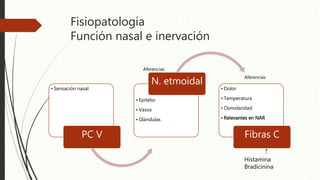
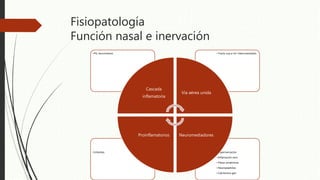
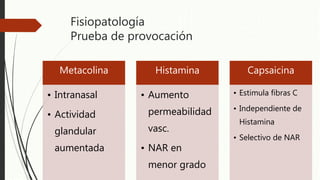
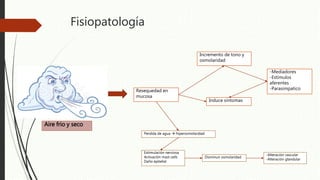
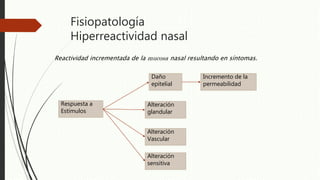
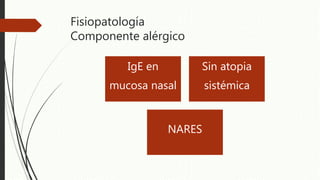
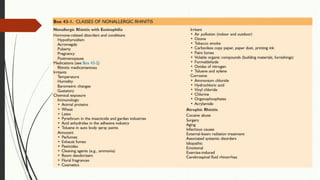
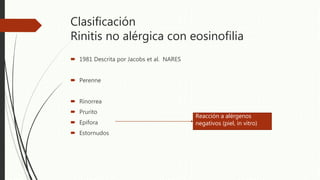
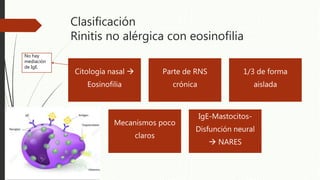
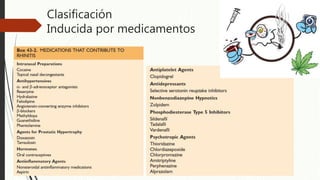
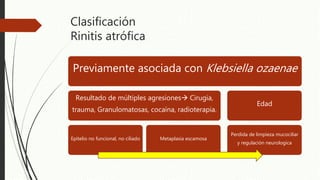
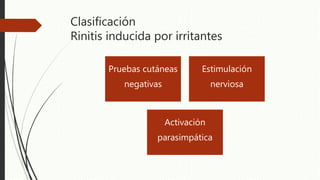
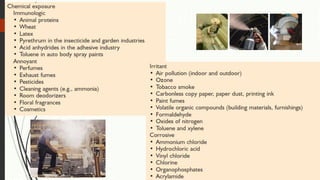
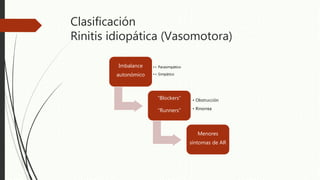
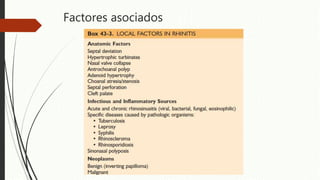
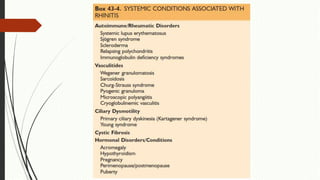
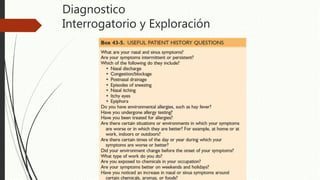
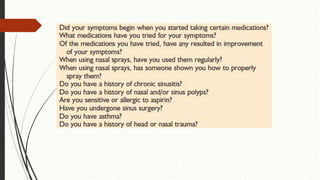
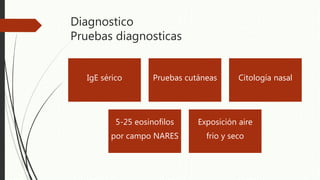
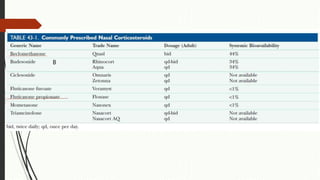
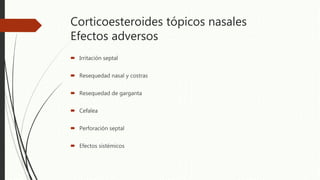
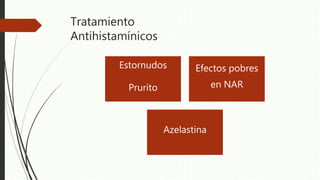
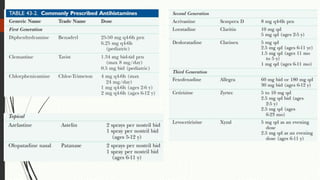
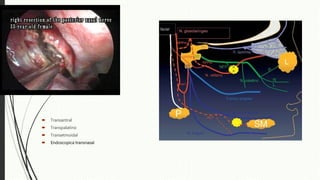
Este documento trata sobre la rinitis no alérgica, clasificándola en varios tipos como la rinitis no alérgica con eosinofilia, rinitis hormonal, rinitis inducida por medicamentos y rinitis atrófica. Explica la fisiopatología de la rinitis no alérgica y los factores asociados. Finalmente, detalla el diagnóstico y tratamiento de esta condición, incluyendo corticoesteroides tópicos nasales, antihistamínicos y cirugía en algunos casos.