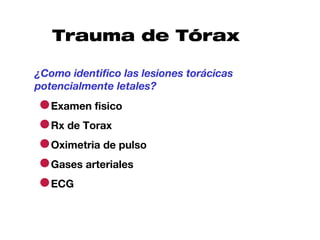
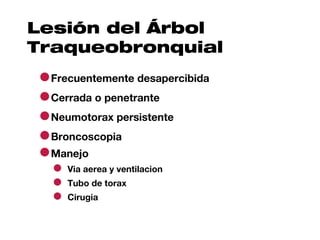
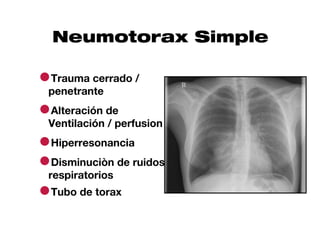
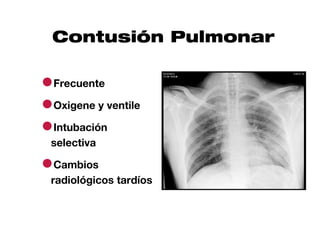
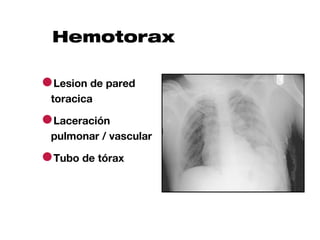
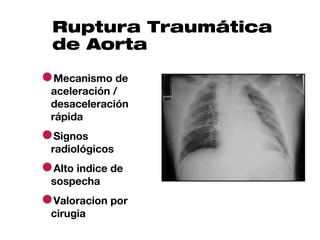
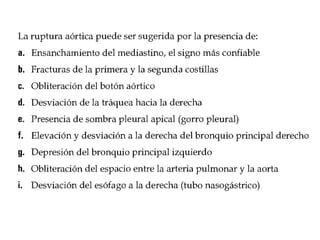
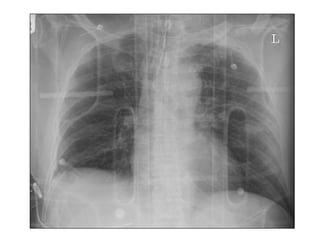
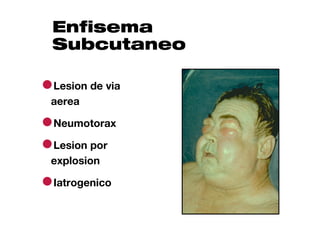
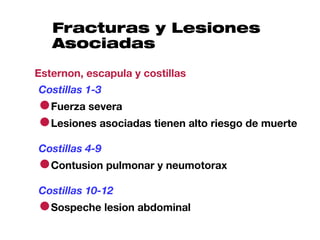
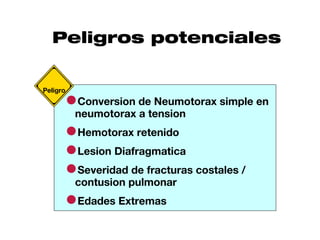
Este documento describe la evaluación y manejo inicial del trauma torácico. Resalta que las lesiones que amenazan la vida como la obstrucción de vía aérea, neumotórax a tensión y hemorragia masiva deben identificarse y tratarse durante la revisión primaria para prevenir complicaciones como hipoxia e hipoperfusión tisular. También destaca que la mayoría de lesiones potencialmente letales como neumotórax simple, contusión pulmonar y hemotorax pueden identificarse con exámen físico, rayos